-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Obstetrics and Gynecology
p-ISSN: 2326-120X e-ISSN: 2326-1218
2012; 1(2): 15-18
doi:10.5923/j.rog.20120102.01
Pattern of Seminal Fluid Analysis among Infertile Couples in a Secondary Health Facility in South-Eastern Nigeria
Ugboma H.A.A1, Obuna J.A2, Ugboma E.W3
1Department of Obstetrics and Gynaecology, University of Port Harcourt
2Department of Obstetrics and Gynaecology, Ebonyi State University Teaching Hospital, Abakaliki and Mile Four Hospital, Abakaliki
3Department of Radiology, University of Port Harcourt
Correspondence to: Ugboma H.A.A, Department of Obstetrics and Gynaecology, University of Port Harcourt.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
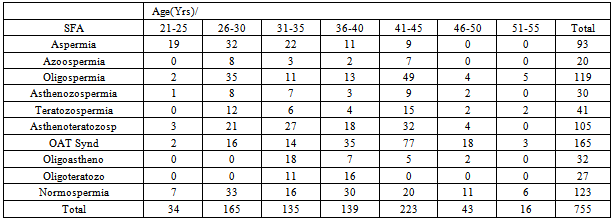
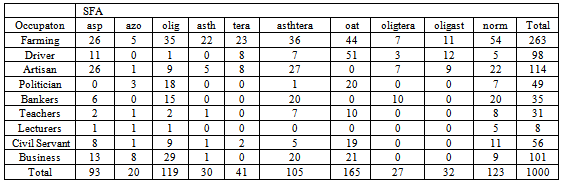
Infertility is increasingly becoming a source of concern among married couples in our environment. The contribution of male factor is assuming a tremendous proportion. This study went out to determine the pattern of seminal fluid analysis among male partners who attended infertility clinic at a secondary health facility over a- five year period. A-five year retrospective review of infertility register at Mile four hospital between July 1, 2005 and July 31, 2010 was undertaken.A total of 776 male partners presented to the infertility clinic during the study period, however, 755 met the inclusion criteria and were recruited for the study. Farmers formed the greatest percentage (34.8%). Lecturers were the least (1.1%). 16.3% had normal sperm parameters. 15.8% had oligospermia. As high as 12.3% had aspermia while azoospermia formed 2.6% of cases. Varicocoele was found in 10.0%. Normospermia was highest in the age bracket 26-30 years (26.8%) and lowest in the age range 51-55 years (4.9%). Abnormal sperm parameters affected all occupation and social class. Male factor is increasingly assuming a significant role in the aetiology of infertility in our environment. Male partners should always be evaluated with their female counterparts.
Keywords: Seminal Fluid, Male. Infertility, Abakaliki
Cite this paper: Ugboma H.A.A, Obuna J.A, Ugboma E.W, Pattern of Seminal Fluid Analysis among Infertile Couples in a Secondary Health Facility in South-Eastern Nigeria, Research in Obstetrics and Gynecology, Vol. 1 No. 2, 2012, pp. 15-18. doi: 10.5923/j.rog.20120102.01.
1. Introduction
- One of the main reasons for marriage is procreation1. Infertility subject couples to great distress[2]. In Africa, women are often blamed while men assumed innocence. In some culture, it is an abomination to declare a man infertile. The blunt of infertility is often ignorantly borne by women[3].The prevalence of infertility is high in sub-Saharan Africa, with a prevalence rate of 20-46% being quoted[2,4]. In Nigeria, various studies report incidence of 20-30 %[5]. In Western countries, 10-15% of couples experience infertility [2]. Male partners directly account for 25-30% of infertility and contribute to another 25 %[2, 6]. In majority of cases of male infertility, the causes of abnormal semen parameters are unknown[2]. However, some of the aetiologies are genital tract infections leading to obstructive azoospermia/oligospermia[6, 7] .Tuberculosis, gonococcal and Chlamydia infections are common in our environment[2, 7]. Bilateral viral orchitis especially after 12 years of age impair sperm parameters[2]. Congenitalabnormality (cryptochordism) and chromosomal disordersalso contribute to sperm abnormality[2].The role of varicocoele is inconclusive. It occurs in 12% of normal men[2,8] .However, studies showed that varicocoelectomyimproved sperm parameters[6,9] . Tobaccos, alcohol, cannabis, drugs and wearing of tight underwear are also implicated[2].The task before an infertility clinic is to make diagnosis of the actual cause of infertility, and seminal fluid analysis (SFA) is very important in this regard[9].Materials and MethodsThis study was carried out at Mile Four hospital, Abakaliki. Mile Four hospital is a mission hospital dedicated to maternal and child health. It has a good microbiology laboratory dedicated to SFA. Couples are encouraged to visit the clinic together. Couples managed for infertility over a-five year period (July 2005-July 2010) were reviewed. Seminal fluid data were reviewed paying attention to semen volume, concentration, motility, morphology and culture results.Modified ‘masturbation’ was the main method of collecting semen in this hospital. Here the wife did the ‘masturbation’ in a dedicated room with dedicated bed and other facilities that made them relax.Some men who lived very close to the hospital were allowed collect at home and brought to hospital within 15-20 minutes. In that case the laboratory scientists were ready for them to analyse the semen immediately within one hour of collection.Masturbation is frowned at by many men for religious reasons. Withdrawal methods and the use of condoms were discouraged. Semen may be lost with withdrawal method or get contaminated with vaginal secretions. Condoms available in our environment are coated with spermicides. Non-medicated condoms (Milex limited) are not available in our environment.Couples are educated on methods of collection and precautions that must be observedInclusion criteria: Men who accompanied their wives to the clinic and did the seminal fluid analysis (SFA).Exclusion criteria: Men who refused to do the seminal fluid analysis.W.H.O criteria for semen analysis are used in this hospital for SFAW.H.O criteria for SFA:• Volume 2ml or more• PH 7.2-7.8• Sperm conc. >20x106 cell/ml• Motility >50% forward movement• Morphology >30% normal form• WBC < 1x106 cells/mlAbnormal sperm parameters:• Aspermia- no ejaculate• Azoospermia-no sperm cell • Oligospermia-<20x106 sperm/ml• Severe oligoserpia-<5x106/ml• Asthenozospermia-abnormal motility• Teratozospermia-abnormal morphology
2. Results
- Seven hundred and fifty five (755) male partners presented to the infertility clinic during the study period and had their seminal fluids analyzed. Aspermia was recorded in 93(12.3%) of cases mostly in the age range 26-30 years (34%). Volumes of less than 2mls was found in 372(49.3%) of cases and greater than 2mls in 290(38.4%) of cases. OAT syndrome was commonest between the age range 41-45 years (46.7%). Abnormal sperm parameters affected all occupations and social class. Positive culture was obtained in 581(77%) and 174(23%) had negative cultures.Testicular sonogram using a 7.5MHZ probe showed that 10% of participants had varicocoele.
|
|
|
|
3. Discussion
- The high number of men 755(97.3%) who presented to the clinic in company of their wives and did seminal fluid analysis as against the 21(2.7%) that refused or failed to do the SFA was in contrast with report from other centers which tend to state that African men do not like to do SFA[7, 9] The result can be attributed to good counseling from the gynaecologists and encouragement from fellow men attending the infertility clinic.Moreso, there is increasing awareness that infertility is a problem of the couple and not of a woman only.The high incidence of aspermia may be attributed to obstruction of the genital tract from high infection rate observed in this study. Genital tract infection is high in our environment and is a common cause of infertility[6, 7]56.2% had low semen volume and compares with report from other workers[7, 8] Low semen volume impairs sperm biochemicalinteractions and vehicular movement of spermatozoa[11]. 16.3% had normospermia by W.H.O standard[12]This is lower than the result from Maiduguri (54%)[11]. the lower result may be influenced by sample size. Laboratory influence may also contribute. 21.9% had abnormality in the three sperm parameters: concentration, motility and morphology. The threeparameters are good predictors of fertility potential of given semen [11]. OAT syndrome has poor prognosis with conventional therapy requiring assisted reproductive technology (ART) which is not readily available in our environment and the few available ones are not within the reach of many infertile couples. The prevalence of oligospermia and azoospermia is 15.3% and 2.6% respectively in this study. This is lower than results from other studies[7, 11,13, 16]. Sample size and laboratory influence may be responsible for this disparity. Also, our stringent measures and close supervision of both semen collection and laboratory techniques may also be responsible for the disparity. Some people have proposed 10x106 sperms/ml as the lower limit instead of 20x106/ml[14] The contribution of varicocoele to this is inconclusive. In our tropical environment with its attendant heat,varicocoelectomy has been found to improve sperm parameters[7, 10].There was lower prevalence of abnormal sperm motility in this study (44%) as opposed to 60% and 54% reported by other workers[9, 16]. The laboratory scientists in Mile Four were carefully trained and are dedicated to doing the SFA. At Mile Four hospital we insist that all semen must be analysed within an hour of collection. Exposure to latex, heat, spermicides and delay in analysing semen may lead to spurious results[8].Seventy-seven percent (77%) had positive culture. Staphyloccocus aureus accounted for greatest proportion. This compares with other studies[6,7,8,11]. The high infection rate may reflect penile contamination. It may also reflect true infection which accounts for the high abnormal sperm parameters in this study[17].
4. Conclusions
- There is high male infertility rate in our environment. There is the need to evaluate male partner in any infertility case[18]. Government, Non-Governmental Organizations (NGO), and donor agencies should assist in theestablishment of ART facilities in this part of the world.
References
| [1] | Genesis 1:28. The holy bible, Authorized King James version. Evangel publisher’s ltd, slim line Ed, 2008. Page 13. |
| [2] | Siladitya Bhattacharya. Infertility. In: D.K Edmonds (Ed). Dewhurst’s textbook of Obstetrics & Gynaecology for Ppostgraduates 7th ed. Oxford Blackwell publishing, 2007. Pp 440-460. |
| [3] | Ojiyi EC, Dike EI, Anolue BU, Okeudo C, Uzoma OI, Uzoma JI. Male factor subfertility at the Imo state university teaching hospital, Orlu. The Internet journal of Gynecology and Obstetrics. 2012; 16(1): 1-6. |
| [4] | Belsey MA. The epidemiology of infertility: A Review with particular references to sub-Saharan Africa. Bull. World health organization. 1976, 54: 321. |
| [5] | Otubu JAM. Infertility. In: Agboola (Ed). Textbook of Obstetrics and Gynaecology for Medical student’s vol. 1. University services educational publishers limited, Lagos, 1998. Pp172-188. |
| [6] | Ekwere PD, Archibong EI, Bassey EE, Ekabua JE, Ekanem EI, Feyi-Waboso P. Infertility Among Nigerian couples as seen in Calabar. Port. Med.Journ 2007; 2(1): 35-40. |
| [7] | Mandong BM. Histological Pattern of testicular biopsies in Nigerian men (undergoing investigations for infertility in Jos, Nigeria). Highland Med Research Journ 2002; 1(1): 7-8. |
| [8] | Ibekwe PC, Mbazor JO. Semen evaluation of infertile couples in Abakaliki, Nigeria. Ebonyi Med Journ 2002; 1(1): 33-37. |
| [9] | Olatunji AO, Sule-Odu AO. Pattern of infertility cases at a University hospital. West Afri J. Med 2003; 22(3): 205-207. |
| [10] | Glezerman M, Bartoov B. Semen Analysis. In: Infertility: Male and Female (vol.1) 2nd ed. Insler V, Lunenfeld B (Ed), Churchhill Livingstone 1993, pp 285-311. |
| [11] | Okon KO, Nwaogwu M, Zailani SO, Chama C. Pattern of Seminal fluid indices among infertile male partners attending the infertility clinic of University of Maiduguri Teaching Hospital, Maiduguri, Nigeria. Highland Med Research Journ 2005; 3(1): 18-23. |
| [12] | WHO Laboratory manual for the examination of human semen and sperm cervical mucus interaction 4th ed. Cambridge University press, Cambridge, 1999. |
| [13] | Yeboah ED, Wadhwani JM, Wilson JB. Aetiological factors of male infertility in Africa. Int. J. Fertile 1992; 37: 300-7. |
| [14] | Mallidis C, Howards EJ, Baker HWG. Variation of semen quality in normal men. Int. J. Androl. 1991; 14: 99-107. |
| [15] | Small DR, Collins JA, Wilson EH, Wrixon W. Interpretation of semen analysis among infertile couples. C MAJ 1987; 136: 829-33. |
| [16] | Adetayo FO, Osegbe DN. Semen Parameters in Infertile Nigerian Males: A Critical Study. Nig Quarterly J. Hosp Med 2005; 15(2): 87-91. |
| [17] | Ugboaja JO, Monago EN, Obiechina NJ. Pattern of semen fluid abnormalities in male partners of infertile couples in southeastern, Nigeria. Nier J Med. 2010; 19(3): 286-288. |
| [18] | Dolores J Lamb. Semen analysis in 21st century medicine: the need for sperm function testing. Asian Journal of Andrology. 2010; 12: 64-70. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML