-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research In Cancer and Tumor
2021; 9(2): 28-32
doi:10.5923/j.rct.20210902.02
Received: Oct. 25, 2021; Accepted: Nov. 10, 2021; Published: Nov. 15, 2021

Metastatic Breast Cancer in Men
Alimkhodjaeva L. T., Norbekova M. Kh.
Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology (RSSPMCO&R), Tashkent, Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The issue of breast cancer is one of the most actual in modern oncology as this disease is the most common among the female population. But today breast cancer in men is also starting to gain momentum, especially locally advanced forms of this disease. Breast cancer metastasis is a big and difficult problem in mammalogical oncology. The tumor is characterized by significant variability in the clinical course. Therefore, the study of the prevalence and possible causes, pathogenetic factors in breast cancer is a priority in the planning and work of the mammalogical oncology service for both men and women.
Keywords: Breast cancer, Prevalence of the process, Metastases, Diagnosis, Prognosis factors
Cite this paper: Alimkhodjaeva L. T., Norbekova M. Kh., Metastatic Breast Cancer in Men, Research In Cancer and Tumor, Vol. 9 No. 2, 2021, pp. 28-32. doi: 10.5923/j.rct.20210902.02.
1. Introduction
- There is a steady increase in the incidence of malignant neoplasms in the modern world. At the same time, not only the structure, but also the dynamics of cancer incidence changes. As for breast cancer, it occupies a leading place in the structure of cancer incidence among the female and male population of developed countries [1-4]. In Uzbekistan the incidence of breast cancer continues to grow both in women and, unfortunately, in men too, despite the fact that the data are obtained only from official statistics, without in-depth epidemiological studies [5]. The pathology of the endocrine-metabolic system underlies many cancers including breast cancer in men. The hormonal effect is based on a mechanism that directly affects the processes of proliferation and differentiation in the target tissue, as well as a potentiating effect that increases the probability of genetic rearrangements [6]. Malignant neoplasms are a disease of older age groups and this is explained both by the effect of aging itself and by the accumulation of external carcinogenic influences over time [7]. Metastatic breast cancer is mostly the last stage of breast cancer, or the final stage of tumor development. According to the latest data, tumors not only with distant metastases, but also with metastases to regional lymph nodes began to be classified as metastatic breast cancer. Diagnostics of breast cancer metastases has certain difficulties. A variety of research methods have been proposed, from general clinical examination and palpation to nuclear magnetic resonance imaging and computed tomography [8]. Radiothermometry is actively used in the algorithm for a comprehensive study of the mammary glands. Russian scientists (Nechutky M.I. et al, 2003) proposed modern research methods, such as videothoracoscopic parasternal lympho- dissection in diagnosing the prevalence of breast cancer. Molecular and histochemical methods of research using tumor and tissue markers have been proposed recently and they allow to clarify the prevalence of the tumor process, conduct an adequate assessment of the treatment performed and track long-term results. Various techniques for identifying "sentinel" lymph nodes which are the first on the pathway of lymph drainage from the primary tumor in the mammary gland have been developed over the past 5 years. Speaking about the role of the sentinel node, it was noted that some tumors have sentinel nodes both in the axillary zone and in the retrosternal zone. Thus, a review of the literature data showed that there was a fairly high incidence of breast cancer metastatic forms. According to most authors data, especially in developing countries, from 50 to 70% of patients have advanced forms of the disease upon admission. This is especially true for men (locally advanced forms, in the form of lesions of regional lymph nodes and distant metastases to various organs). The nature and frequency of distant metastases of breast cancer are very diverse. In 40-80% of cases breast cancer has metastases to the bone. However, it can metastasize to other organs and systems, for example, to the liver, lungs, brain and others. Diagnosis and treatment of distant metastases of breast cancer are an urgent problem in oncomammology, since mortality at these forms remains very high. The long-term and immediate results of treatment are still very unsatisfactory.Aim of the study was an optimization of diagnostic and therapeutic measures with evaluation of prognostic factors in metastatic breast cancer in men.
2. Material and Methods
- The study on the results of metastatic breast cancer treatment in the Republic of Uzbekistan covers the period from 2010 to 2020. The material of the study was data on all cases of morbidity and mortality from malignant neoplasms of the breast in men at the Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology (RSSPMCO&R). During the study period according to the cancer registry RSSPMCO & R 103 patients with newly diagnosed metastatic breast cancer were registered and treated in Uzbekistan. The most numerous group consisted of breast cancer patients with metastases in the age group of 41-50 years (31%) and 51-60 years (27.3%). There were slightly fewer breast cancer patients aged 61-70 years (19.6%) and even fewer in old age - 79 patients (7.6%). The most frequent histological forms of the primary tumor were lobular (41%) and ductal (30%) types of cancer. In 13.5% of cases, the histological structure of the tumor was represented by an undifferentiated form in stipulated in some cases by therapeutic pathomorphosis. Less commonly, other histological variants of the tumor were presented, such as glandular solid, scirrhoid, mucous and medullary types. Statistical and clinical research methods were used in our study. Determination of standard errors was performed using a 95% confidence interval (CI). Sure, the use of a 99% confidence interval more truthfully reflects the statistical parameters of the studied phenomenon, but in most cases, the use of a 95% confidence interval is sufficient. Survival (overall, cumulative) was estimated using the Kaplan-Meier survival table, and the reliability between the compared survival curves was performed using the Mantel-Haenzel test. The methods of univariate analysis based on computer programs were used for determining the prognostic factors. All studies were conducted in accordance with the strict unified criteria of WHO and IARC (International Agency for Research on Cancer). The survival frequency and survival rates reflect the state of diagnosis, registration of cancer, the state and efficiency of the special therapy performed. The data do not fully reflect the results of the disease outcome or treatment, since some patients, and sometimes this part, reaches up to 40-50% and, according to various sources, are excluded from the review. The survival table provides complete information accumulated over a certain period until the full end of the period or date of the survey. This method of calculating survival is very convenient for studying small series of observations. However, later it was shown that it could be used for large series, with a large number of observations, even with the use of a computer. The survival table shows the survival rate calculated by the direct method. A widespread scoring technique that is often used in computer programs is the Kaplan-Meier (1958) estimator. This is a similar method, similar to the actuarial one, but instead of calculating the cumulative survival rate at the end of each year of follow-up, the proportion of patients who are alive in a short time interval is calculated. Diagnostics of metastatic breast cancer consists of 2 sequential stages: primary and clarifying diagnostics. The primary diagnostics includes an individual examination, anamnesis, the use of clinical methods, and it is aimed at determining the clinical and anatomical form of relapse. Clarifying diagnostics is carried out using instrumental and laboratory research methods and is aimed at determining the prevalence of both primary or recurrent and secondary tumors, its morphological structure and evaluation of the patient general condition. When studying the anamnesis, the timing of the appearance of the first signs of a tumor and the rate of their development were determined. The stage of the primary tumor, its clinical form, localization in the mammary gland, histological structure, the nature of the treatment of the primary neoplasm and the presence of hormonal diseases play an important role: these objective data largely determine the localization and frequency of subsequent metastasis. Clinical manifestations of metastases in breast cancer depend on the clinical and anatomical form of the secondary tumor (localization, number of metastatic nodes, their size, volume of bone-destructive lesions, growth of the chest wall, pressure on the abdominal and retroperitoneal organs), as well as the general condition of patients. Instrumental examination methods were as follows: ultrasound of the soft tissues of the chest wall, regional lymph nodes and abdominal organs, computed tomography.Surgical methods: lymph node biopsy; excisional biopsy; pleural puncture in the presence of fluid in the pleural cavity; chest x-ray; scintigraphic examination of skeletal bones. Histological examination: examination of calcium; tumor markers. A large number of markers are currently available for the breast cancer diagnostics. These include estrogen and progesterone receptors, DNA ploidy and S-phase profile, epidermal growth factor receptors, HER-2 / neu oncogene, p53 tumor suppression gene, cathepsin D, proliferation markers, СА-15-3, СЕА, МСА, СА-549. The most widely used of them are receptors for estrogen and progesterone, the oncogene HER-2 / neu. Currently, the possibilities of CA-15-3 and CEA as a monitoring test for breast cancer are being studied. Other markers such as MCA, CA-549 have specificity and sensitivity similar to those of CA-15-3. Usually one of the mucins (eg CA-15-3 or MCA) and CEA are used. Serum levels of CA-15-3 and CEA depend on the stage of the disease - they are significantly higher in patients with lymph node involvement and in large tumors in compare with small tumors. Low levels of markers in patients with suspected breast cancer do not exclude the presence of a tumor, either primary or metastatic. But on the other hand, high levels of the marker in patients with breast cancer almost always reflect the presence of a metastatic disease, the presence of distant metastases. CEA and CA 15-3 are also useful for monitoring metastases, but are not used in the early diagnosis of loco-regional recurrence, where clinical examination is the preferred method. Unfortunately, the study for tumor markers was carried out only in a relatively small proportion of patients. And the study of calcium in the blood was not carried out in any patient.
3. Results
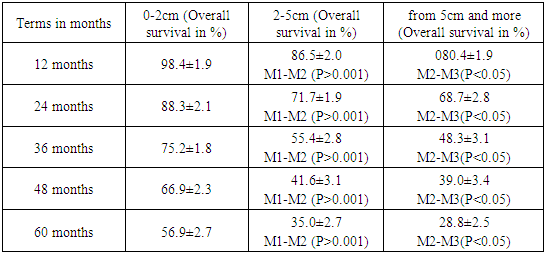
- At the first stage we studied such factors as the stage of the primary tumor or the size of the neoplasm in the mammary gland. The sizes of neoplasms ranged from 0 to 5 cm and more (Table 1).
|
|
|
4. Discussion
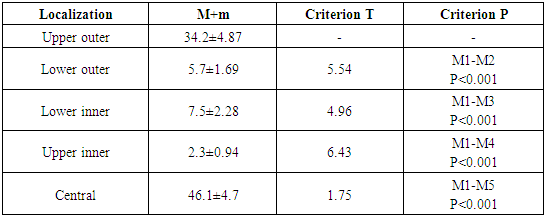
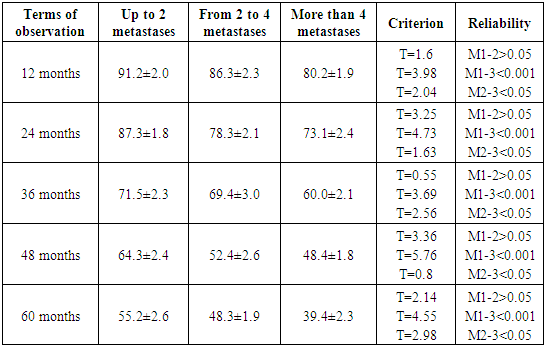
- Analysis of five-year survival data showed that the lowest rates were obtained with the lesion of the parasternal lymph nodes (47.5%) and this difference was statistically significant in comparison with all other groups of patients. A rather low survival rate was also noted among the group of patients with lesions of the cervical and supraclavicular lymph nodes (50-51%) compared with axillary and subclavian lesions (57% and 65%).We have studied the overall survival rate of patients with metastatic breast cancer depending on the age of the patients at the time of diagnosis. The survival rate of patients in the first year of life was statistically significantly higher in the group of men relative to the older age (51 years and above) compared with the age group of 31-40 years. It should also be noted that when comparing the age groups 61-70 years and 41-50 years, the survival rate was statistically significantly higher in the first one. There were no significant differences in survival between the age groups of 61-70 years and 51-60 years. Approximately the same trend persists when studying three-year survival rates. However, there was a statistically significant difference when comparing the indicators in the group of patients under 50 years old: the survival rate was higher in the group of patients aged 41-50 years, compared with the group under 40 years old. The highest five-year survival rates were observed in the group of patients aged 51-60 in compare with other age groups. It was statistically significantly higher in relation to only one group (31-40 years old). There was no reliability of the compared values in relation to other groups. According to our study, bones were affected in 24.0% of cases at the initial admission in men. In 8 cases it was the spine, in 7 - the ribs and 4 - the ilium. Osteolytic lesion was observed in 5 patients. Such a lesion is characterized by the washing out of the mineral part of the bone, its thinning and fractures. There were no fractures in our cases. Osteoblastic metastases, on the other hand, are characterized by compaction of the mineral part. Compaction of bone tissue is caused by the fact that tumor cells can both directly destroy bone tissue and stimulate cells that renew this tissue. So, when osteoclasts (resorbing bone) are stimulated, osteolytic metastases occur, when osteoblasts (cells that deposit hydroxyapatite) are stimulated, osteoblastic lesions occur. It was difficult to determine the type of lesion radiographically in two cases. The main clinical manifestation of tumor metastases in the bone was pain syndrome which occurred in 65% of cases. The pain arose as a result of tumor infiltration of nerve endings, an increase in intraosseous pressure, as well as stimulation of nerve endings with substances secreted by the tumor. Pain syndrome is explained by chemical and mechanical effects on nanoreceptors. At the complex treatment to which (15.1%)) of men were subjected, all patients underwent surgery, radiation therapy and chemo-hormonal treatment. Postoperative complications were noted in 4 (13%) patients after radical mastectomy: in 3 patients - lymphorrhea, in 1 - marginal necrosis of skin flaps. During histological examination of the postoperative material, the diagnosis of metastasis was morphologically confirmed. This was the reason for further special treatment. At the second stage the patients underwent radiation therapy on the affected areas. The interval between surgical treatment of the primary tumor and radiation therapy, as well as the sequence of these procedures varied depending on the extent of the tumor process. Moreover, in the first case, the irradiation techniques were significantly more varied: from wide-field to local with equivalent total focal doses in the range of 24 - 36 Gy and irradiation modes of fraction of 4 Gy. After the operation, the method of radical radiation therapy was used with a single dose of 2 - 2.5 Gy and a total focal dose of 44 - 50 Gy. A complication in the form of post-radiation epidermis was developed in some patients at a single dose of more than 3 Gy. In parallel with radiation therapy, less often after it, patients were performed chemotherapy. Metastatic breast cancer tumors, like the primary breast tumor itself, are sensitive to many antitumor drugs. The most popular for both monochemotherapy and combination chemotherapy are cyclophosphamide, 5-fluorouracil, methotrexate and doxorubicin. These drugs are included in the schemes of the most popular combinations, such as CMF (cyclophosphamide, methotrexate, 5-fluorouracil), CAF (cyclophosphamide, doxorubicin, 5-fluorouracil) and AC (doxorubicin, cyclophosphamide). Most often, patients were prescribed the CMF regimen (in 50% of cases), less often AC - 27%, CAP was prescribed to 23% of patients. Most often, 4 courses were carried out - in 37% of cases, less often 3 courses were prescribed - 24%. One and two courses were prescribed in 3% and 10%, respectively, which was caused by the presence of concomitant diseases in patients and their exacerbation during chemotherapy. 13% of patients received 5 and 6 courses of chemotherapy. Side effects during chemotherapy were observed in 93% of patients. The main side effects of chemotherapy were nausea, vomiting, neutropenia, leukopenia, diarrhea, stomatitis and alopecia. At complex treatment a relatively complete control of the metastatic disease was ensured which prevented further local and secondary spread of the tumor and also complete local cure was achieved. At the combined treatment which was carried out in 67 (36%) patients, a local effect was used in the form of surgical or radiation treatment. Chemotherapy was performed after surgery or in parallel with radiation therapy. Compared to complex treatment, the combined treatment used more options for chemotherapy, in particular, monotherapy (with doxorubicin or taxoter) was also used. Local treatment in the form of radiation therapy was performed in patients with localized metastases: in the spine - 8, the ilium - 4, ribs - 7, bones of the lower limbs - 1. Surgical treatment was further supplemented by radiation and chemotherapy. Thus, a comparative analysis of the complex, combined, local and systemic approaches to the treatment of patients with breast cancer metastases shows that their use is sometimes determined by the localization, the prevalence of metastases, as well as the general condition of patients, their age, the presence of concomitant diseases. At the same time, complex, combined and local approaches to the treatment of breast cancer metastases provide a higher frequency of local cure which prevents further spread of the tumor process.
5. Conclusions
- To summarize all of the above, the best option for the treatment of MBC in men is an integrated approach. The lowest survival results with the combined treatment approach are determined by the fact that appropriate local treatment of the metastatic focus is not provided. At the same time, at a complex approach, intense local effect, the further spread of the tumor is prevented, which ensures high local control. When assessing the overall survival of patients with various treatment approaches, the best results were also achieved with the complex treatment of metastatic breast cancer. So, 64.2% of patients survived 5 years or more, which was statistically significantly higher than with the combined and combined methods (P <0.05, t = 2.l). There is no doubt that the histological structure of the primary tumor plays an important role in the clinical features of the disease and the choice of treatment tactics. One of the objectives of our research was to study the effect of histological structure on treatment results and overall survival of patients with metastatic BC. When choosing a method for the treatment of metastatic BC in men, it is necessary to take into account the localization of metastasis, the age and general condition of the patient, the presence of concomitant diseases and previous treatment for primary breast cancer. The number of metastatic regional lymph nodes, the histological structure of the tumor, as well as the methods of treatment used are also important prognosis factors.Thus, in the treatment of metastatic breast cancer in men, it is necessary to provide adequate local treatment of the primary focus, control of regional and distant metastases which prevents further spread of the tumor process.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML