-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research In Cancer and Tumor
2022; 10(1): 1-3
doi:10.5923/j.rct.20221001.01
Received: Feb. 15, 2022; Accepted: Apr. 18, 2022; Published: May 12, 2022

A Dermatofibrosarcoma Case Report: Did Intravenous High Doses of Vitamin C Help in His Treatment?
José Rodríguez Gómez1, 2, Edgardo Ramirez-Cedeno3, Michael J. González4, 5, Miguel J. Berdiel6
1Universidad Carlos Albizu, Professor, PhD Clinical Psychology Program, San Juan, PR
2University of Puerto Rico, Rio Piedras Campus, San Juan, PR
3Mas Salud, Mejor Vida Clinic, CEO, San Juan, PR
4University of Puerto Rico, Professor, Medical Sciences Campus, School of Public Health, Department of Human Development, Nutrition Program, San Juan, PR
5Universidad Central del Caribe, Chiropractice School, Bayamon, PR
6Berdiel Clinic, CEO, Ponce, PR
Correspondence to: José Rodríguez Gómez, Universidad Carlos Albizu, Professor, PhD Clinical Psychology Program, San Juan, PR.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This is a case report of a young adult 25 years old diagnosed with Dermatofibrosarcoma protuberans (DFSP), a rare local malignant cutaneous soft-tissue sarcoma in his right forearm. This condition was treated with high dose intravenous Ascorbic Acid (vitamin C, 25,000 mg 2 times per week for 4 weeks) This therapeutic approach changed this tumor into a more benign form. High dose intravenous vitamin C has demonstrated anti-neoplastic activity in different tumors and stages. The Cytotoxic effect produced by vitamin C in an array of malignant cell lines has been associated with its pro-oxidant and toxic to oncogenic cells. We suggested a clinical trial with more patients to validate this therapeutic modality for this type of malignancy.
Keywords: Dermatofibrosarcoma, Intravenous High Doses Ascorbic Acid (vit. C), Cytotoxic Effect
Cite this paper: José Rodríguez Gómez, Edgardo Ramirez-Cedeno, Michael J. González, Miguel J. Berdiel, A Dermatofibrosarcoma Case Report: Did Intravenous High Doses of Vitamin C Help in His Treatment?, Research In Cancer and Tumor, Vol. 10 No. 1, 2022, pp. 1-3. doi: 10.5923/j.rct.20221001.01.
1. Introduction
- Dermatofibrosarcoma protuberans (DFSP) is a rare locally malignant cutaneous soft-tissue sarcoma. As a soft tissue sarcoma, rises from transformed cells of mesenchymal (connective tissue) origin in the middle layer of the skin (dermis) forming a lump of tissues (protuberans), that may be purplish, flesh colored or reddish. This particular skin cancer often forms on the arms, legs head and neck region, trunk and usually grows slowly and hardly produces metastasis beyond the skin. Usually, it could appear as a bruise or scar [1,2]. It grows gradually and very slow, however tends to recur after excision. Nevertheless, the tumor rarely presents metastatic disease, but has a high recurrence rate [3]. The cause of DFSP is unknown but an injury to the affected skin may be a predisposing factor Estimates of the overall occurrence of Dermo Fibro Sarcoma Protuberans in the United States are 0.8 to 4.5 cases per million persons per year. In the United States, the condition accounts between 1 and 6 percent of all soft tissue sarcomas and 18 percent of all cutaneous soft tissue sarcomas [4]. In general, Dermatofibrosarcoma protuberans is estimated to occur in 1 in 100,000 to 1 in 1 million people per year. All age groups are susceptible to suffer the condition [1,4]. Trauma at the affected site has been reported in approximately 10-20% of patients [6]. Recent advances have shown that in approximately 90% of cases, dermatofibrosarcoma protuberans is associated with a rearrangement (translocation) of genetic material between chromosomes 17 and 22 which results in the fusion of two genes [8], [9]. Skin biopsy is needed to confirm the diagnosis, within a well laboratory, and well skilled professional pathologist. It may take more than one surgical procedure to achieve complete removal of the primary tumor. Recurrence after Mohs surgery is reported rare, usually around 1%. Treatment using conventional chemotherapy is reported to be ineffective [2,7,9]. In the literature intravenous vitamin C is proposed as a possible treatment management of malignant oncogenic tumors [10,11,12]. Case Report Information:
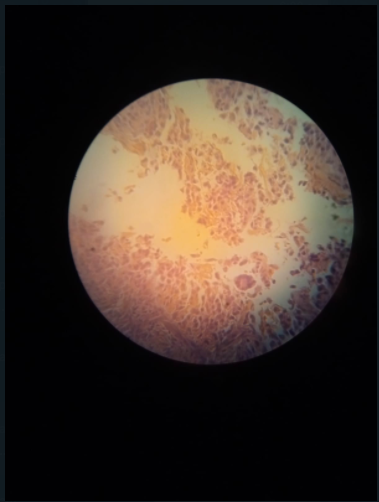 | Figure 1 |
 | Figure 2 |
2. Conclusions
- Intravenous vitamin C has demonstrated anti-neoplastic activity in different tumors and stages [10,11]. Cytotoxic effect produced by vitamin C in an array of cell lines (mostly malignant) has been associated with its pro-oxidant activity and modification or destruction of such cells [12,14]. Vitamin C and its radical may help to potentiate the activation of transcription factor NF-kappa B, which has been associated with inhibition of cell growth [1,2,4]. Evidence supports the concept of using high-dose intravenous vitamin C (HDIVC) for extended periods, in doses high enough to achieve and maintain plasma levels above those which have been found to be preferentially cytotoxic to tumor cells [11,12,13]. In this particular case, HDIVC, in a very short time, show a tumoral cytological transformation, from a dermatofibrosarcoma to a better and less aggressive cellular variant reported by pathologist as atypical fibrous histiocytoma. Usually, this kind of lesion has a better outcome with rarely metastasize [1,2,4,9]. Administration of HDIVC need to further evaluate within this kind of pathology and considered as a possible complementary treatment that may help patients to avoid malignant proliferation.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML