-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Obstetrics and Gynecology
p-ISSN: 2326-120X e-ISSN: 2326-1218
2017; 5(1): 7-9
doi:10.5923/j.rog.20170501.02

Primary Ovarian Carcinoid Tumor, Rare Type of Ovarian Germ Cell Neoplasm: A Case Report
Bhoomika Tantuway1, Y. M. Mala1, R. Tripathi1, Nidhi Mahajan2
1Department of Obstetrics and Gynaecology, Maulana Azad Medical College and Associated Lok Nayak Hospital, University of Delhi, New Delhi, India
2Pathology at Chacha Nehru Bal Chikitsalaya, New Delhi
Correspondence to: Bhoomika Tantuway, Department of Obstetrics and Gynaecology, Maulana Azad Medical College and Associated Lok Nayak Hospital, University of Delhi, New Delhi, India.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

A 44 years old lady with 18-20 weeks, firm to hard mass in lower abdomen presented to Department of Obstetrics and Gynaecology, LNJP Hospital, New Delhi. After all pre-op investigations patient was posted for surgery, staging laparotomy with total abdominal hysterectomy with bilateral salpingoopherectomy, bilateral pelvic and paraaortic lymphadenectomy, infracolic omentectomy was done. Per operatively 15x10 cms left ovarian solid to cystic mass with single septation was present. Final histopathology report of ovarian mass shows tumor present in form of nests, trabeculae and ribbons. Cells are monomorphic with abundant granular eosinophilic cytoplasm with a centrally placed elongated nucleus, stripped nuclear chromatin. Mitotic activity was less than 1/10. Immunohistochemistry strongly express synaptophysin and focally express chromogranin, cytokeratin. Ovarian capsule was free of tumor. Overall histology and immunohistochemistry was suggestive of pure trabecular carcinoid of left ovary. Patient was investigated for carcinoid elsewhere in body, but results were negative. Patient was staged as stage 1A and adjuvant chemotherapy was not given. She is under follow up without any signs of recurrence.
Keywords: Ovarian carcinoid tumor, Stage 1A, Adjuvant chemotherapy
Cite this paper: Bhoomika Tantuway, Y. M. Mala, R. Tripathi, Nidhi Mahajan, Primary Ovarian Carcinoid Tumor, Rare Type of Ovarian Germ Cell Neoplasm: A Case Report, Research in Obstetrics and Gynecology, Vol. 5 No. 1, 2017, pp. 7-9. doi: 10.5923/j.rog.20170501.02.
1. Introduction
- Primary ovarian carcinoid tumor is a very rare type of ovarian germ cell neoplasm. It constitutes about <0.1% of all ovarian malignancies. Gastro intestinal tract and lungs are the most common site for carcinoid tumor [1]. Carcinoid tumor can present with four different types of histopathology, which are Insular, trabecular, strumal and mucinous. The most common presentation is of insular pattern (26-53%) [2] but clinical carcinoid syndrome is usually associated with trabecular type and it also has a favorable prognosis. We are reporting a case of primary trabecular type of ovarian carcinoid tumor.
2. Case Report
- A 44-year-old lady presented to the department of Delhi with complaints of pain in lower abdomen for 1 year. On examination, a 18-20 weeks mass was felt in lower abdomen, firm to hard in consistency and lower limit of mass could not be reached. Her general physical examination and Obstetrics and Gynaecology, Lok Nayak Hospital, New routine investigation revealed no abnormality. Ultrasonography showed a normal size uterus with an irregular cystic mass of 17x12 cm in left adnexa with echogenic fluid and few septae. Left ovary could not be identified separately. Right ovary was normal. Serum CA-125 was 30 U/ml. On MRI, a large solid cystic mass of 14.3x10x14 cm was seen with incomplete septations and thick enhancing wall. This mass was closely abutting the left broad ligament and adnexa. On staging laparotomy, a 15x10 cms ovarian mass was present on left side, solid in consistency with few septations. This ovarian mass was sent for frozen section, which reported as malignant epithelial neoplasm of ovary. Therefore, total abdominal hysterectomy, bilateral salpingoopherectomy, bilateral pelvic and paraaortic lymphadenectomy with infracolic omentectomy was performed. Patient was stable post operatively. Final histopathology report revealed unremarkable uterus and cervix with trabecular carcinoid of left ovary. Microscopic picture of the ovarian cyst showed a tumor in form of nests, trabeculae and ribbons. The cells were monomorphic, bland appearing elongated with abundant granular eosinophilic cytoplasm with a centrally placed elongated nucleus and stripped nuclear chromatin. Mitotic activity was less than 1/10. Further immunohistochemistry showed a strong expression of symptophysin and focal expression of chromogranin and cytokeratin. Tumor cells were negative for inhibin and calretinin. Ovarian capsule was free of tumor involvement. Patient was investigated for carcinoid elsewhere in the body which included upper, lower GI endoscopy, CECT chest, USG whole abdomen and TFT. All reports were found to be normal. Final diagnosis of ovarian carcinoid tumor stage IA was made. Adjuvant chemotherapy was not planned as patient is stage IA. Patient is currently under follow up without any symptoms and signs of recurrence.
3. Discussion
- Primary ovarian carcinoid tumor is rare ovarian neoplasm, constituting <0.1% of all ovarian neoplasm. It commonly occurs in peri-menopausal and postmenopausal age group [3]. Primary ovarian carcinoid is more common as compared to secondary ovarian carcinoid, which is usually secondary to gastrointestinal carcinoid. Primary ovarian carcinoid is mostly associated with mature cystic teratoma. Ovarian carcinoid either presented with abdominal mass or features of carcinoid syndrome, eg episodic cutaneous flushing, cyanosis, abdominal cramps, diarrhea, carcinoid heart disease. Surgery is the mainstay of treatment for ovarian carcinoid [4]. Role of chemotherapy is not very well defined for it. And our patient was also staged as stage 1A and not given adjuvant chemotherapy and patient had not shown any signs of recurrence.Histopathology slides
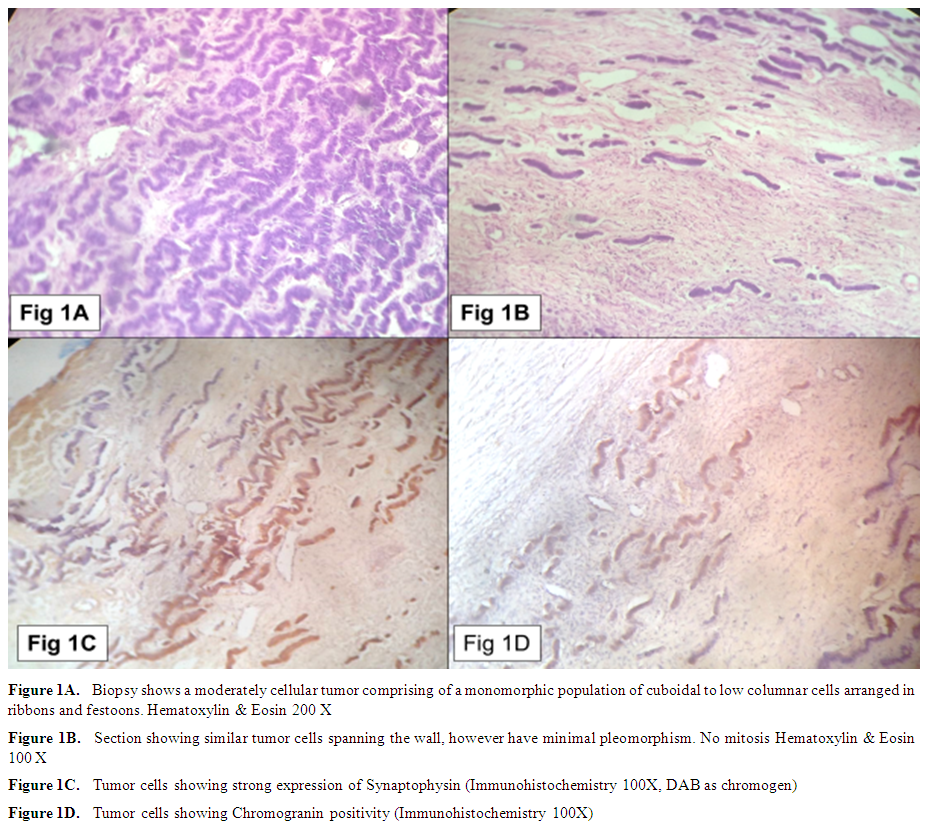 | Figure 1 |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML