-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Obstetrics and Gynecology
p-ISSN: 2326-120X e-ISSN: 2326-1218
2017; 5(2): 24-29
doi:10.5923/j.rog.20170502.02

Comparative Study of Hysteroscopic and Histopathologic Findings in Women Monitored at a High Complexity Hospital
Gentil de Oliveira Paiva Júnior1, Maria Lúcia Neto de Menezes2, Maria das Neves Figueiroa2, Maria da Conceição Farias Souto Maior3, Marcelo Flávio Batista da Silva4, Soraia de Oliveira Pequeno4
1Medical Residency Program of Pernambuco, Brazil
2School of Nursing ‘Nossa Senhora das Graças,’ University of Pernambuco, Brazil
3Catholic University of Pernambuco, Brazil
4Arcoverde Higher Education Autarchy, Brazil
Correspondence to: Maria das Neves Figueiroa, School of Nursing ‘Nossa Senhora das Graças,’ University of Pernambuco, Brazil.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction: The prevalence of problems related to abnormal uterine bleeding and the importance of early diagnosis of neoplasms justify the adoption of alternatives for early diagnosis aiming at measures to reduce mortality. Thus, when endometrial proliferation is suspected, hysteroscopy is the most adequate propaedeutic method to evaluate uterine cavity in women, either asymptomatic or with vaginal bleeding, since it provides direct visualization of diffuse or focal abnormalities within the endometrial cavity. Objective: To investigate the correlation between findings derived from direct visualization of the uterine cavity by hysteroscopy and results of uterine cavity biopsy in women provided with care at a referral hospital for gynecology in Recife city, Pernambuco, Brazil. Methodology: Cross-sectional epidemiological study, with a quantitative and retrospective approach, conducted at the ‘Agamenon Magalhães’ Hospital, in Recife, a referral institution in specialized gynecological care. Data was obtained from the 68 medical reports issued as results of hysteroscopic examination, collected within the period from September 2015 to March 2016. The study has been approved by the Research Ethics Committee of the ‘Agamenon Magalhães’ Hospital. Results: Endometrial thickening caused 36.9% of the hysteroscopic procedures and uterine polyps caused 51.3% of these procedures. The histopathologic reports evidenced the occurrence of endometrial polyps (59%). Analyzing the correlation between hysteroscopy and histopathology showed a concordance of 82.4%. The occurrence of cancer corresponded to 7.35% in the total sample. Among women with cancer, the average age was 62.7 years. Conclusion: The correlation between hysteroscopic findings and sample analysis of the histopathologic study has been considered favorable, thus we may claim that the behavior of methods to support the diagnosis of endometrial pathologies analyzed in this study is effective.
Keywords: Biopsy, Histological techniques, Endometrial neoplasms, Uterine cervix neoplasms, Hysteroscopy
Cite this paper: Gentil de Oliveira Paiva Júnior, Maria Lúcia Neto de Menezes, Maria das Neves Figueiroa, Maria da Conceição Farias Souto Maior, Marcelo Flávio Batista da Silva, Soraia de Oliveira Pequeno, Comparative Study of Hysteroscopic and Histopathologic Findings in Women Monitored at a High Complexity Hospital, Research in Obstetrics and Gynecology, Vol. 5 No. 2, 2017, pp. 24-29. doi: 10.5923/j.rog.20170502.02.
1. Introduction
- Human endometrium is regarded as a hormonally active organism, which undergoes periodic changes that are the basis of the human menstrual cycle. Irregular vaginal bleeding is one of the main reasons why women seek gynecological care. There are several causes of uterine bleeding, which can occur at any age, resulting from problems related to anovulation, benign or malignant anatomical lesions, pregnancy, or hormonal disorders [1].It is estimated that 1.5% of the women with anomalous uterine hemorrhage are diagnosed with endometrial hyperplasia (EH). Hyperplasia without atypia seems to be more frequent (0.5-5%) than hyperplasia with atypia (less than 1%). Endometrial hyperplasia is clinically relevant, because it is often a precursor lesion of endometrial adenocarcinoma. Distinguishing between hyperplasia and true precancerous lesions has a significant clinical effect, since it helps proposing an adequate intervention, in order to avoid deficient or excessive treatment [2].The classification of endometrial proliferative lesions involves the groups named as hyperplasia, endometrial intraepithelial neoplasm (EIN), and carcinoma. Hyperplasias, represent hyperestrogenic conditions, EIN, precursor lesion, and finally carcinoma. Both endometrial hyperplasia and endometrial cancer usually have endometrial thickening. EH is a histological entity characterized by proliferation of endometrial glands [3].Hyperplasia is the normal endometrial response to an estrogenic stimulus. When the stimulus is increased, and above all not compensated by progesterone, an exaggerated growth of the glandular endometrial component occurs. There is an increased gland/stroma ratio and the glands have variable size and shape; the glandular epithelium may or may not have atypia [3].Among the benign changes in the endometrium, polyps emerge as lesions with low malignant potential. Polyp is a clinical term applicable to any sessile or pediculate formation of relief from the implant area in relation to the adjacent surface, regardless of its histological structure. Endometrial polyps totally or partially reproduce an immature endometrium type, with a microscopic structure consisting of glands and stroma. The literature reports that the prevalence of polyps in women with a history of abnormal uterine bleeding ranges from 10 to 30% [4].Endometrial carcinoma is the most common neoplasm, observed in 90% of the cases. In women with postmenopausal metrorrhagia, the prevalence ranges from 3 to 10%, and in this context it is key to exclude such a pathology, especially considering the importance of diagnosis at an early stage and having a favorable prognosis [5].The occurrence of endometrial cancer constitutes a frequent neoplasm among women in the USA, with about 34,000 new cases diagnosed and 6,000 deaths per year [6]. In Brazil, endometrial cancer occupies the fourth place among malignant neoplasms of the female population, and this is the second most frequent pelvic tumor among Brazilian women [7]. The population-based registry of adjusted incidence in Brazil ranges from 2 to 7 new cases per 100,000 women in the cities of São Paulo, Brasília, Cuiabá, and Goiânia.The incidence of endometrial cancer is evidenced within the age group over 50 years, with an average age of diagnosis at 61 years. The incidence in women less than 50 years old is rare. In cases of this cancer type, survival depends on the stage at which the disease is detected. In the initial stage, 5-year survival can reach 80% to 90% of the cases. In later stages, survival is significantly lower. In developed countries, a decrease in the mortality rate has been observed, which is assigned to the fact that disease has been detected earlier [8].When any change in the endometrium is suspected, the clinician should undertake the propaedeutic analysis until the final diagnosis is obtained. In the diagnostic evaluation, when endometrial proliferation is suspected, hysteroscopy is the most adequate propaedeutic method to evaluate the uterine cavity in women, either asymptomatic or with vaginal bleeding, since it provides direct visualization of diffuse or focal abnormalities within the endometrial cavity and cervical canal [7].Nowadays, there is a great diversity of diagnostic techniques available to evaluate pathologies within the uterine cavity, all of them with advantages and limitations. In this group, hysteroscopy constitutes a safe alternative, with low incidence of complications, accurate for diagnosing intrauterine anomalies, thus it is clinically useful to diagnose and exclude pathologies.The development of hysteroscopy allowed a unique evaluation of the uterine cavity, as well as an analysis of functional aspects of endometrium, such as surface, color, glandular distribution, vascularization, thickness, mucus presence or absence, and signs indicating infection or tumors. Hysteroscopy is an examination that allows guided biopsy of suspected areas or lesions, with advantages classically related to the endoscopic approach, such as lower morbidity and mortality, shorter length of hospitalization, and shorter time to restart activities. This allows investigating the cases of abnormal uterine bleeding and infertility, as well as the therapeutic approach to lesions, such as: submucous myomas, polyps, septa, synechiae, diagnosis of pathologies suspected by other methods, localization of foreign bodies within the uterine cavity, diagnosis and monitoring of endometrial hyperplasia, among others [9]. Hysteroscopy was performed for the first time in 1869, reaching its peak of development in 1980, by means of the 4 mm optics, which provided direct visualization of the cavity, making the therapeutic approach to lesions easier [10]. This exam has the advantage of recording the image to obtain a second opinion. However, it is a difficult access procedure for the Brazilian population, which depends on public health services, since few centers resort to this technology.To complement the hysteroscopic results, the collection of material for histopathologic evaluation is recommended, as a strategy for biopsy aimed at the area of greatest suspicion. The hysteroscopic study is a simple, fast, and safe exam, and it has a low incidence of complications. This procedure has been widely used in the investigation of abnormalities within the uterine cavity lately, constituting a method of high diagnostic accuracy, thus it has been regarded as the gold standard for diagnosing endometrial lesions [11].Considering the prevalence of problems related to abnormal uterine bleeding and the importance of early diagnosis of possible neoplastic changes, the main alternatives for reducing mortality are associated clinical examination, hysteroscopy, and biopsy aimed at histopathologic analysis.Histopathologic examination consists in microscopic analysis of tissues to detect possible lesions, in order to inform the clinician about the nature, severity, extent, evolution, and intensity of lesions, as well as to suggest or even confirm the cause of the condition. Histopathologic examination can define proper treatment of the lesion; this technique can also help preserving the tissue architecture needed to correlate the neoplastic tissue type with its biological behavior and response to therapy.Given the above, this study aimed to analyze the correlation between findings resulting from direct visualization of the uterine cavity by hysteroscopy and the results of uterine cavity biopsy in women provided with care at a referral hospital for gynecology in Recife city, Pernambuco, Brazil.
2. Material and Methods
- This is a cross-sectional epidemiological study, with a quantitative and retrospective approach, which translates information into figures, so that they can be classified and analyzed by using statistical techniques [12]. The research was conducted in Recife, capital city of the state of Pernambuco, a coastal metropolis that occupies a central position, 800 km far from other two regional metropolises, Salvador and Fortaleza – fighting with them for a strategic influence on northeastern Brazil.The locus of research was the ‘Agamenon Magalhães’ Hospital, located in the metropolitan region of Recife. This is a public hospital that serves more than 5,000 patients per month within its 4 emergency sectors (Clinic, Cardiology, Otorhinolaryngology, and High Risk Maternity), where more than 10,000 outpatient appointments per month are provided at the specialty outpatient facilities, among them gynecology. The ‘Agamenon Magalhães’ Hospital is an institution linked to the network of the Pernambuco State Health Department, accredited by the Ministry of Education and the Ministry of Health as a teaching hospital, similar to most university hospitals in the country. It has 477 beds, 59 of them in adult and neonatal ICUs.Considering hysteroscopy, about 15 procedures are performed each month. Women are referred from the gynecology outpatient clinic of the ‘Agamenon Magalhães’ Hospital and other gynecological services and outpatient clinics in Recife. Those referred to undergo hysteroscopy are screened in the institution to determine the actual indications. Once the need for this procedure is confirmed and the preoperative examinations are performed, women undergo hysteroscopy by the medical team members who work at the specialized gynecology service. During the hysteroscopic procedure, material is collected from the uterine cavity for histopathologic examination.The study was conducted with secondary data obtained from the medical reports issued as results of hysteroscopic examination and histopathologic study of endometrial and/or endocervical samples. Data were collected from all women submitted to hysteroscopy at the ‘Agamenon Magalhães’ Hospital, within the period from September 2015 to March 2016, and a total of 97 medical records were analyzed, whose biopsy was advised (i.e. after visualization of intrauterine lesions, the hysteroscope is removed and the material is obtained by curettage or aspiration) or carried out (material collection through direct hysteroscopic visibility).Data collection was conducted in October 2016, after approval by the Research Ethics Committee of the ‘Agamenon Magalhães’ Hospital, under the Brazilian Certificate of Submission for Ethical Assessment (CAAE) no. 61666716.8.0000.5197. Information was collected from the medical records service of the institution and reviewed according to the sample eligibility criteria.Data obtained was organized, according to the variables of interest in the study, on a database organized by means of the software Microsoft Excel. Descriptive statistics has been adopted for data processing; the results were organized into tables and graphs containing absolute and relative values – discussed in the light of the literature.This study was conducted complying both with the Resolution no. 466/2012, from the Brazilian National Health Council (CNS), and the 2008 Declaration of Helsinki, which provide for research involving human beings.
3. Results
- The analysis addressed 97 records, and 68 of them were selected for the sample (70.1%), due to their information on the hysteroscopic procedure and the material sent to the histopathologic examination.The age of women whose examinations were analyzed ranged from 31 to 89 years, with an average of 53.7 years, and 49.4% were aged ≥ 50 years (Graph 1).
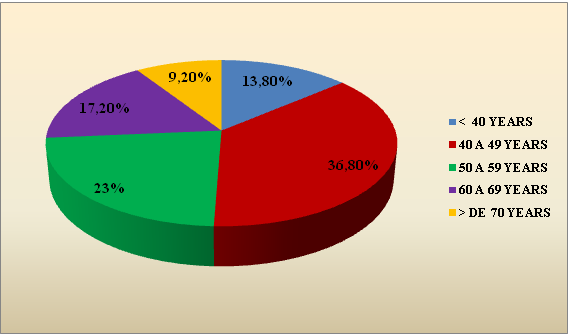 | Graph 1. Sample distribution according to the age group. Recife, 2016. (Source: Prepared by the authors) |
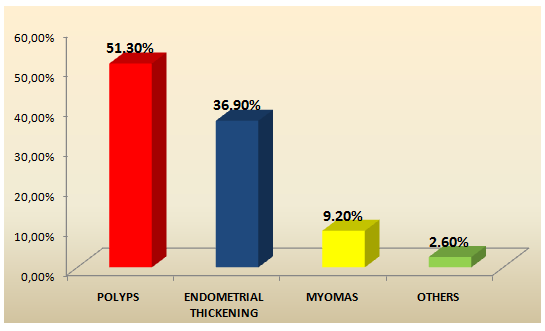 | Graph 2. Percentage distribution of pathologies that justified hysteroscopy indications. Recife, 2016. (Source: Prepared by the authors) |
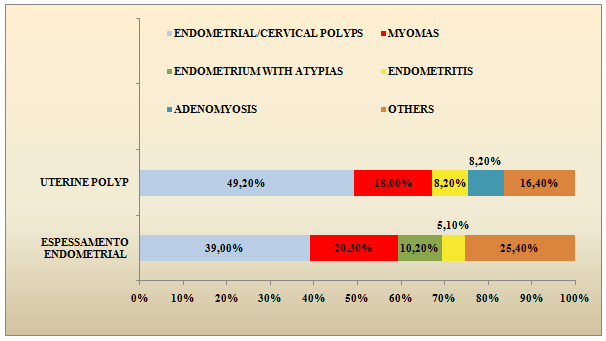 | Graph 3. Distribution of the percentage of changes that justified hysteroscopy and the correlation with their respective results. Recife, 2016. (Source: Prepared by the authors) |
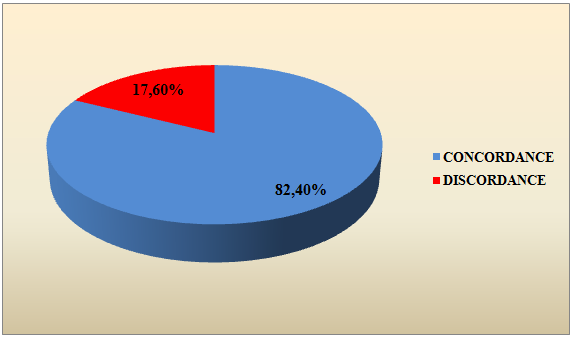 | Graph 4. Percentage of the correlation between hysteroscopy results and the respective histopathological reports. Recife, 2016. (Source: Prepared by the authors) |
4. Discussion
- This study was conducted having the review of hysteroscopic and histopathologic reports as a basis. Currently, hysteroscopy is regarded as a gold-standard exam in the endometrial evaluation, because it allows direct visualization of the cavity and it allows the therapeutic approach of lesions. After the introduction of hysteroscopy and especially since technological advances and the hysteroscopy technique itself have made it possible to perform this in a simple, safe, and tolerated way, it has taken a major role in the study of intra-uterine pathology, especially in the context of postmenopausal metrorrhagia.Most of indications for this procedure were motivated by endometrial thickening and presence of polyps. This fact is justified because the most suitable propaedeutic method available for evaluating the uterine cavity in women with suspected endometrial thickening, either asymptomatic or with vaginal bleeding, is hysteroscopy [13].Endometrial thickening is defined as ≥ 5 mm endometrium on the ultrasonography of menopausal women without hormone therapy [1]. Almost all the studies carried out to evaluate the accuracy of the ultrasound examination used as 4 or 5 mm cutoff point, threshold below which the possibility of malignant disease is extremely low.Studying the endometrium is of relevant importance in all women who are in the menopausal climacteric, for the purpose of detecting possible precursor lesions and initial carcinomas in the uterine mucosa. Considering the limitations of clinical propaedeutics, there is a need to use adequate complementary diagnostic methods, such as ultrasonography followed by diagnostic hysteroscopy [14].Increased endometrial thickness can be caused by endometrial polyps, endometrial hyperplasia, or even endometrial carcinoma [1]. Ultrasound can diagnose submucous polyps, septa, and myomas with high accuracy. However, hysteroscopy has been indicated to confirm and remove these changes.Endometrial thickness is much more significant in symptomatic premenopausal women than in asymptomatic ones [15]. The endometrial thickening value may also be a major tool in the diagnosis of endometrial carcinoma and hyperplasia in premenopausal women.Thus, some studies have shown there is not always a correlation between the finding of thickening in the uterine mucosa obtained by transvaginal ultrasonography with lesions within the uterine cavity. Thus, in a significant part of the menopausal patients with thickened endometrial echo, intracavitary abnormalities consisted of endometrial polyp, intrauterine synechia, submucous myoma, or intracavitary fluid, especially mucus [7].In this investigation, a positive correlation was detected between the occurrence of endometrial thickening and uterine polyp, with hysteroscopy and histopathology in more than 56% of the cases.Endometrial polyps, on ultrasonography, are characterized by focal endometrial thickening with hyperechogenic appearance, always in continuity with the basal endometrial layer. However, they may also have a high frequency in the form of non-specific and heterogeneous endometrial thickening (with or without cystic areas), since these tumors suffer flattening due to the compression exerted by the uterine walls. However, these lesions represent high rates of false negatives, when investigating hysteroscopically.Polyps have a higher prevalence among women within the age group from 40 to 60 years, showing a twice-higher frequency among postmenopausal women, when compared to the menacme period, since it corroborates the age group of most women who participated in this study. The term endometrial polyp is histologically recognized by the fibrous stroma and thick-walled blood vessels, typical of the basal layer, which often accompany its major axis, may be covered by normal, atrophic glandular epithelium, or other changes than simple hyperplasia. Despite the occurrence of simple hyperplasia, which is in essence a part of the glandular epithelium of many endometrial polyps, they rarely undergo malignant change. In several studies including women with abnormal uterine bleeding, the frequency of malignancy associated with polyps ranged from 0.59% to 3.2%, and it mostly occurs in postmenopausal women [4].Within the reproductive period, the diagnosis of endometrial polyp is most often determined in symptomatic patients, with abnormal uterine bleeding, or in infertile patients undergoing diagnostic hysteroscopy. On the other hand, asymptomatic endometrial polyps, whose only finding is usually focal endometrial thickening, occasionally diagnosed by post-menopausal transvaginal ultrasonography, may be a risk factor for endometrial cancer [4].Polyps account for 21% to 28% of all causes of postmenopausal uterine bleeding, making it a relevant condition for differential diagnosis of endometrial neoplasm. In this study, there was a prevalence of endometrial polyps (34.4%) and cervical polyps (4.2%), and the association of polyps with endometrial neoplasm has not been detected.The incidence of endometrial cancer associated with polyps is around 3.5%, varying according to most studies around 4.8%, and this risk is higher in postmenopausal and bleeding women.In this investigation, the occurrence of neoplasm associated with endometrial thickening was above the percentage observed in the literature and this data may be associated to the fact that the research was conducted in a referral service of medium and high complexity for the treatment of gynecological pathologies that receives patients under cancer investigation. Ultrasonographic signs of endometrial cancer include heterogeneity and irregular endometrial thickening, which are nonspecific signs that can also be seen in cases of hyperplasia and polyps [7].
5. Final Remarks
- Despite the limited sample analyzed and the difficulties related to access to information from all exams performed within the data collection period, it was possible to conclude, through this study that the existence of clinical and ultrasound findings of endometrial thickening had a positive correlation around 56% with the diagnosis of uterine polyp by histopathological examination.The occurrence of endometrial cancer was found in 7.35% of the studied sample, especially grade II adenocarcinoma, in women with an average age of 62.7 years. Cases of endometrial neoplasms were identified in the hysteroscopic study through endometrial thickening.A correlation of more than 80% of the hysteroscopy findings and the analysis of histopathological samples was regarded as favorable, making it possible to affirm that the behavior of methods to support the diagnosis of endometrial pathologies analyzed in this study is effective.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML