-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research In Cancer and Tumor
2025; 12(2): 21-26
doi:10.5923/j.rct.20251202.01
Received: Sep. 5, 2025; Accepted: Sep. 29, 2025; Published: Oct. 13, 2025

Comparative Characteristics of Visualization Methods in the Diagnostics of Benign and Malignant Breast Formations
I. Z. Pulatova, Ya. M. Mamadalieva, Kh. Kh. Khushnazarov
Center for Professional Development of Medical Workers, Tashkent, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of this study was to investigate the possibilities of applying a multimodal radiation approach to the differential diagnostics of breast tumors in a comparative aspect. Background. Breast cancer is one of the central problems of clinical mammology – the medical science of diagnosing, treating, and preventing diseases of the mammary glands. Early diagnostics of breast cancer at the preclinical stage of development remains one of the priority tasks in oncology. Material and methods. This prospective study included 197 women with focal breast diseases at the age from 28 to 76 years. The mean age of the patients was 52±4.3 years. The diagnostic algorithm included step-by-step studies with BIRADS system protocoling. Results. Detailed B-mode ultrasound imaging revealed 224 focal tumor lesions in 197 women. The average stiffness coefficient of formations in category BIRADS 3 was 2.32±0.12, BIRADS 4 – 4.63±0.28, BIRADS 5 – 6.12±0.27. Discussion. We determined that increasing age was a risk factor for the development of malignant tumors (χ2=11.25, OR=8.4; p=0.002), which had a direct impact on the increase of BIRADS category. Age between 40 and 60 is a crucial factor in the development of malignant neoplasms in women, which is associated with hormonal changes occurring due to premenopausal and menopausal changes in the female body. Conclusion. Using a comprehensive approach to diagnosing breast tumors can provide a more comprehensive assessment of the formations nature, which is important for accurately identifying malignant tumors and minimizing false positive results.
Keywords: Breast cancer, Differential diagnostics, Early diagnostics, Multimodal radiation approach
Cite this paper: I. Z. Pulatova, Ya. M. Mamadalieva, Kh. Kh. Khushnazarov, Comparative Characteristics of Visualization Methods in the Diagnostics of Benign and Malignant Breast Formations, Research In Cancer and Tumor, Vol. 12 No. 2, 2025, pp. 21-26. doi: 10.5923/j.rct.20251202.01.
Article Outline
1. Introduction
- Breast pathology continues to occupy a leading position in the structure of overall female morbidity. The spectrum of focal breast pathology is quite broad and varies from inflammatory and benign formations to malignant ones [1-3].Breast cancer is one of the central problems of clinical mammology – the medical science of diagnosing, treating, and preventing diseases of the mammary glands. Early diagnostics of breast cancer at the preclinical stage of development remains one of the priority tasks in oncology [4-5].The diversity of clinical presentations and the complexity of differential diagnostics for breast diseases require the use of modern, highly informative diagnostic methods. It involves searching for additional research methods to optimize existing diagnostic methods, taking into account the improvement of their efficiency [6-7].Traditional ultrasound diagnostics (US) in B-mode combined with mammography (MMG) are widely used in the clinical screening of breast cancer and are also methods for the differential diagnostics of benign and malignant breast tumors [1,8].A multimodal approach is the only correct solution in diagnostic mammology. Mammography, B-mode ultrasound and ultrasound elastography are the most common non-invasive imaging methods used to detect breast lesions [9-10].Mammography is the basic method for objective evaluation of breast condition and differential diagnostics. Modern digital mammography technology is highly sensitive and allows for the detection of breast formations at the preclinical stage of their development. However, differential diagnosis of some pathological processes is difficult, especially against the background of increased tissue density of the gland. It often leads to false conclusions and, consequently, to a delay in detecting a malignant tumor or an unjustified biopsy in the case of a benign process [11-12,10].Elastography, which is a non-invasive method that allows determining the stiffness of the area of interest has been actively used in recent years as a new direction in ultrasound imaging [4,13]. This technique can significantly improve the differential diagnostics of benign and malignant breast tumors, avoiding unnecessary biopsies [7]. Two types of elastography techniques are used: compression elastography and shear wave elastography. The reporting system and mammary gland image data, according to the BIRADS classification, integrated with subsequent innovative ultrasound methods, have led to better characterization of mammary gland tumors. However, some focal formations demonstrate overlapping ultrasonic features of both malignant and benign origin, and histopathological correlation becomes the definitive test for the final diagnosis [12].Unfortunately, each method has its limitations and drawbacks. Differential diagnostics of certain pathological formations is a difficult task for radiological diagnostic methods, since small sizes and unclear radiological characteristics often do not allow determining the malignant nature of changes.The aim of this study was to investigate the possibilities of applying a multimodal radiation approach to the differential diagnostics of breast tumors in a comparative aspect.
2. Material and Methods
- This prospective study included 197 women with focal breast diseases aged 28 to 76 years who were treated at the Tashkent Regional Branch of the Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology for the period from 2021 to 2024. The mean age of patients was 52±4.3 years. The patients' complaints were as follows: painful sensations, feelings of fullness, and palpable formations in the mammary glands. All patients were divided into two groups according to age: Group 1 (n=67) included women up to 39 years of age, accounting for 33.9% of the total number of patients;Group 2 (n=130) consisted of women over 40 years which corresponded to 66.1%. The diagnostic algorithm included step-by-step examinations with logging according to the BIRADS system.All patients in group 1 underwent standard gray-scale ultrasound examination and elastography in two modes: compression elastography and shear wave elastography. In case of suspicious ultrasound results, women of Group 1 underwent X-ray mammography. Patients of Group 2 underwent X-ray mammography followed by ultrasound examination (B-mode and elastography). Ultrasound examinations were performed using Logiq E10 expert-class devices (GE Healthcare, Milwaukee, WI, USA) with transducers with a frequency range of 9–24 MHz. Using standard ultrasound diagnostics in B-mode, the following criteria were assessed: shape, contours, size, number of formations, boundaries, presence of acoustic shadow or micro-calcifications, spatial orientation.Then, compression elastography was performed by applying gentle repetitive compression with a transducer. The upper boundary of the area of interest on elastographic images was set to include subcutaneous fat, and the lower boundary of the area of interest was set to include the pectoral muscles; the lateral boundaries were set at a distance of more than 5 mm from the tumor boundary. Compression elastography data were recorded in color gradation, and the strain ratio (SR) was calculated. Both qualitative and quantitative characteristics were evaluated during compression elastography. A qualitative indicator of stiffness was evaluated based on the color pattern of the formation, according to the classification by A. Itoh and E. Ueno [14]. There are 5 elastotypes according to this classification: Type 1 – a solid formation is colored identically to the surrounding tissues with the presence of isolated, permissibly altered color signals.Type 2 – characterized by mosaic coloring of the formation with alternating blue and green shades.Type 3 – blue color is observed mainly in the central part of the formation, and the peripheral part has a green pattern.Type 4 - a solid formation is mapped in a completely uniform blue color.Type 5 – the formation is stained blue with a color transition to the surrounding tissue.A separate elastotype (0-type) is used to mark cavity formations that have a three-layer coloration: blue-green-red (BGR).For quantitative characterization of elastography, the strain ratio (SR) was calculated, with a threshold value of 4.0 adopted in accordance with European EFSUMB recommendations. If the formation had three or more suspicious ultrasound criteria in B-mode, as well as 4-5 types of elastograms and a strain ratio (SR) greater than 4.0, then this focus was classified as malignant. Elastographic images were generated without compression during shear wave elastography. The default region of interest size was 2.5 × 1.5 cm, with a maximum size of 3 × 2.5 cm. All results of gray-scale ultrasound and sonoelastography indicators were compared with the results of morphological examination.X-ray mammography was performed in two projections: direct and oblique. During the imaging, each breast was placed one by one on a special platform of the device, and the upper plate lightly pressed the breast to evenly distribute the tissue and improve the quality of the image, which also helps to reduce the radiation dose. During mammography, the following parameters were assessed: localization of nodular formations, shape, contours, quantity, presence of deformation and change in the structuring of the mammary gland, tissue thickness and density, presence of calcifications or microcalcifications. Statistical analysis of the data was performed using the Statistics 6.1 program. The data are presented as M±σ, where M is the arithmetic mean; σ is the standard deviation. Categorical variables are presented as absolute number and percentage (%), continuous variables as mean ± standard deviation and median. The normality of data distribution was tested using the Kolmogorov–Smirnov test.
3. Results
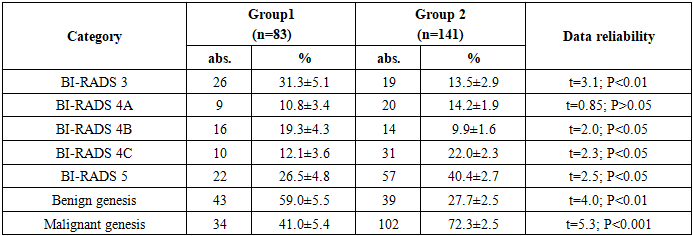
- Detailed B-mode ultrasound imaging revealed 224 focal tumor lesions in 197 women. There were 83 (37.1%) focal breast lesions in 67 women in group 1 and 141 (62.9%) tumors in group 2, respectively. According to the BIRADS classification, patients in Group 1 were distributed as follows: category 3 – 26 (31.3%), category 4A – 9 (10.8%), 4B – 16 (19.3%), 4C – 10 (12.1%), category 5 – 22 (26.5%). There were 49 (59.0% of 83) benign cases and 34 (41.0% of 83) malignant cases. The following trend was observed in group 2: BIRADS 3 – 19 (13.5%), BIRADS 4A – 20 (14.2%), 4B – 14 (9.9%), 4C – 31 (22.0%), BIRADS 5 – 57 (40.4%). Among them, 39 (27.7% of 141) and 102 (72.3% of 141) benign and malignant tumors were found, respectively (Table 1).
|
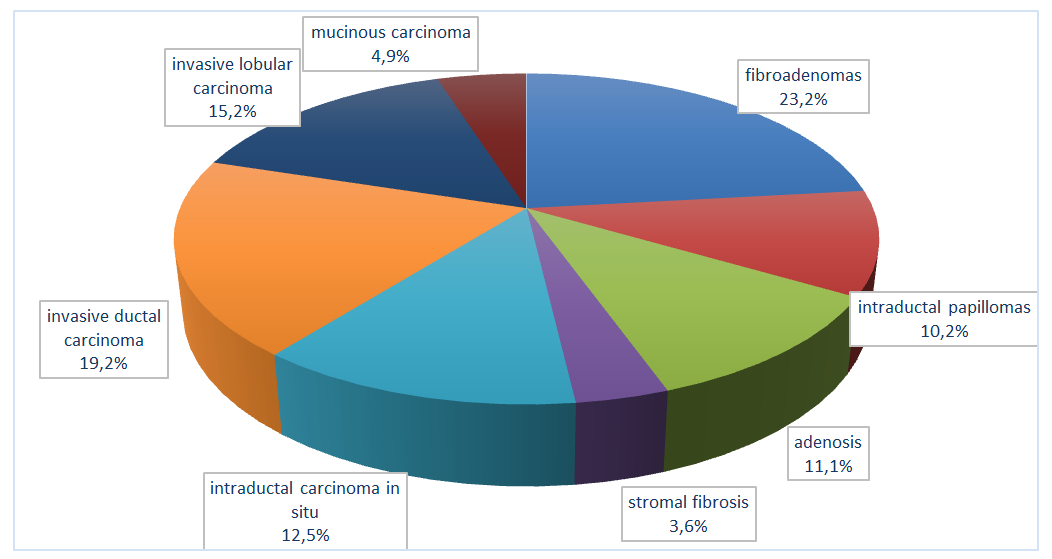 | Figure 1. Distribution of patients according to morphological findings |
 | Table 2. Distribution of elastotypes of focal lesions in the mammary glands of the BIRADS category 3-5 |
4. Discussion
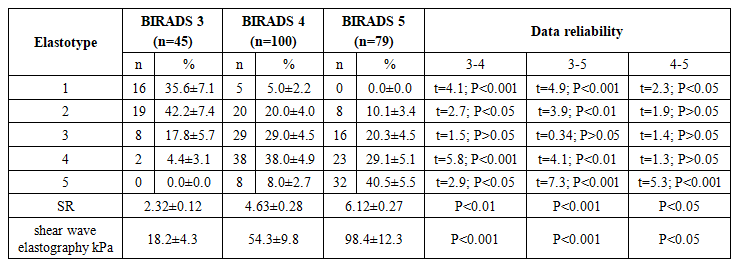
- When diagnosing breast cancer, it is necessary to pay attention not only to clinical data, but also to their connection with the mandatory skills of interpreting the results of breast ultrasound and mammography. The multimodal radiological approach means that the doctor conducting the initial appointment must clearly know the purpose and sequence of the diagnostic algorithm, which includes step-by-step studies with protocoling according to the BIRADS system [15,14,16].In our study, we found that increasing age is a risk factor for the development of malignant tumors (χ2=11.25, OR=8.4; p=0.002), which had a direct impact on the increase of the BIRADS category. Our data are consistent with the studies of Chesnokova N.P. and co-authors (2018), Alghamdi I.G. and co-authors (2018) and Nadia Srur-Rivero, Mayra Cartin-Brenes (2024), who found that age from 40 to 60 years was the most important factor in the development of malignant neoplasms in women, which was associated with hormonal changes occurring due to pre-menopausal and climacteric changes in the female body [2,17,8].The use of the BIRADS classification in ultrasound diagnostics facilitates the assessment of the risk of breast tumor formation, while reducing the frequency of false diagnoses [14]. In our studies, the BIRADS-1 category corresponds to normal, unchanged breast tissue; we did not include this category in the study. In the BIRADS-3 category, all formations (n=45) had a benign genesis, and the results of compression elastography were 2 times lower than in the BIRADS-4C category (n=41), and shear wave elastography were 2 and 3.5 times lower than in the category with BIRADS-4B and 4C formations, respectively. In category 4 of 73 focal formations, 10 (13.7%) tumors were benign, and 63 (86.3%) were malignant. In the study by Shen Y. et al., the diagnostic accuracy was significantly improved by combining the BIRADS classification with elastography and contrast-enhanced ultrasound. The combined approach allowed to get a sensitivity of 88.5%, a specificity of 87.0%, a positive predictive value of 80.0%, a negative predictive value of 92.8%, and an accuracy of 87.5%. It is noteworthy that 55.8% of BIRADS 4A nodules were classified as BIRADS 3 and confirmed as benign after pathological examination, thus allowing the avoidance of unnecessary biopsies [12].Using a comprehensive approach to diagnosing breast tumors can provide a more comprehensive evaluation regarding the nature of the formations, which is important for accurately identifying malignant tumors and minimizing false positive results. Our results are consistent with those of other studies, confirming the importance of comprehensive ultrasound diagnostics in clinical mammology [10].Our results are consistent with those of other studies, confirming the importance of comprehensive ultrasound diagnostics in clinical mammology [10]. Our study found that in compression elastography, the stiffness coefficient for BIRADS 3 lesions was 2.32±0.12, for BIRADS 4 lesions it was 4.63±0.28, and for BIRADS 5 lesions it was 6.12±0.27. In shear wave elastography, the values were as follows: BIRADS 3 – 18.2±4.3 kPa; BIRADS 4 – 54.3±9.8 kPa; BIRADS 5 – 98.4±12.3 kPa. The obtained data showed a correlation dependence: the rigidity of focal lesions in the mammary glands increased (r=0.852; p=0.002) with an increase in the BIRADS category.X-ray mammography is one of the main methods for detecting oncological diseases of the mammary gland, which allows identifying the presence of calcifications, cysts, fibroadenomas and other neoplasms in the tissues of the mammary gland. According to randomized studies conducted abroad, mammography can diagnose about 75% of breast cancer cases among women aged 40-50 years and up to 90% among women aged 50 years and older [3,19]. According to the conducted studies, anomalies detected during mammography include volumetric formations, clusters of microcalcifications, general and local asymmetry in the form of structural reorganization of the breast tissue. The most significant sign of malignancy is a formation with uneven, radiant contours - more than 90% of cases. Cluster accumulation of microcalcifications, as a manifestation of intraductal necrosis of tumor cells, occurs in 60% of cases of cancer. Well-defined seals are highly likely to indicate a benign process (cyst, fibroadenoma, lymph node), while there are often exceptions when carcinoma, sarcoma or lymphoma may appear as a well-defined formation [10,1,16]. Frequency of microcalcifications in our study were detected in 7.7% of benign and 66.1% of malignant lesions. Macrocalcifications were identified in 18.5% of benign lesions and in 9.3% of malignant nodules. Nipple retraction was not observed in any of the benign lesions, but was noted in 22.9% of malignant lesions. Skin thickening in malignant breast tumors was observed in 18.5% of patients. Changes in architecture and the presence of glandular tissue heaviness were observed among malignant formations in 30.5% of cases.
5. Conclusions
- Thus, the use of a comprehensive approach in the diagnostics of breast tumors can provide a more comprehensive evaluation of the nature of the formations, which is important for the accurate detection of malignant tumors and the minimization of false positive results. Our results are consistent with those of other studies, confirming the importance of comprehensive ultrasound diagnostics in clinical mammology.
Ethical Approval and Consent to Participate
- Our institution's research ethics board does not require review or approval of case reports.Our investigation is conducted in accordance with the World Medical Association's Code of Ethics (Declaration of Helsinki).
Source of Funding
- Each author has reviewed and approved this manuscript. None of the authors has any conflict of interest, financial or otherwise. This manuscript is original, no part of it has been previously published, and it is not being considered for publication elsewhere. The corresponding author agrees to take full responsibility for authorship during the submission and review stages of the manuscript.
ACKNOWLEDGEMENTS
- The authors express their gratitude to the management of the multidisciplinary clinic of Tashkent Regional Branch of the Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology for the material provided for our study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML