-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research In Cancer and Tumor
2022; 10(1): 14-20
doi:10.5923/j.rct.20221001.03
Received: Jul. 13, 2022; Accepted: Aug. 5, 2022; Published: Aug. 23, 2022

Factors Influencing the Time to Presentation, Diagnosis, and Treatment of Patients with Esophageal Cancer at Moi Teaching and Referral Hospital, Eldoret, Kenya
Tabitha Chepkemoi1, Diana Menya2, Naftali Busakhala2
1Kabarak University, Kabarak, Kenya
2Moi University, Eldoret, Kenya
Correspondence to: Tabitha Chepkemoi, Kabarak University, Kabarak, Kenya.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Esophageal Cancer (EC) is a malignancy with high incidence and mortality globally. Late presentation and diagnosis lead to poor outcomes and high cost of treatment. The aim of this study was to describe factors influencing the time to presentation, diagnosis and treatment of patients with esophageal cancer at Moi Teaching and Referral Hospital (MTRH). This was a cross-sectional study conducted on patients with esophageal cancer seeking treatment at MTRH during the study period. Consecutive sampling of the patients in oncology clinic and surgical wards was done until a sample size of 104 was achieved. Logistic regression was used to determine the associations between factors and timelines for presentation, diagnosis and treatment using R-4.1.0-win software. The association was measured using Odds Ratios (ORs) with 95% CI. Monthly income of < 20,000 Kenya shillings (OR=0.1, CI, 0.002-0.52) was associated with late presentation to the health facility after the onset of symptoms. Being widowed (OR 0.05, CI, 0.003-0.39) was associated with late diagnosis while referral from another facility to MTRH was associated with early diagnosis (OR=3.74 CI, 1.08- 14.7). Participants who had no medical insurance were more likely to be diagnosed and treated late (OR =0.3 CI, 0.079-0.82) and (OR= 0.27, CI, 0.079-0.82) respectively. Low income status was associated with late presentation to a health facility. Being widowed and lack of medical insurance were associated with late diagnosis and treatment while referral to MTRH was associated with early diagnosis.
Keywords: Esophageal cancer, Cancer presentation, Cancer diagnosis, Cancer treatment, Cancer stage at diagnosis, Patient -mediated factors, Health system mediated factors, Late presentation, Early presentation
Cite this paper: Tabitha Chepkemoi, Diana Menya, Naftali Busakhala, Factors Influencing the Time to Presentation, Diagnosis, and Treatment of Patients with Esophageal Cancer at Moi Teaching and Referral Hospital, Eldoret, Kenya, Research In Cancer and Tumor, Vol. 10 No. 1, 2022, pp. 14-20. doi: 10.5923/j.rct.20221001.03.
Article Outline
1. Introduction
- Esophageal cancer ranks seventh with reference to incidence (604,100 new cases) and sixth cause of mortality (544,076 deaths) globally [1]. The latter shows that esophageal cancer is responsible for an estimated 1 in every 18 cancer deaths. Of all the esophageal cancer incidence and deaths globally, 80% occur in low and middle -income countries [2,3]. According to GLOBOCAN report [4], esophageal cancer is the fourth most common cancer in Kenya. It causes the highest number of cancer-related deaths in the country killing over 4,000 people annually [5]. The factors influencing the time to presentation, diagnosis, and treatment are summed in a complex interplay between the patient- mediated and health system mediated. Patient-mediated factors are described as factors influencing the time from onset of symptoms to the time of the first presentation to the health facility include demographics, socioeconomic issues, health beliefs, and psychosocial [6]. Health system-related factors include all factors that are influenced by health care providers or the health system in terms of access to healthcare, diagnostic and treatment cost, and referrals [7,8]. Despite being a deadly disease, there have no studies conducted in Western Kenya on the factors related to time of patients’ presentation to health facility for diagnosis and treatment [9]. The aim of the study therefore was to identify factors influencing the time to presentation, diagnosis, and treatment of patients with esophageal cancer at MTRH.
2. Materials and Methods
- Study design and Study population: The study design was a cross-sectional which involved the interviewing of patients with esophageal cancer using a semi-structured questionnaire and the review of their medical records to retrieve information on clinical data. The study population included patients with esophageal cancer seeking medical and surgical treatment at Moi Teaching and Referral Hospital. The study population was patients who were histologically confirmed to be having esophageal cancer seeking medical and surgical treatment at Moi Teaching and Referral Hospital within the study period while those whose records were incomplete and those who have been visiting the clinic for more than 6 months ( to avoid recall bias) [10] were excluded. Sample size determination and Sampling techniques: A sample size of 104 patients was estimated using the formula for the finite population (Daniel 1999) with the following assumptions: 50% prevalence of late esophageal cancer diagnosis, 5% margin of error, Critical value associated with type 1 error 1.96 (95% level of confidence). Patients were recruited using consecutive sampling until the targeted sample size was achieved. Data collection techniques: At the oncology and cardiothoracic clinics, the researcher started from the clinician desk to check on the registers for the patients who were identified as having esophageal cancer. Their names were written down and then they were approached physically on the waiting bay to give consent for the researcher to peruse through their files and to be interviewed. For those who met eligibility criteria, the researcher retrieved the information on clinical data from their files then proceeded to interview them in a secluded area within the hospital. For those who were admitted to the surgical wards cardiothoracic section, the researcher identified the patients with esophageal cancer with the assistance of the nurse on duty. They too were approached to give consent for their file to be perused and to be interviewed if they met eligibility criteria. Data management and analysis: Data was reviewed after collection to check for missing data and unclear entries. Data captured using the structured interviewer-administered questionnaires were entered into an electronic database, MS. Excel. The database was encrypted with a password to ensure confidentiality. Data analysis was done using R-4.1.0-win software. Descriptive statistics was used for demographic characteristics where frequency tables and percentages were calculated. Logistic regression was also used to determine the associations between explanatory factors determining the stage at diagnosis and timelines of esophageal cancer presentation, diagnosis and treatment. The strength of the association was measured using ORs with 95% CI.Ethics: The study sought ethical approval from the Institutional Research and Ethics Committee (IREC) of Moi University, IREC/2019/288. Informed written consent was obtained from all the eligible participants and those who consented were interviewed. Permission was also sought from the hospital administration before the commencement of the study. Informed written consent was obtained from all eligible patients, Information about the research was given verbally to each patient and those that gave a written consent were interviewed.
3. Results
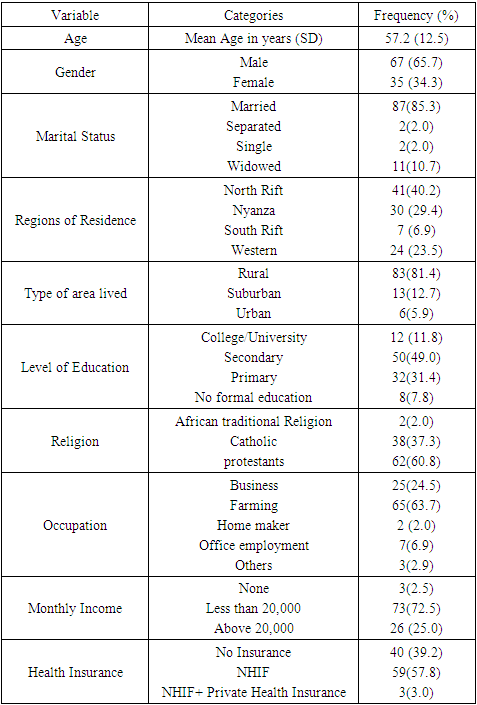
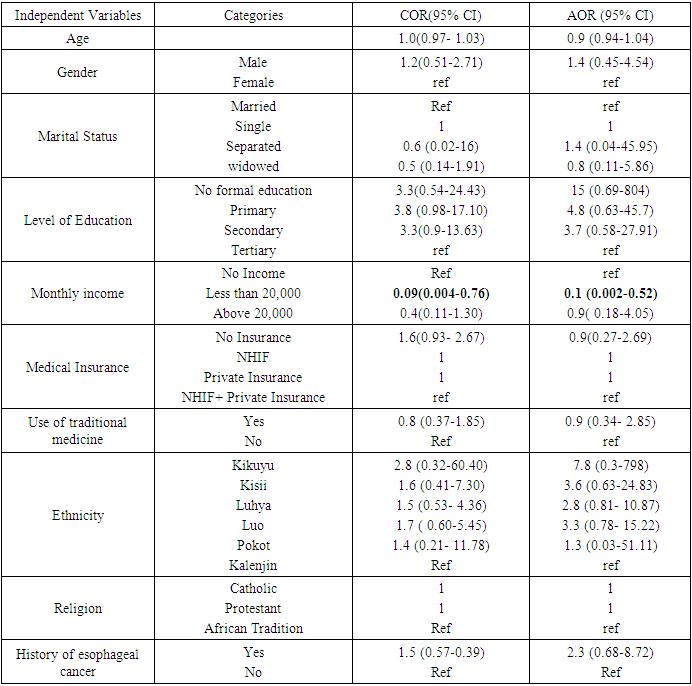
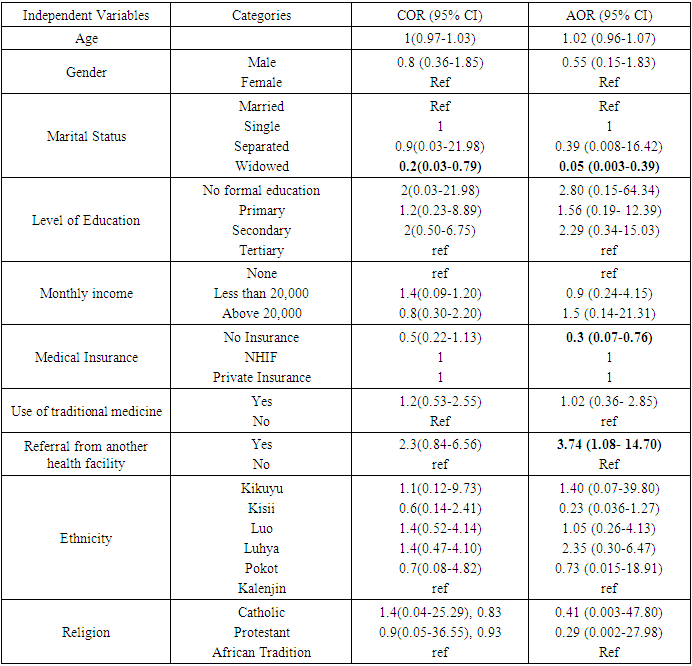
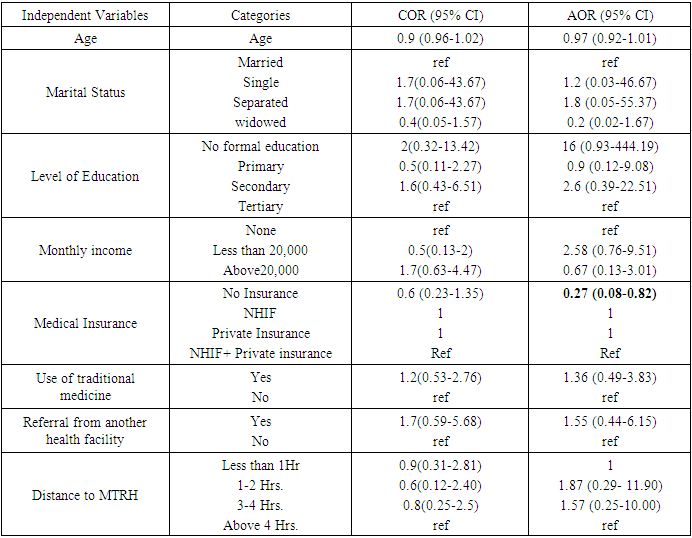
- The mean age of the study participants was 57.2 years (SD, 12.5 years) at the time of study. A majority of participants 65.4% were male, 85.3% married, 81.4% living in rural setting and 40.2% were residents of north rift region. On education, 7.8% were illiterate, with over 60.0% having secondary and above as their highest level of education. On religion, a majority of participants were Protestants 60.8%. Majority of the participants 63.7%, were farmers with 72.5% earning less than 20,000 shillings per month. Most participants 60.8% had medical insurance Table 1. Participants with monthly income less than 20,000 Kenya shillings 0.1 (0.002-0.52) were more likely to present late to health facility after the onset of symptoms Table 2. Being widowed AOR, 0.05 CI (0.003-0.39) and having no medical insurance AOR 0.3 CI (0.07-0.76), were more likely to make participants delay in esophageal cancer diagnosis. Participants who were referred from another facility to MTRH were more likely to be diagnosed early as compared to those not referred AOR 3.74, CI (1.08- 14.70) Table 3. Having no medical insurance AOR 0.27, CI (0.08-0.82), was more likely for a patient to delay for treatment after histological confirmation of esophageal cancer Table 4.
|
|
|
|
4. Discussion
- The study revealed that esophageal cancer is common among the older population; the results were consistent with other published reports [10,11]. The male: female ratio among the patients with esophageal cancers was 1.9: 1, a slightly higher ratio than 1.5:1 found by [12]. The higher male to female ratio may be attributable to higher risk among men such as drinking alcohol and smoking [13]. The distribution of patients with esophageal cancer was high in North rift region which can be explained by the close proximity and accessibility of MTRH. Nyanza region, however, recorded a significant figure supporting previous study that found high incidence rates of esophageal cancer near Lake Victoria [14]. A relatively high number of the participants had low level of education, with a majority in low socio-economic status. Despite the efforts by Kenyan government to increase the NIHF enrollment, the study revealed most participants still had no medical insurance. However, there has been a significant improvement (57.8%) in NHIF coverage overall as compared to 2015-2016 NHIF coverage of about 19% [15]. Factors influencing time to first presentation of patients with esophageal cancerThe study revealed that monthly income was associated with time to presentation of patients with esophageal cancer. Those patients who earned an income of less than 20,000 shillings were 5times more likely to present late as compared to their counterparts who earned more monthly income. This can be explained by structural inequalities in Kenya’s health care, disproportionality influence accessibility where people with high income status seek health care more conveniently [16,17]. Transport cost and other related expenses to medical attention are some of the hindrances to early presentation [14]. Income status is a precursor for social economic status (SES), so people with low SES have poor financial support and less ability to afford medical care prolonging delay time. The results agreed with a study done in China that found an association between social economic status and health care delay in esophageal cancer [18,19,20]. Factors influencing time to diagnosis of patients with esophageal cancerIn our study, widowed patients were 6 times more likely to be diagnosed late in reference to their married counterparts, (OR 0.062, CI, 0.004-0.43). These results were consistent with other studies that have reported an association between being widowed and late esophageal cancer diagnosis as well as higher mortality from esophageal cancer [21,22]. This association may be attributable to social challenges resulting from loss of emotional support, less income, and fewer social relationships as a result of partner loss. The study found a > 2 folds increased risk of being diagnosed late with esophageal cancer among the patients with no medical insurance as compared to those participants who had either NHIF or private medical insurance(OR =0.228 CI, 0.057-0.80). Medical insurance cost in Kenya is high leaving the poor families to pay for diagnostic services out of pockets causing delay in healthcare finance mobilization and negating their health seeking behaviors for esophageal cancer for diagnosis. The government in the recent past has put efforts to improve the NHIF coverage for patients with terminal illness, [14] but more effort is still needed because the percentage of cancer patients who are uninsured is still high. The results were in agreement with a study done by [23], on cost and affordability of NCDs screening, diagnosis and treatment in Kenya who found out that the payments required for cancer diagnostic tests for patients without medical insurance were beyond their reach. The patients who were referred from other facilities to MTRH were 3.74 more likely to be diagnosed early as compared to those patients who were not referred (OR=3.74 CI, 1.08- 2.34). Delay in referral is often related to misdiagnosis of common symptoms, for instance treating heartburns, pneumonia, GERD, and esophagitis among others [24]. Strengthening the referral system has proven to reduce the delays in diagnosis thus improving the overall outcome of the disease. The use of telephone contact or digital referral system is one way to reduce the navigation pathway [25,26]. Factors influencing time to treatment of patients with esophageal cancerHaving no medical insurance, was statistically significant factor to delay in seeking treatment for esophageal cancer after histological confirmation (OR= 0.27, CI, 0.079-0.823). The cost of cancer treatment in Kenya is very expensive, impeding many patients from seeking early treatment [27,28]. The government of Kenya has made positive strides on improving the NHIF care package on cancer treatment including ten chemotherapy sessions, oral and injectable anti-cancers drugs, inpatient and outpatient oncology services, twenty sessions for radiotherapy, and about two sessions for Brachytherapy for advanced cancer, per year [14,15]. It is therefore, evident that having no medical insurance is a huge barrier to early cancer treatment because the patients miss out on the NHIF package that would help in treatment to the cancer. In addition, a medical insurance is an indicator of social economic status aggravating financial constraints in seeking cancer treatment services [21].
5. Conclusions
- Income status influenced the time to presentation of patients with esophageal cancer in MTRH, with low income associated with late presentation to first medical attention. Widowed individuals and lack of medical insurance were associated with late diagnosis while referral to MTRH was associated with early diagnosis of esophageal cancer. Lack of medical insurance was also associated with late treatment of esophageal cancer. These factors’ influence on esophageal cancer burden and overall implications on patient health point to the need for tailored interventions to modify and support positive healthcare seeking behaviors and overall outcome of the disease in the population.
ACKNOWLEDGEMENTS
- We thank God for giving us the strength to carry out the study; we also convey our gratitude to the study participants, and the School of Public Health Moi University for academic guidance.
Disclosure
- Competing interestsThe authors declare no competing interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML