-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Obstetrics and Gynecology
p-ISSN: 2326-120X e-ISSN: 2326-1218
2016; 4(1): 1-6
doi:10.5923/j.rog.20160401.01

The Effect of Acupressure on Non-stress Test Parameters in Primiparous Women
Maasumeh Kaviani1, Rafat Ebadi2, Sara Azima1, Nasrin Asadi3, Mohammad Javad Hadianfard4, Mehrab Sayadi5
1Department of Midwifery, School of Nursing and Midwifery, Shiraz University of Medical Sciences, Shiraz, Iran
2Department of Midwifery, Student Research Committee, Shiraz University of Medical Sciences, Shiraz, Iran
3Fellowship Student of Perinatology, Department of Gynecology and Obstetrics, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran
4Department of Physical Medicine and Rehabilitation, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran
5Department of Biostatistics, School of Health, Behbahan University of Medical Sciences, Shiraz, Iran
Correspondence to: Sara Azima, Department of Midwifery, School of Nursing and Midwifery, Shiraz University of Medical Sciences, Shiraz, Iran.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

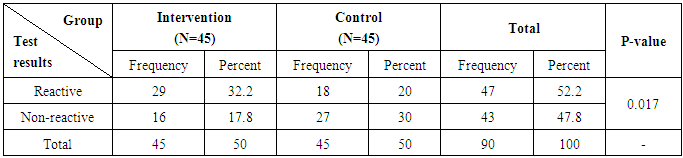
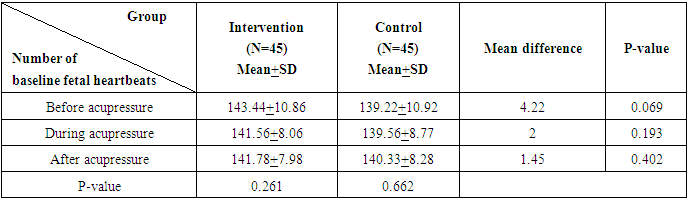
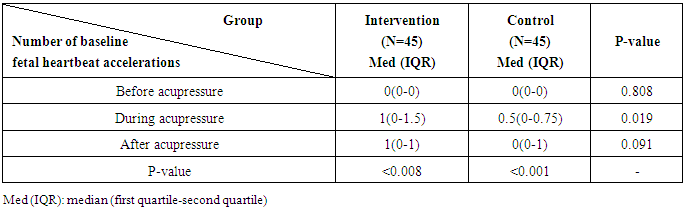
Abstract Non-Stress Test (NST) is one of the main methods of fetal health assessment. In this method, the fetus receives a score based on increase in its heartbeat while movement. The present study aimed to investigate the effect of acupressure at Zhiyin (BL67) acupoint on NST parameters in primiparous women. In this randomized clinical trial, 90 primiparous women were randomly divided into an intervention (acupressure at BL67 acupoint) and a control group (touching BL67 acupoint without application of acupressure). The NST parameters were interpreted by a perinatologist. Finally, the data were entered into the SPSS statistical software and analyzed using independent t-test, Fisher’s exact test, and repeated measures ANOVA. The results showed a significant increase in fetal heartbeat accelerations during application of acupressure in the intervention group compared to the control group (P=0.019). Also, a significant difference was observed between the two groups regarding the percentage of reactive test results (P=0.017).Application of acupressure at Zhiyin (BL67) acupoint increased fetal heartbeat accelerations and the rate of reactive test results.
Keywords: Non-stress test, Acupressure, Pregnancy, Primiparous women
Cite this paper: Maasumeh Kaviani, Rafat Ebadi, Sara Azima, Nasrin Asadi, Mohammad Javad Hadianfard, Mehrab Sayadi, The Effect of Acupressure on Non-stress Test Parameters in Primiparous Women, Research in Obstetrics and Gynecology, Vol. 4 No. 1, 2016, pp. 1-6. doi: 10.5923/j.rog.20160401.01.
Article Outline
1. Introduction
- One of the main components of pregnancy care is evaluation of fetal health which aims to diagnose high-risk fetuses and prevent complications, particularly fetal and infantile mortality [1]. The most common tests used for investigation of fetal health before delivery include Non-Stress Test (NST), Contraction Stress Test (CST), and Biophysical Profile (BPP) [2]. In comparison to the other two tests, NST is a non-invasive and inexpensive method which does not require the beginning of uterine contractions [3]. This test is usually selected for evaluation of fetal health and survival [4]. In this method, electronic monitoring is employed in order to record fetal heartbeat. Following fetal movement, fetal heartbeat is accelerated providing the basis for NST [5, 6]. Increase in fetal heartbeat due to movement represents normal pH and fetal status [7, 8].In order to decrease the rate of false positive NST results, various methods have been proposed, including moving the fetus, lengthening the test time, vibroacoustic stimulation of the fetus before the test, changing the mother’s position, and application of acupressure. Among these methods, acupressure is the easiest, does not require any specific equipment or position change, and can lead to maternal relaxation [9, 10]. Acupressure is one of the complementary medicines in which fingers are used to apply pressure on key points on the skin for stimulation and induction of body’s natural self-treatment [11]. Zhiyin (BL67) point is one of the acupoints used in acupressure. Evidence has shown that stimulation of this point leads to movement and change in the position of the fetus. This acupoint lies on the little toe just on the outside aspect of the toenail on the bladder meridian. Yet, this has not been confirmed in all the studies conducted on the issue. [12]Reactive NST results are among the main methods for evaluation of fetal health [1, 13]. Considering the fact that a limited number of studies have been conducted on the effect of acupressure on fetal health, the present study aims to investigate the effect of acupressure at Zhiyin (BL67) acupoint on NST parameters.
2. Patients and Methods
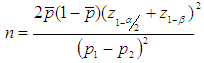
- The present clinical trial was conducted on 90 primiparous women referring to Hafez hospital, Shiraz, Iran between August and December 2013. Based on the study by Neri et al., 2002 [14], considering power of 80%, α=5%, mean difference of 27%, and loss rate of 10%, and using the following formula, a 90-subject sample size (45 in each group) was determined for the study.
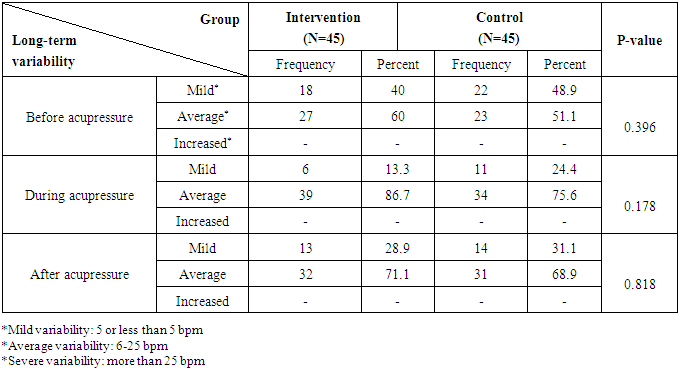
 The study samples were selected through purposive sampling and were divided into an intervention and a control group using permuted block randomization. According to the hospital protocol, NST is performed for all the mothers with the gestational age of 37-42 weeks who refer for prenatal care. The inclusion criteria of the study were being 18-35 years old, singleton pregnancy, gestational age of 37-40 weeks, baseline fetal heartbeat of 110-160 beats per minute (bpm), not suffering from psychological diseases, such as psychosis and anxiety disorders, not suffering from chronic diseases, such as cardiovascular, pulmonary, and kidney diseases, hypertension, and diabetes, not having severe activity 2 hours before the test, having eaten a meal at least 2 hours before the test, and having non-reactive test results before beginning of the study. On the other hand, the exclusion criteria of the study were the incidence of midwifery events, such as labor pain, detachment, and umbilical cord prolapse, and not being willing to take part in the study.The study data were collected using a questionnaire containing two parts. The first part which included demographic information was completed by the researcher. In addition, the second part consisted of NST parameters and was filled out by a perinatologist.At first, the subjects were asked to lie down on the left side. In this study, Doppler transducer was used to record fetal heartbeat, while Toko dynamometer was utilized for recording the uterine contractions. In the current study, NST was recorded for 20 minutes. Five minutes after the beginning of the test in the intervention group, acupressure was applied at Zhiyin (BL67) acupoint (figure 1) for 10 minutes (5 minutes on each foot). In doing so, 2 kg pressure was applied for 30 seconds followed by a 10-second rest. Duration and intensity of acupressure was determined based on consultation with a specialist in physical medicine and rehabilitation as well as the previous studies conducted on the issue [15, 16]. It should be noted that fetal heartbeat was continually recorded by Analogic Line-TM device (made in Japan) during and 5 min after application of acupressure. In the control group, the researcher only touched the BL67 acupoint, but did not perform acupressure. The recorded NSTs were evaluated by a specialist at the hospital. Afterwards, the recorded NSTs were given to a perinatologist who was unaware of the study process. Accordingly, the second part of the questionnaire was completed.The parameters recorded in the current study included baseline fetal heartbeat, long-term heartbeat variability, and heartbeat acceleration. Based on the National Institute of Child Health and Human Development [17], baseline heartbeat is defined as the mean of heartbeats in 10 minutes after rounding more than 5 bpm increases. In addition, variability is defined as change in fetal heartbeat for 2 cycles in a minute. Variability is determined as the distance between the minimum (0) and maximum (25) number of heartbeats based on bpm. Accordingly:Lack of variability: The distance is not measurable.Mild variability: The distance is measurable to 5 bpm or less.Average variability: The distance is 6-25 bpm.Severe variability: The distance is above 25bpm.Finally, acceleration is defined as a sudden, detectable increase of 15 bpm or more in fetal heartbeat lasting for more than 15 seconds.
The study samples were selected through purposive sampling and were divided into an intervention and a control group using permuted block randomization. According to the hospital protocol, NST is performed for all the mothers with the gestational age of 37-42 weeks who refer for prenatal care. The inclusion criteria of the study were being 18-35 years old, singleton pregnancy, gestational age of 37-40 weeks, baseline fetal heartbeat of 110-160 beats per minute (bpm), not suffering from psychological diseases, such as psychosis and anxiety disorders, not suffering from chronic diseases, such as cardiovascular, pulmonary, and kidney diseases, hypertension, and diabetes, not having severe activity 2 hours before the test, having eaten a meal at least 2 hours before the test, and having non-reactive test results before beginning of the study. On the other hand, the exclusion criteria of the study were the incidence of midwifery events, such as labor pain, detachment, and umbilical cord prolapse, and not being willing to take part in the study.The study data were collected using a questionnaire containing two parts. The first part which included demographic information was completed by the researcher. In addition, the second part consisted of NST parameters and was filled out by a perinatologist.At first, the subjects were asked to lie down on the left side. In this study, Doppler transducer was used to record fetal heartbeat, while Toko dynamometer was utilized for recording the uterine contractions. In the current study, NST was recorded for 20 minutes. Five minutes after the beginning of the test in the intervention group, acupressure was applied at Zhiyin (BL67) acupoint (figure 1) for 10 minutes (5 minutes on each foot). In doing so, 2 kg pressure was applied for 30 seconds followed by a 10-second rest. Duration and intensity of acupressure was determined based on consultation with a specialist in physical medicine and rehabilitation as well as the previous studies conducted on the issue [15, 16]. It should be noted that fetal heartbeat was continually recorded by Analogic Line-TM device (made in Japan) during and 5 min after application of acupressure. In the control group, the researcher only touched the BL67 acupoint, but did not perform acupressure. The recorded NSTs were evaluated by a specialist at the hospital. Afterwards, the recorded NSTs were given to a perinatologist who was unaware of the study process. Accordingly, the second part of the questionnaire was completed.The parameters recorded in the current study included baseline fetal heartbeat, long-term heartbeat variability, and heartbeat acceleration. Based on the National Institute of Child Health and Human Development [17], baseline heartbeat is defined as the mean of heartbeats in 10 minutes after rounding more than 5 bpm increases. In addition, variability is defined as change in fetal heartbeat for 2 cycles in a minute. Variability is determined as the distance between the minimum (0) and maximum (25) number of heartbeats based on bpm. Accordingly:Lack of variability: The distance is not measurable.Mild variability: The distance is measurable to 5 bpm or less.Average variability: The distance is 6-25 bpm.Severe variability: The distance is above 25bpm.Finally, acceleration is defined as a sudden, detectable increase of 15 bpm or more in fetal heartbeat lasting for more than 15 seconds.3. Statistical Analysis
- The study data were analyzed using descriptive as well as inferential statistical methods including chi-square test, repeated measures ANOVA, and Friedman, Mann-Whitney U, and McNemar non-parametric tests. Besides, P<0.05 was considered as statistically significant. All the analyses were performed using the SPSS statistical software (v. 16).
4. Ethical Considerations
- After gaining the approval of the Ethics Committee of Shiraz University of Medical Sciences (CT-90-6660) and registration of the study in Iranian Registry of Clinical Trials (IRCT2013111815449N1), the study objectives were explained to the participants and written informed consents were obtained from them. Both groups received the routine care. According to the hospital’s treatment protocol, in case non-reactive test results were obtained, NST was performed for the third time after having a meal. If non-reactive NSTs were obtained again, biophysical profile was requested and the necessary measures were taken based on the results.
5. Results
- The present study was conducted on 90 primiparous women referring to Hafez hospital affiliated to Shiraz University of Medical Sciences, Shiraz, Iran. The study results revealed no significant difference between the two groups regarding demographic characteristics, including mother’s age (P=0.178), gestational age (P=0.938), level of education (P=0.216), mother’s occupation (P=0.11), and time of performance of the test (P=0.238). The mean age of the study participants was 26.63+4.62 years and their mean gestational age was 37-38 weeks.The study results revealed a significant difference between the intervention and the control group regarding the percentage of reactive NST results (P=0.017) (Table 1). However, no significant difference was observed between the two groups concerning baseline fetal heartbeat before (P=0.069), during (P=0.193), and after application of acupressure (P=0.402) (Table 2).
|
|
|
|
6. Discussion
- Nowadays, there is no agreement on the best method for evaluation of fetal health [18]. Devoe believed that an appropriate diagnostic instrument must differentiate the features of a normal fetus from those of a high-risk one [19]. Reactive NST results encourage continuation of pregnancy. Non-reactive results, on the other hand, necessitate more accurate examinations [20-22].The present study aimed to assess the effect of acupressure on NST parameters in primiparous women. The study results indicated that application of acupressure at Zhiyin (BL67) acupoint increased fetal heartbeat accelerations and the percentage of reactive NST results. Neri et al. (2007) reported that acupuncture accompanied by moxibustion at Zhiyin acupoint was effective in reduction of fetal heartbeats, while none of these two methods alone affected the baseline fetal heartbeat [23]. Guittier et al. (2008) evaluated the effect of moxibustion on change of the fetus’ position from breech to cephalic. In doing so, they measured fetal heartbeat 10 minutes before, 20 minutes during, and 10 minutes after moxibustion at Zhiyin acupoint. The study results showed that the fetal heartbeats were normal through the study [24], which is consistent with the findings of the current study.The present study results revealed a significant increase in the number of fetal heartbeat accelerations while application of acupressure. In the study by Pirhadi et al. (2013), stimulation of BL67 acupoint reduced the time interval between the first and the second acceleration, but did not change other NST parameters [25]. Similarly, Neri and Fazzio (2002) reported that stimulation of BL67 acupoint increased the number of accelerations [14], which is in agreement with the results of our study. However, Cardini et al. (1998) showed that stimulation of Zhiyin (BL67) acupoint had no impacts on the number of accelerations [26].It should be noted that mechanism of effect of BL67 acupoint stimulation on fetal behavior has not been identified in the above-mentioned studies [27]. Yet, it seems that stimulation of this point stimulates the adrenal cortex, eventually increasing paired estrogen and changing prostaglandin F/prostaglandin E ratio (reducing prostaglandin E but not changing prostaglandin F, thereby increasing prostaglandin F/prostaglandin E ratio). Estrogen, in turn, increases the uterus’ sensitivity to response to prostaglandin F. This mechanism may increase the fetal movements, resulting in an increase in fetal heartbeat. This effect may also continue after disruption of BL67 acupoint stimulation [26, 28, 29]. Nevertheless, fetal-maternal adrenal gland suppression leads to a reduction in fetal heartbeat. Although a large number of factors affect fetal heartbeat regulation, most studies have referred to endocrine factors [30]. Accordingly, fetal heartbeat rhythm is affected by fetal-maternal adrenal gland suppressionas well as by changes in mother’s cortisol levels [31].The findings of the present study revealed no significant difference between the two groups regarding long-term fetal heartbeat variability before, during, and after application of acupressure. Previous studies have indicated that mother’s anxiety level was effective in fetal heartbeat variability. For instance, Kafalli et al. (2011) investigated the effect of music and mother’s anxiety on fetal heartbeat. The results demonstrated that the control group mothers’ anxiety scores increased after the NST compared to before the test. They also stated that NST, itself, was a stressful process for mothers [32].The studies measuring fetal heartbeat during pregnancy have indicated that maternal stress and anxiety led to long-term variability in fetal heartbeat. In one study, the mothers exposed to laboratory stressors had fetuses with lower heartbeat variability [33]. Moreover, Glover et al. (2009) revealed the relationship between maternal and fetal cortisol levels in pregnant women and stated that mother’s emotional and mental status was effective in function of the placenta [34]. Uterine arteries resistance is influenced by some factors which affect mother’s peripheral blood flow. However, anxiety and stress increase arterial pressure and reduce uterine blood flow, eventually increasing umbilical arteries resistance and affecting fetal cardiac function [35]. One of the limitations of the present study was that the mothers’ anxiety level was not measured before and after NST. In addition, this study was conducted on healthy primiparous women; thus, the effect of acupressure on high-risk (diabetes, preeclampsia), multiparous, preterm, and post-term mothers cannot be determined.Conclusions: According to the results of the current study, it seems that application of acupressure on Zhiyin (BL67) acupoint increased the accelerations and led to reactive NST results. Considering the fact that acupressure is a simple, safe, and inexpensive method, can be performed by the individuals themselves, does not require specific facilities, and can improve NST, it is recommended to be performed in prenatal clinics. Yet, further studies with larger sample sizes are recommended to be conducted on high-risk mothers who need repetition of NST.
ACKNOWLEDGEMENTS
- This article was extracted from Rafat Ebadi' M.Sc. thesis approved by Shiraz University of Medical Sciences (proposal No 92-6660).Hereby, the authors would like to thank the Research Vice-chancellor of Shiraz University of Medical Sciences, personnel of NST department in Hafez hospital, and all the individuals who cooperated in the study. The authors are also grateful for Ms. A. Keivanshekouh at the Research Improvement Center of Shiraz University of Medical Sciences for improving the use of English in the manuscript.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML