-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Obstetrics and Gynecology
p-ISSN: 2326-120X e-ISSN: 2326-1218
2013; 2(3): 13-27
doi:10.5923/j.rog.20130203.01
The Impact of Education on Recommended Weight Gain and Selected Prenatal Outcomes in Low Income Pregnant Women
1Clayton State University, School of Nursing, Morrow, Georgia, 30260, United States of America
2Marguerite Murphy, Georgia Health Sciences University, Augusta, Georgia, 30912, United States of America
3Betty Lane, Clayton State University, School of Nursing, Morrow, Georgia, 30260, United States of America
Correspondence to: Grace M. Nteff, Clayton State University, School of Nursing, Morrow, Georgia, 30260, United States of America.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
The study aims were to educate pregnant women about appropriate nutrition during pregnancy, the Institute of Medicine (IOM) weight gain guidelines and obesity risks; to determine the relationship between education and actual maternal weight gain; to determine the relationship between education and selected prenatal outcomes.A two-group design compared outcome measures of maternal weight, blood pressure, pre-pregnant BMI, and fundal height measurements post-education intervention among 40 low income women. The intervention group was a convenience sample of prenatal care patients. Intervention participants received individualized education about nutrition during pregnancy, obesity risks, and IOM weight gain guidelines. Weight gain was plotted on pre-determined BMI weight gain graphs during 4 visits post-intervention for two months. The control group, derived from a sequential retrospective chart review was matched with intervention participants on four variables. Results indicated no statistical significance between education and study variables except education and first visit blood pressure @ p = 0.04. Knowledge about nutrition, IOM weight gain guidelines and obesity risks did not result in expected pregnancy weight gain.
Keywords: Nutrition, Pregnancy, Education, IOM Weight Gain Guidelines, Obesity Health Risks, Low Income Pregnant Women
Cite this paper: Grace M. Nteff, The Impact of Education on Recommended Weight Gain and Selected Prenatal Outcomes in Low Income Pregnant Women, Research in Obstetrics and Gynecology, Vol. 2 No. 3, 2013, pp. 13-27. doi: 10.5923/j.rog.20130203.01.
Article Outline
1. Introduction
- Obesity is a serious and growing health problem in society today. In 2005, the Surgeon General estimated that two thirds of Americans were either overweight or obese[33]. This number represents 331.6 million adults, 62% women and 71% men[49]. Considering the alarming numbers of overweight or obese persons today, it is no surprise that at the diagnosis of a pregnancy most women are already overweight or obese[14]. In minority and low-income women, being overweight or obese is a common obstetric condition. Among females of childbearing age, African Americans (AA) and Hispanics have a 51% and 21% higher prevalence of being overweight and obese respectively, compared to Caucasian women. In a longitudinal study conducted by[13], to examine the distribution of weight gain among low income women with a normal pre-pregnancy weight, Caucasian women had the highest excess gestational weight gain of 55.9%, followed by Hispanic women and black women with gestational weight gains of 51.9% and 41.7%, respectively.Excess gestational weight increases the risk of negative long and short-term maternal and fetal consequences. Long-term, the risk for gestational hypertension doubles and the risk for gestational diabetes quadruples. Osteoarthritis, breast, colon and endometrial cancer, overweight and obesity in later life[62] are other long term risks.Short-term, consequences include increased incidence of cesarean section delivery, risk for pre-term birth (PTB) (<37 weeks), and very low birth weight (VLBW) < 2500 g neonates[4],[11],[56]. Serious fetal outcomes include macrocosmic (> 4000 gm) newborns and neonatal hypoglycaemia, with the potential for admission to Neonatal Intensive Care Units (NICU)[58]. Maintaining appropriate maternal weight gain during pregnancy may also have a positive impact on health care expenditures since maternal and neonatal complications account for 5.7% of direct healthcare costs, and annual costs of $52 billion[46]. Premature neonate care account for 40% to 60% of estimated annual hospital costs of $26.2 billion, with $5.8 billion for direct costs, and $3,500 daily for NICU costs[26],[38],[34]. The average length of hospitalization after delivery of an overweight or obese pregnant woman is 4.4 and 4.5 days respectively, compared to 2.4 days for a normal weight pregnant woman[14]. Several studies have demonstrated that nutrition education and counselling alone, or combined with other behavioral lifestyle changes, have positive effects on pregnancy weight gain and outcomes. This study examined the impact of knowledge about nutrition, recommended pregnancy weight gain, and obesity-related health risks on actual weight gained in low income women.
1.1. Purpose
- The purposeof this study was to examine the impact of knowledge about nutrition, recommended pregnancy weight gain, complications of excessive weight gain, and obesity related health risks on actual weight gained during pregnancy among low income women.
1.2. Specific Aims
- Specific aims included: 1) educate pregnant women regarding appropriate nutrition during pregnancy,recommended weight gain guidelines and obesity associated risks; 2) determine if there is a relationship between education and actual weight gained during pregnancy; and, 3) determine if there is a relationship between education and selected prenatal outcomes like weight gain, fundal height measurements, and blood pressure.
1.3. Background
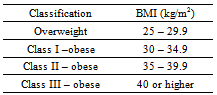
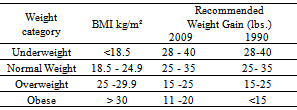
- Among women, a vulnerable weight gain period is during pregnancy when an increase in weight gain is required to support increased metabolic demands and enhance positive pregnancy outcomes[54]. Increased weight gain during pregnancy is accomplished by increased caloric intake via diet. Weight gained, and not lost, but carried over from one pregnancy to another, can be a trigger for obesity during the childbearing years and in later life for women[41]. Gestational weight gain has been identified to be an independent predictor of long term weight gain and obesity in women[42]. Overweight during pregnancy is defined as a weight gain of more than 25 pounds by women with a pre-pregnant BMI between 25- 29.9 kg/m², and obesity is defined as a weight gain of more than 20 pounds by women with a pre-pregnant BMI > 30 kg/m²[13]. Adult obesity is further classified as Class I – III and associated with chronic disease states such as type 2 diabetes mellitus, cardiovascular disease, sleep apnea, and cerebral infarcts[48]. See Table 1.
|
|
2. Conceptual Framework
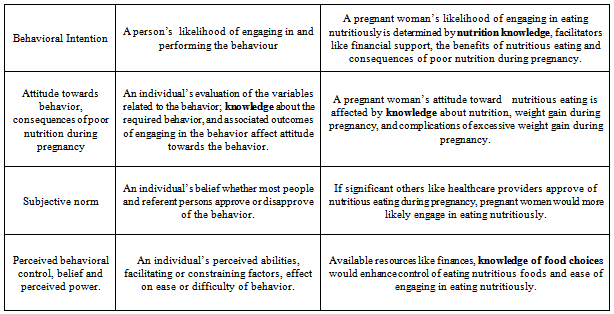
- The Theory of Reasoned Action (TRA) provided the conceptual framework for this project. The TRA was developed and introduced in 1967 by[20] to explain the relationship between attitudes, beliefs, and behavior. It has been used to explain and examine health behavior. Described as an expectancy theory, an overall assumption is that people are rational individuals, capable of processing information, and making decisions based on available information or knowledge. It proposes that people are more likely to perform a behavior when they are in control of the behavior, have facilitators to enhance engaging in behavior like knowledge about the behavior, the outcome, and benefits, and consequences of not engaging in behavior. Knowledge related to various aspects of the behavior enhances control, attitude towards the behavior, and the value placed on the outcome of the behavior. In the TRA, Fishbein contends that attitude towards a behavior is a much better predictor of that behavior and that a positive attitude enhances behavior[20].Therefore, if a pregnant woman has adequate knowledge about nutrition, and the effect of nutritious eating on the newborn, pregnancy, and postpartum period, her attitude would be positive towards nutritious eating, enhance making healthy food choices, and gaining weight within the IOM guidelines. Gaining knowledge about nutrition, appropriate weight gain during pregnancy, and obesity related risks would equip pregnant women with the resources to control and achieve the desired outcomes of pregnancy. Another construct determining behavior isbehavioralcontrol[2],[3]. Behavioral control is the ability to engage in the desired behavior. Facilitators of control include knowledge about the desired behavior or attributes related to the behavior and, availability of financial resources. Reference[2] contends that knowledge enhances compliance with the behavior. Financial facilitators via WIC vouchers are available during pregnancy in this population. Therefore, if pregnant women are knowledgeable about nutrition, appropriate weight gain during pregnancy, and obesity related risks and possess facilitators to engage in nutritious eating behavior, they would be more likely to engage in nutritious eating during pregnancy. They are in control of their eating behavior because they are better able to make good decisions based on knowledge and can afford quality food choices. See Table 3 for the Theory of Reasoned Action Concepts and Figure 1 for the Theory of Reasoned Action Model.
|
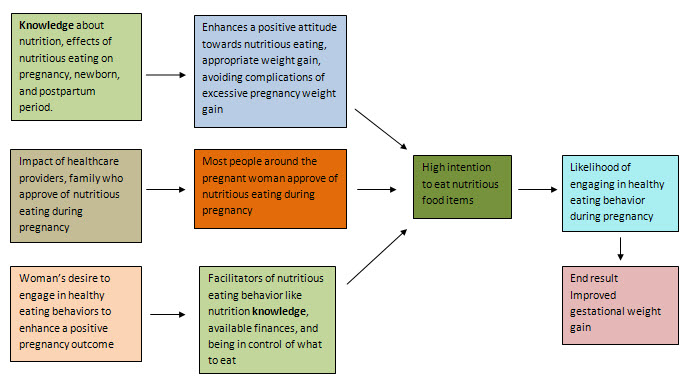 | Figure 1. Theory of Reasoned Action Model,[20] |
3. Review of the Literature
- From the review, there were two approaches to gestational weight management: community and individualizedinterventions. The most effective interventions included community nutrition education and counselling programs that focused on the quality of food instead of quantity of food, the importance of meal planning to avoid high fat consumption, and the importance of increasing physical activity during pregnancy. Other individualized interventions identified were one – on – one instruction and counselling, developing individual weight management plans with emphasis on making low fat food choices, calorie composition, and increased protein in the first trimester of pregnancy[55]. Educational instruments included individual weight gain graphs based on pre-gravid BMIs, nutrition brochures with the food guide pyramid for “moms”, food diaries, and community food preparation demonstrations.Reference[5] conducted a Randomized Controlled Trial (RCT) between October 2005 and April 2007, to examine the effects of a consistent, organized program of dietary education and counselling to prevent excess gestational weight gain in a racially diverse low income population of (n = 100) women. Overall, the treatment group experienced a 28.7 pound decrease in weight compared to a 35.6 pound weight gain in the control group, p = .01. An educational intervention about diet and nutrition, caloric content of food items, exercise, IOM recommended weight gain was included in the intervention. The 1990 IOM guidelines were used to determine the proportion of women whose weight gain was within the IOM guidelines for the duration of the pregnancy. Secondary outcomes included neonatal weight, cesarean deliveries, gestational diabetes, difficult deliveries and vaginal lacerations. A normal pre-gravid BMI was the most predictive factor in adherence to weight gain guidelines and avoidance of poor pregnancy outcomes like cesarean delivery, gestational hypertension, and gestational Diabetes. Women not adherent to the IOM guidelines had macrosomic babies (>4000 gm. wt.). The education and counselling content was not described in this study.In[53], a RCT was aimed at developing and testinga stepped-care behavioral intervention to prevent excessive weight gain in pregnant normal weight (BMI 18.5 – 24.9 kg/m²) and overweight ( BMI 25.0- 29.9 kg/m² ) low income women (n=110). Women were randomly assigned to the treatment (n=57) and control group (n=53). Women in the control group received the standard nutrition counselling given by the healthcare providers, emphasizing taking a daily prenatal vitamin/iron supplement and eating a well-balanced diet. The intervention group received the routine prenatal care counselling, plus written and verbal information on the following topics: 1) Appropriate weight gain; 2) Exercise during pregnancy; and 3) Healthy eating during pregnancy. Newsletters with prompts on healthy eating and exercise habits were mailed to participants biweekly. A personal prenatal weight gain graph was sent to participants after each prenatal visit and women were provided a stepped-care structured intervention based on their weight gain graphs. For example, if a woman’s graphed weight was out of the normal range for her BMI, she received additional individualized nutrition counselling including a review of the weight gain chart, assessment of current eating and exercise habits, and weight gain goals. If the weight was below normal limits she was referred to the obstetrician for further guidance. The nutrition counselling emphasis ranged from making healthy low fat food choices and avoiding high fat items like fast foods, substituting with healthier items like fruits and vegetables, increasing walking rather than driving short distances, more intensive interventions of a structured meal plan with caloric goals for women who exceeded weight gain goals. The intervention significantly decreased the percentage of normal-weight women who exceeded the Institute of Medicine’s (IOM) recommendations for weight gain (33% vs 58%; p<0.05). In the group of women who were overweight at the initial measure, 59% of the intervention group and 32% of the control group exceeded the weight gain recommendations of the IOM. There was no significant intervention effect on overweight women (p = 0.09). Outcome measures included total weight gained during pregnancy, postpartum weight at the first postpartum clinic visit, fat consumption and energy expenditure postpartum, neonatal birth weight and pregnancy and delivery complications. Pregnancy and labor complications measured were not listed.Reference[8] examined nutrition knowledge, beliefs, socioeconomic status (SES), and diet quality intake among 4,356 adults (2219 men and 2137 women) in the United States. Subjects were obtained from the United States Department of Agriculture (USDA) Continuing Survey of Food Intakes among Individuals (CSFII). This database maintained data on diet and nutrition variables not collected by other surveys, such as the Diet and Health Knowledge Survey (DHKS) which links individual diet and health knowledge, beliefs, and perceptions to food intake. The database represented individuals age 0 - 90 years old. Two main measures of interest in this study were Socioeconomic Status (SES) and education of adults in the database. Nutrition knowledge was measured using an 11 item DHKS tool covering knowledge, beliefs, and perceptions about nutrition and diet. An emphasis was placed on consumption of fruits and vegetables using the CSFII 24-hr diet recalls. A Health Eating Index (HEI) and an Alternate Mediterranean Diet Score (aMED) was calculated for each subject. Analysis showed moderate agreement between the HEI and aMED scores (r= 0.50; p<0.05) with an agreement of 32.2% for age and gender matching on the instruments. There was an association between high SES and consumption of fruits and vegetables and the overall quality of the diet improved for higher SES. There was no association between education status and diet quality in persons with low nutrition knowledge.High education level and high nutrition knowledge were significantly associated with high fruit and vegetable consumption, p<0.10.Based on this study, it was concluded that to improve diet quality, health education should be implemented in conjunction with SES interventions that assist with providing adequate income. The IOM guidelines were used in a[35] quasi - experimental study to educate and counsel pregnant women on exercise, weight gain, and diet in maternity and child health clinics in Finland. Three clinics volunteered to be used as intervention clinics while all other clinics were used as controls. The purpose of the study was to determine if education about diet and physical activity during pregnancy, based on IOM recommendations, could have positive effects on physical activity and, prevent excessive gestational weight gain. Diet, verbal instructions and education about nutrition counselling focused on the importance of increasing portions of high fiber breads, fruits and vegetables, restricting high sugar drinks and snacks to < 1/day, instructions on acceptable weight gain patterns in pregnancy, and a hand out of the IOM weight gain guidelines. Counsellors were public health nurses with different experiences and backgrounds, nurse midwives, child health nurses, and other registered nurses with different educational preparations who received additional training on counselling. Counselling about exercises during pregnancy followed the American College of Sports Medicine Recommendations of 30 minutes of moderate intensity supervised group exercise. Exercise trainers were trained by the research team to lead the exercise.More women in the treatment group exceeded the IOM BMI specific weight gain recommendations (46% vs 30%); however, this group had more women with high pre-gravid BMIs and low education levels at initiation of the study. The counselling and teaching sessions had a positive effect on fiber, fruit, and vegetable intake but had no effect on leisure time exercise (p = 0.04; p = 0.004).Reference[36] carried out a descriptive study to examine if greater nutrition knowledge promoted successful weight loss in a tri-ethnic (67% Hispanic, 18% AA, and 15% white) group of low income overweight and obese mothers with young children. This was a pre-post-test design where a convenience sample of N= 141 subjects were recruited from patients at Public Health Clinics and elementary schools where mothers had children in attendance. The mothers who met the criteria completed a demographic and nutrition knowledge questionnaire and attended eight weekly weight loss classes where diet, physical activity, and behavior modification were emphasized. The nutrition knowledge covered six areas: 1. prenatal nutrition; 2. child nutrition; 3. vitamins and minerals; 4. macronutrients; 5. weight loss; and 6. the food guide pyramid. The participants’ knowledge increased in all six areas and mothers with a weight loss > 2.27 kg demonstrated greater overall knowledge than those who did not lose at least 2 kg of weight. Women who lost more weight had higher pre-test (r=0.31; p<.001) and post-test (r= 0.34 p<.001) knowledge scores. Mothers who did not lose weight only demonstrated improved knowledge scores in two areas versus all six areas for those whodid[36].According to[36], Caucasian women improved their pre-post test scores by 11%, compared with a 20% and 36% improvement in Hispanics and African American women, respectively (p<.05). No significant differences inknowledge were observed based on initial BMI categories. Mothers who did not skip meals and attended childbirth classes had higher pre-test scores (68%; p<.01), than those who did not (56%; p <.05). This study’s findings support reinforcement of information on the Food Guide Pyramid, energy nutrients, vitamins and minerals in WIC and low incomepopulations [36]. Reference[28] conducted a pilot randomized study to examine whether a goal setting contract enhanced the effectiveness of the Expanded Food and Nutrition Education / Food Stamp Nutrition Education Program (EFNEP/FSNEP) to increase fruit & vegetable consumption in low income women in seven California counties. Participants were randomized into a three group parallel arm study. The control group received lessons on life skills; one treatment group received lessons on the Food Guide Pyramid series used by the California EFNEP/FSNEP; the other group received the education intervention, plus completed a contract to change their nutritional habits and were reminded of their goals in subsequent nutrition classes. Outcome measures were assessed to evaluate the anticipated dietary changes pre and post intervention and one month after intervention. Three tools were used to collect dietary information: 1. the Health Beliefs Questionnaire, a 14-item tool that assessed readiness to change based on Prochaska’s stages of change; 2. a 16-item Food Behavior Checklist that determined food consumption patterns in this population; and 3. The Red Hutchinson Food Frequency Questionnaire using the 5-a-day method to estimate intake of fruits and vegetables. The effects of the dietary education intervention/ contract on the stage of dietary change – (fruits & vegetable intake) were statistically significant at the p< .05 level when compared to both the control and education only groups. Continued change at follow up was observed in the contract group.The findings from these studies demonstrate thatknowledge and education enhance behavior related to diet and nutrition in prenatal women. However, knowledge alone does not produce the desired effect of making good food choices to prevent excess weight gain and obesity in later life. Other psychological factors such as personal beliefs, attitudes, resources, and the environment may also play a role in long-term behavior changes.
4. Methodology
- The purpose of this study was to determine the impact of education about nutrition, recommended pregnancy weight gain, and obesity health risks on actual weight gained during pregnancy and selected prenatal outcomes among low income women. Specific project aims were: 1) educate pregnant women regarding appropriate nutrition during pregnancy, recommended Institute of Medicine (IOM) weight gain guidelines and obesity associated risks; 2) determine the relationship between education and actual maternal weight gained during pregnancy; and 3) determine the relationship between education, fundal height measurements and maternal blood pressure during pregnancy.
4.1. Study Design
- This quality improvement project used a two-group study to compare outcome measures of maternal weight, maternal blood pressure, and fundal height measurements post educational intervention. The intervention group was a convenience sample drawn from participants at the Peach State Women’s Healthcare Clinic (PSWHC). The control group was drawn from a retrospective chart review.
4.2. Control and Intervention Groups
- The intervention group was identified during the two week period that the educational intervention was offered at the PSWHC from prenatal care clients who provided consent and met the inclusion criteria. The inclusion criteria were: women, age 21-35 years, who were in the first or second trimester of pregnancy with a healthy singleton pregnancy, a Medicaid recipient, and could speak and read English. The exclusion criteria included being on special diets (prescribed or self-imposed), taking medications with side effects of weight gain or loss, a complicated pregnancy, or twin pregnancy. All participants who met the inclusion criteria were offered the opportunity to participate in the study. It was projected that the intervention group would consist of 20 to 30 subjects based on the average daily number of women seen at the PSWHC. During the two week period (10 days) that the education intervention was provided, 3 to 5 prenatal care clients met the inclusion criteria and 2 to 3 of those consented daily to participate for a total of 30 eligible participants. Seven subjects partially completed or did not complete the informed consent and demographic form processes, or delivered prior to completion of visit #4 and were dropped for a total of 23 participants in the intervention group. The control group was a historical comparison group obtained from a sequential retrospective chart review of women who received prenatal care at PSWHC and delivered prior to the start of the education intervention. Charts of women who delivered the day prior to the start of the educational intervention were reviewed to identify women who met the inclusion criteria with the exception of trimester of pregnancy. Each chart was matched with a member of the intervention group based on race, maternal age, gestational age at the beginning of prenatal care, and maternal pre-gravid BMI. If the chart review yielded a woman who could not be paired with a member of the intervention group, that chart was skipped and the review continued until each member of the intervention group had been matched to a client identified through the sequential retrospective chart review.
4.3. Instrumentation
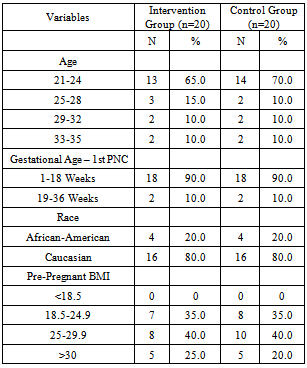
- Tools used to collect data for this project included a demographic survey with a total of eleven items used to describe the demographic characteristics of participants as seen in Table 4. Data collection tables where age, race, blood pressure, fundal heights, weights, and pre-pregnancy BMI measurements were recorded at study entry and at four subsequent corresponding visits were also used to collect data for both groups. Institute of Medicine weight gain graphs, specific to mothers’ pre-pregnancy BMIs, were used to plot participant weights and determine if weight gains at each prenatal visit during the study were within the IOM recommended ranges. A copy was retained in the participant chart for use by clinic providers to graph and monitor weight gain prior to delivery. See sample graph Figure 2 Normal pre-pregnant BMI weight gain graph.
|
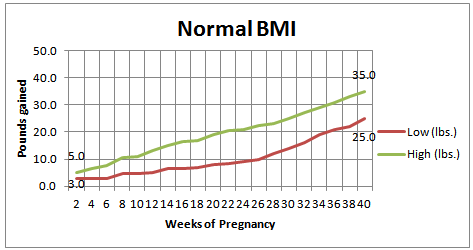 | Figure 2. Normal Pre-Pregnancy BMI Weight Gain Graph |
5. Implementation
- When a patient who met the inclusion criteria arrived for their appointment, the primary investigator questioned the woman either before or after the scheduled visit in a private room to explain the project and determine interest in participation. Once an individual agreed to participate, she was given a study packet and informed that it would take 10 to 15 minutes to obtain consent and review contents of the packet. The study packet contents included a welcome letter describing the study; the informed consent, the March of Dimes(MOD) brochure “Nutrition During Pregnancy”, pre-determined Body Mass Index Weight Gain graphs, an introductory sheet of the MOD video “Healthy Choices: What to Eat During Pregnancy” and, the Demographic Survey. Each prospective participant met one-on-one with the primary investigator before or after the scheduled visit evaluation, reviewed the informed consent, and completed the demographic survey answered questions. The education session was conducted in a private room at the PSWHC with adequate number of seats, lighting and environmental comforts. Another room was available to accommodate other family members and children.The primary investigator reviewed the MOD brochure “Nutrition During Pregnancy” with participant, the brochure contents were discussed and questions answered. The participant’s current visit weights were discussed in relationship to the IOM weight gain guidelines and graphed on the BMI weight graphs. A copy of the graph was retained in the client’s record to be used by clinic primary care providers to plot maternal weights obtained during subsequent visits and review weight gain progress using the graph at each follow up visit until delivery. The primary investigator encouraged participants to watch the MOD video in the waiting area during each subsequent visit to PCWHC.During the data collection period, the schedule of prenatal clients for the day was reviewed to verify if patients that met the project inclusion criteria were scheduled to be seen that day. Each morning of the educational intervention period and for the 2½ month duration of the study, the MOD video “Healthy Choices: What to Eat During Pregnancy” was played continuously in the waiting area of the clinic. Retrospective review of each participant’s chart was carried out to determine actual maternal weights, blood pressure readings and fundal height measurements recorded at follow up visits during the two month period following the conclusion of the educational intervention by the primary investigator. At the end of the 2½ month study period (30 June to 14 September 2010), the comparison group data were obtained via a retrospective chart review to collect demographic data (including age, race, gestational age at initiation of prenatal care, and pre-gravid BMI) and matched intervention subjects. Each chart was matched with a member of the intervention group on age, race, gestational age at the time prenatal care was instituted at PSWHC, and maternal pre-gravid BMI. If the chart review yielded a woman who could not be paired with a member of the intervention group, that chart was skipped and the review continued until each member of the intervention group was matched to a client identified through the sequential retrospective chart review. Data regarding blood pressure, maternal weights, and fundal height measurements over a comparable two months period was obtained and used to compare pregnancy outcomes.
5.1. Setting
- Peach State Women’s Health Care Clinic (PSWHC) is the only prenatal clinic with a Certified Nurse Midwife (CNM) in McDonough, Georgia. The clinic mission is to provide individual and family centered care services that place customers and healthcare relationships first, to the community. Comprehensive care services and choices, that are cost effective and convenient, are offered to women across the lifespan. The vision is to create an environment that empowers staff, women, and families with knowledge about health issues, provide holistic, high quality services that value each customer’s uniqueness and worth. Inherent in the mission and vision are these values: family, building mutually beneficial relationships, collaboration, social engagement, holistic care, communication, caring, learning, integrity, and spirituality. Most staff at PSWHC have more than 10 year’s longevity; the Administrative/IT employee has been with the clinic from its inception. There is one physician and one CNM.The demographic makeup of the community served by the clinic is as follows; Caucasians are the majority race at 62.2%, followed by AA at 34.29%, Asians at 3.5% and Latinos at 1.4%. Women comprise 55.7% of the population [21]. The percent of High School graduates is at 27.1% compared to the city of Atlanta at 11.3%[21]. The median income in this community is between $25,000.00- $70,000.00 per year. This population is a reflection of the patients at the PSWHC where more than 50% are on Medicaid for insurance coverage. The clinic location is next door to the Health Department and provides a referral source for WIC patients. PSWHC accepts private insurance, Medicaid, and self- pay patients.Rationale for the choice of the setting was the fit between project focus, the mission, vision, and values of the clinic. Clinic staff was very supportive of project aims and demonstrated a willingness to provide assistance needed to accomplish project aims.
5.2. Data Collection Methods
- Data were collected using paper and pencil demographic surveys from the intervention participants who met the inclusion criteria and consented to participate in the study. Subsequent data were collected via prospective chart reviews of the intervention participants to obtain weights, blood pressure, fundal height measurements, and pre-gravid BMIs at subsequent visits. The charts of the comparison/control participants were reviewed retrospectively to obtain age, race, weights, blood pressure, fundal height measurements, and pre-gravid BMIs at comparable gestational ages to the intervention participants. Data were coded using sequential numbers from 1i, 2i, 3i etc. and 1c, 2c, 3c to reflect the intervention and control subjects, respectively and entered in data collection tables at study entry and corresponding four visits over the two month period. All data were de-identified at the end of the data collection period, decisions made about outcome variables, and entered into the data collection tables.
5.3. Participants
- At the beginning of a two week period from June 29th to July 13th 2010, a total of 102 patient records were reviewed to identify and compile a list of prospective participants who met the study criteria. A total of 30 patients met the inclusion criteria and 23 participated in the intervention group. To identify the control group, 113 patient charts were reviewed who had received prenatal care from PSWHC in the past and delivered.The majority were Caucasian, age between 21-24 years (69.6%), in the overweight BMI category (43%) Selected control participants were matched on four categorical variables (age, race, pre-gravid BMI and gestational age at first prenatal care visit) to the intervention participants. Demographic characteristics of participants are in Table 4.
6. Data Analysis
- The data analysis for this project was generated using SPSS software version 18 and an Excel program for data analysis.
6.1. Results
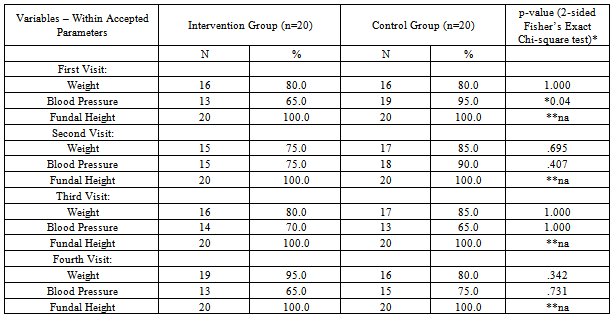
- A total of 46 women were included in the study. Each participant in the control group was matched to one participant in the intervention group on four categories: age, gestational age at first prenatal care visit, race and pre-pregnant BMI. One pair did not match based on the age categories (#23, age 22 & 25 fell in different categories); however, since the age was within 3 years and the two subjects matched on all other categories they were paired. Three pairs did not match on pre-pregnant BMI categories (pair #12, 15, and 22) but were matched on other criteria. 1) Most participants were between 21-24 years of age (65% and 70% of the intervention and control group, respectively); 2) 1-18 week gestational age at first prenatal visit; 3) was Caucasian; and 4) 25-29.9 k/m² pre-pregnant BMI (40% and 40% of the intervention and control group, respectively).There were four study outcomes of weight gain, blood pressure, fundal height and pre-gravid BMI. Each outcome was measured using an ordinal or continuous number then compared to a predetermined acceptable range based on outcome measured and gestational age. Once the outcome variable was compared to the acceptable range, the variable was converted to a binomial variable based on the answer to the question, “Does the variable fall within the acceptable range?” Yes or no. Data obtained on all four variables for the two groups, during four prenatal visits at corresponding gestational ages were analysed in SPSS statistical software version 18. A comparison of groups with outcome variables is shown in Table 5. Actual weight gained was determined by subtracting previous visit weight from current visit weight. If weight gain was more than four pounds and two pounds in the first and second trimesters respectively, the data were categorized as falling outside the parameters of the IOM guidelines, and therefore a “not appropriate” weight gain. The control group had more acceptable weight gain and blood pressure subjects compared to the intervention group. The investigator reviewed participants in the first trimester who began prenatal care at 12 weeks or less.
|
7. Formative Evaluation
- The intervention participants’ knowledge about pregnancy weight gain related to Body Mass Index (BMI), appropriate pregnancy weight gain, and obesity health risks was reinforced by clinic staff on each visit. They enjoyed observing the process of graphing individual weights on the predetermined weight gain graphs, sharing their curiosity to find out their weight status relative to the IOM guidelines. The clinic staff made positive comments about the weight graphs, liked the video for the information provided in an appealing format, but only used the weight graphs sporadically. Upon retrospective review of patient records, the Primary Investigator noted that the weight graphs were not being consistently used during each follow-up visit with women in the intervention group, so it was necessary for the PI to remind the staff and Certified Midwife to use the graphs in designated patient records.
7.1. Summative Evaluation
- Individualized education of patients and matching on four variables is time consuming. When the PI returned to the clinic to answer project related questions from patients and staff, the video was playing in the waiting area and the weight graphs were retained in the patient charts.
8. Discussion
- This education intervention coupled with the use of IOM weight gain graphs did not significantly reduce weight gain during pregnancy in this sample of low income women. Probable contributing factors include: 1) controls had a longer exposure to standard care; from first prenatal visit to delivery, while the intervention participants were exposed to the intervention in the first or second trimester only; 2) small sample size (n = 40) of this project; 3) length of post intervention follow up of intervention participants for two months post intervention compared to follow-up that continued to delivery in similar studies[5],[53], provider’s inconsistent use of the BMI weight gain graphs to monitor weight gain and provide appropriate feedback to women regarding weight gain; 5) over 60% of participants were in the higher BMI categories (overweight plus obese) prenatally, making it more difficult for them to maintain minimal weight gain during pregnancy.In[36] study, participants were exposed to the nutrition education intervention over an eight week period and received continued reinforcement of the education up to delivery. In[5],[8],[36] studies, all study samples were n > 100 participants. The current study sample was n = 40. Post intervention follow up in all reviewed studies was from the first prenatal visit up to delivery. This was not the case in this study. In the study by[53] the use of weight charts improved weight gain of pregnant women within the IOM guidelines. In this study the providers were instructed on use of the BMI specific weight gain charts to calculate appropriate weight gain for patients. The providers were also encouraged to plot the patients’ weight at each visit on the graph and use the plotted weights to reinforce appropriate weight gain with each pt. in the study. However, review of the IOM BMI based weight-gain graphs on the charts of the intervention group indicated that not all providers were consistently using the graphs as instructed. The inability to track active involvement of provider’s use of the weight gain graphs to educate, counsel, and monitor weight gain could have contributed to findings. Previous studies have all indicated that normal pre-gravid BMI and individualized counselling or nutrition education are the most predictive of weight gain within IOM guidelines[36],[53],[5]. In these studies, the findings were compatible with[5] findings that a normal pre-gravid BMI is most predictive of appropriate weight gain during pregnancy. Most participants in the intervention group were in the overweight category for BMI. For example, 65% of women in the intervention group were in the overweight/obese BMI categories. This was the same finding in[35] study. The literature indicates that pre-pregnant BMI is an independent risk factor for excessive pregnancy weight gain in low income populations. This project included a pre-pregnancy BMI category of >30 kg/m². The project findings may have been strengthened by dividing that category into BMI categories of 30-39 and >40 to achieve more similar matches in 3 of the pairings. For example these matches were dissimilar for BMI category pairs #12, BMIs -41.6 & 33; #15- BMIs 35.5 & 23, # 22-BMIs 20 & 29.In[53], where educational interventions positively impacted appropriate weight gain, additional interventions applied, coupled with individualized education sessions. For example, weight gain contracts between study participants and investigators were used, the patients kept tract of their weight on weight gain graphs at home and graphs were monitored by the care providers on subsequent visits. These added interventions were not used in the current study and may have impacted the lack of positive correlation between educational intervention and appropriate weight gain. In[53], the use of weight charts improved weight gain of pregnant women within the IOM guidelines. In this study the providers were instructed on use of the BMI specific weight gain charts to calculate appropriate weight gain for patients. The providers were also encouraged to plot the patients’ weight at each visit on the graph and use the plotted weights to reinforce appropriate weight gain with each patient in the study. However, review of the IOM BMI based weight-gain graphs in the charts of the intervention group indicated that all providers were not consistently using the graphs as expected. The inability to track active involvement of provider’s use of the weight gain graphs to educate, counsel and monitor weight gain could have also contributed to study findings. Other contributing factors to the lack of statistical significance between education and blood pressure measurements in all 4 visits could be related to the fact that some blood pressure values were in the pre-hypertension category, versus the hypertension category as classified by the Seventh Report of the Joint National Committee on detection and prevention of hypertension[50]. Gestational hypertension has been associated with chronic stressors and release of corticortropic releasing hormone (CRH) which prematurely stimulates the physiologic pathways that begin labor and delivery. Chronic stress during pregnancy in this population also induces gluconeogenesis and lipolysis contributing to excess pregnancy weight gain andobesity [67]. Use of a convenience sample may have limited the study, but was offset as much as possible by using a matching control group. Other limitations of this study include a small sample size and inability to generalize findings. In addition, findings may have been more significant if additional interventions such as the food diaries, or self-monitoring contracts had been included in the intervention plan.
8.1. Implications for Practice
- The IOM recommendation that pregnancy weight gain be tracked using pre-pregnant BMIs is not implemented in practice. There are gaps between the evidence and practice in prenatal care services. The use of BMI weight graphs to track and manage weight gain in this population has been successfully documented in the literature[5],[53]. It might have been appropriate to focus on educating the staff and care providers in the use of the IOM weight gain graphs. Individualized education and counselling is time consuming. Therefore, the use of an appropriate tool like the IOM weight gain graph in patient records for weight management and counselling, and a DVD in the waiting area could achieve positive outcomes. Follow up on anecdotal comments about the video and MOD brochure for implementation in the clinic may improve outcomes in the future. When placed within the framework of the Theory of Reasoned Action, findings of this study should be explored for other variables that may have impacted the outcomes of the study. The intervention in this study provided nutrition knowledge and ongoing assessment of weight gain. However, it was not possible to control for financial resources or the attitudes of others close to the pregnant women as part of behavioral intent, or subjective norms. Within each of these components of the TRA, there were variables that could have influenced the choices made by study participants that compromised making good nutrition choices. For example, if the woman already had children, changing the diet may have been difficult for the woman in light of others in the household. If other women surrounding the study participant were not supportive of diet changes or exercise, the pregnant women may have believed that the consequences of excessive weight gain would not affect them because it had not affected others.
9. Conclusions
- Premised on examining the impact of knowledge about nutrition, recommended pregnancy weight gain,complications of excessive weight gain, and obesity related health risks on actual weight gained during pregnancy among low income women, this study set out to educate pregnant women about appropriate nutrition during pregnancy, recommended weight gain guidelines, obesity associated risks, to determine if there is a relationship between education and actual weight gained during pregnancy, and whether or not there is a relationship between education and selected prenatal outcomes. A two group design compared outcome measures of maternal weight, blood pressure, pre-pregnant BMI and fundal height measurements post education intervention among 40 low income women was used. The intervention group was a convenience sample of prenatal care patients who received individualized education about nutrition during pregnancy, obesity risks, and IOM weight gain guidelines. Weight gain was plotted on pre-determined BMI weight gain graphs during 4 visits post-intervention for two months. The control group, derived from a sequential retrospective chart review was matched with intervention participants on four variables. The results indicated no statistical significance between education and study variables except education and first visit blood pressure @ p = 0.04.These findings would lead one to infer that, if a pregnant woman gained excessive weight between prenatal visits, simply counselling and educating her on appropriate nutrition during pregnancy may not be effective. Feelings of frustration and disappointment in progress may lead to a sense of helplessness and powerlessness, further hindering progress towards maintaining the recommended weight. Clinically, gaps exist between evidence and practice in prenatal care. Use of pre - determined weight gain graphs and, consistent individualized education offer successful evidenced based interventions. Knowledge alone did not change eating behavior and consequently weight gain. This finding is consistent with the literature review which indicated that pregnancy weight gain is a multifactorial concept. Therefore, a reinforcement of other contributing factors such as social or family support, readily available food items, Health Care Provider approval of the recommended pregnancy weight gain are significant contributors to maintaining appropriate weight during pregnancy. In future, interventions should be applied in a holistic fashion to assist pregnant women at risk of gaining excessive weight. While nutrition knowledge and weight gain monitoring are important, other activities re-inforce a sense of being in control of gaining appropriate weight. Discussions of how a woman feels about her progress or needs for additional interventions should also be included in clinic visits.
ACKNOWLEDGEMENTS
- Kathy Cannella, M.S., Ph.D., R.N.; Hannah B. Ngwa, M.N., B.S.; Denotra Gaillard, DNP, APRN, FNP-C.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML