-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research In Cancer and Tumor
2021; 9(1): 1-7
doi:10.5923/j.rct.20210901.01
Received: Dec. 31, 2020; Accepted: Jan. 16, 2021; Published: Jun. 30, 2021

Histopathological Study of Oral and Oropharyngeal Lesions in a Tertiary Care Hospital
Md. Sabbir Hossain 1, Md. Rahimullah Miah 2, Mahfuja Fardous 3, Nur-E-Jannatul Ferdous 4, Md. Golam Mostofa 5, S. A. M. Imran Hossain 6, Chowdhury Shadman Shahriar 7, Mohammad Taimur Hossain Talukdar 8, M. A. S. Ansari 9
1Associate Professor, Department of Pathology, North East Medical College and Hospital, Sylhet, Bangladesh
2Head, Department of Information Technology in Health, North East Medical College and Hospital, Sylhet, Bangladesh
3Ex-Student of Master of Public Health, National Institute of Preventive and Social Medicine (NIPSOM), Dhaka, Bangladesh
4Assistant Professor, Department of Pathology, North East Medical College and Hospital, Sylhet, Bangladesh
5Department of Medicine, Combined Military Hospital (CMH), Jalalabad Cantonment, Sylhet, Bangladesh
6Associate Professor and Head, Department of Oral and Maxillofacial Surgery, North East Medical College and Hospital, Sylhet, Bangladesh
7USMLE Student, USA and Ex-student of North East Medical College, Sylhet, Bangladesh
8Associate Professor, Department of Clinical Oncology, North East Medical College and Hospital, Sylhet, Bangladesh
9Associate Professor, Department of Pathology, Sylhet Women’s Medical College, Sylhet, Bangladesh
Correspondence to: Md. Sabbir Hossain , Associate Professor, Department of Pathology, North East Medical College and Hospital, Sylhet, Bangladesh.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Oral diseases are major public health problems owing to their high prevalence and incidence in all regions of the world. Bangladesh is particularly under privileged area in south east Asia with densely populated country. Current report says that 11.9 percent people are affected by oral cancer. Therefore, this study has been undertaken to evaluate the histopathological spectrum of oropharyngeal lesions. A prospective, descriptive cross-sectional study was from January 2017 to December 2018. Patients of different age group and both sexes were selected for this study according to inclusion and exclusion criteria. Present study comprised of 69 cases oral and oropharyngeal lesions of which were 58% of male, and female 42%. The age range was from 35 to 90 years with an average of 58.21 years, the highest number of patients to be in 5th decade. According to site of involvement, tongue is the commonest site. Among 69 cases, 5 cases (7%) were non-neoplastic, 2 cases (3%) were benign tumour and 62 cases (90%) were malignant tumour. However, this small study gives an understanding of the national scenario.
Keywords: Non-neoplastic lesions, Benign tumours, Malignant tumours, Squamous cell carcinoma, Verrucous carcinoma
Cite this paper: Md. Sabbir Hossain , Md. Rahimullah Miah , Mahfuja Fardous , Nur-E-Jannatul Ferdous , Md. Golam Mostofa , S. A. M. Imran Hossain , Chowdhury Shadman Shahriar , Mohammad Taimur Hossain Talukdar , M. A. S. Ansari , Histopathological Study of Oral and Oropharyngeal Lesions in a Tertiary Care Hospital, Research In Cancer and Tumor, Vol. 9 No. 1, 2021, pp. 1-7. doi: 10.5923/j.rct.20210901.01.
Article Outline
1. Introduction
- Oral and oropharyngeal cancers are the biggest magnitudes of all cancers in the present world. A wide range of group people fall into oral and oropharyngeal cancers, which occurs in the mouth itself [28]. Oral and oropharyngeal cancer is the main global public health problem, which is congregated together as the sixth most common cancers in different countries of the world [35,36]. These cancers upsurge in the rate of commonness within two eras. Still there is no national dynamic screening policy or else protocol, and the risk factors for these diseases remain to be reasonably unchanged. Oral cancer is a critical health problem, which is the key reasons of death from oral diseases in different countries [29]. The oral cavity and oropharynx are the peak portions of the digestive tract and unique in the variety of tissues enclosed within a minor zone [1]. The prevalence of cancer of the oral cavity was testified as 2.6% of all cancers tailed by 1.2% of pharyngeal cancers [2]. Two thirds of oral cancer are the most common cancer in men worldwide, which is borne by developing countries [3]; [4]. Oral cancer is the conjoint type of cancer in Bangladesh among people of all cancers, which are of oral cavity [5]. The oral cavity is the first part of digestive system and there are many types of tissues like bone of mandible and maxilla, epithelial tissue of oral mucosa, minor salivary glands, and odontogenic tissue; it liable for different types of epithelial, mesenchymal and lymphoid tumours [6]. Oral cavity is prone for a myriad of changes [7]. Approximately one person every hour of everyday will die from oral cancer in the United States of America alone [28]. Human papilloma virus (HPV) DNA may be associated with recurrence of HPV-positive head and neck squamous cell carcinoma, which is estimated to cause almost 22% of oropharyngeal and 5% of oral cavity squamous cell carcinomas (SCCs) worldwide [39]. This recurrence was also detected in the absence of demonstrable HPV DNA to suggest that the presence of HPV DNA may be associated with detection of sub-clinical cancer [38]. Oral squamous cell carcinoma (OSCC) is a common malignancy of the head and neck areas of human beings [29]. Histopathological grading was introduced by Broders for squamous cell carcinoma of the lip and was based on the differences in differentiation between tumours [30]. Later more complex grading systems were suggested by Jakobsson et al. [31], Anneroth et al., [32] and Bryne et al. [33]. Inquisitively on the oral cancer situation, the World Health Organization (WHO) did not ratify effective multifactorial provisions and paid little consideration to minimum data sets or uniform histopathological reporting [29]. Early detection may provide patients the opportunity for long-term disease control through surgical salvage of locoregional recurrence or oligometastatic disease [42,45].With advancing age as well as a result of the environmental and life style related factors, oral lesions can occur as a result of infections, local trauma or irritation, systemic diseases and excessive consumption of tobacco, betel quid and alcohol [8]. Benign tumours and tumour like conditions of oral cavity include eosinophilic granuloma, fibroma, granular cell tumour, lipoma, keratoacanthoma, schwannoma, papilloma, neurofibroma, pyogenic granuloma etc, as well as odontogenic tumours [9]. The usual treatment for these conditions is to surgical excision since they are unlikely to recur [10]. There is a wide variation in the incidence and mortality rates of oral cancer [11] in different regions around the world. In the developing world oral cancer is the third most common cancer after stomach and cervical cancer [12]. In Bangladesh [13] particularly under privileged area, current report says that 11.9 percent people are affected by oral cancer [14]. Therefore, this study has been undertaken to evaluate the histopathological spectrum of oropharyngeal lesions.
2. Material and Methods
- A prospective, descriptive cross-sectional study was conducted in the Department of Pathology, Northeast Medical College & Hospital, Sylhet in Bangladesh during a 24 months period from January 2017 to December 2018. Patients of different age group and both sexes were selected for this study according to inclusion and exclusion criteria. Inclusion criteria were all Oral and oropharyngeal lesions for which biopsy is advised for histopathological examination. The exclusion criteria were major salivary gland lesions, Patients receiving chemotherapy and radiotherapy. A total of 69 cases who met the enrolment criteria were included in this study. Oral and oropharyngeal tissues collected from lesion by biopsy. All obtained specimens were immersed in 10% buffer formalin. These samples were fixed for 6 hours to 24 hours which were required for proper H&E. Routine tissue processing and routine H&E staining were done on all 69 cases at the department of Pathology, North East Medical College & Hospital, Sylhet. Statistical analysis of the results was obtained by the statistical software of SPSS, version 26. The results were presented in tables, figures, charts and diagrams. Every ethical issue was discussed with the patients; regarding the study and informed written consent were obtained.
3. Results
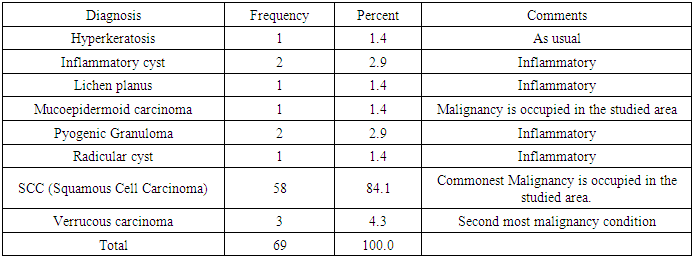
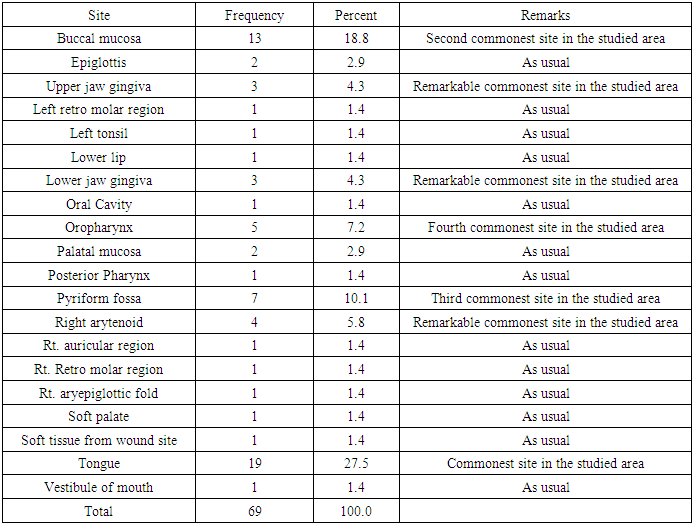
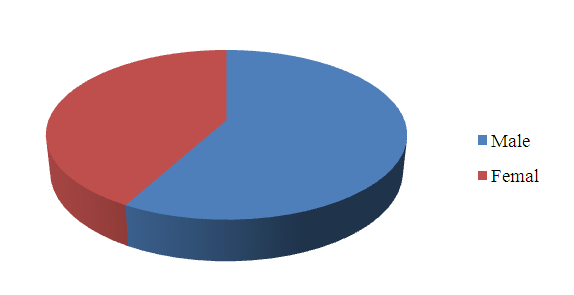
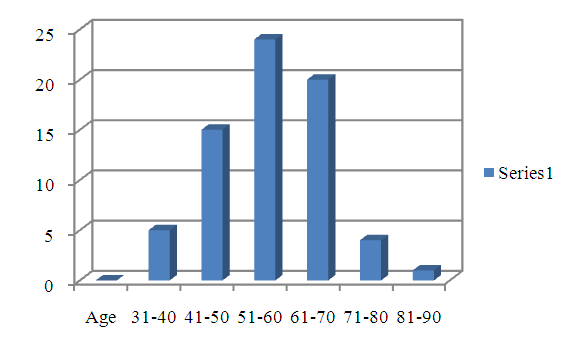
- Present study comprised of 69 cases oral and oropharyngeal lesions of which were 58% of male and (42%) of female (Fig. 1). The male and female ratio was 1:1.38. The age range was from 35 to 90 years with an average of 58.21 years (Fig. 2). The cases were divided into six age-groups according to decades, the highest number of patients to be in 5th decade (51-60 years old). According to site of involvement, tongue is the commonest site (19 cases, 27.5%) followed by buccal mucosa (13 cases, 18.8%), which as shown in Table 2. Among 69 cases, 5 cases (7%) were non-neoplastic, 2 cases (3%) were benign tumour and 62 cases (90%) were malignant tumour (Fig. 3). Among 69 cases, 5 cases were different histopathological types of non-neoplastic lesions. Of these, vast majority 2 cases were inflammatory cyst. Among 2 cases of benign tumour all were pyogenic granulomas. Out of a total of 62 malignant tumours, vast majority 58 (94%) were invasive squamous cell carcinoma (Table 1).
|
|
 | Figure 1. Distribution of patients by sex |
 | Figure 2. Distribution of patients by age gradation |
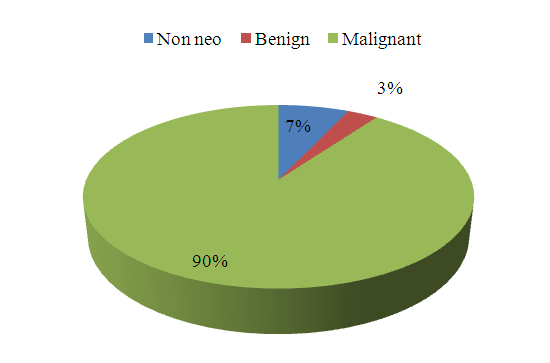 | Figure 3. Distribution of patients by histological pattern (n =69) |
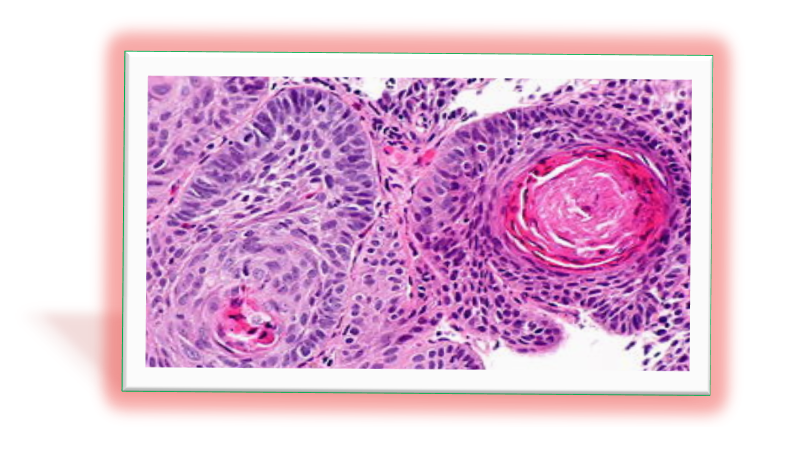 | Figure 4. Photomicrograph showing squamous cell carcinoma of Buccal Mucosa (case no. 29 H&E x 400) |
4. Discussion
- The diagnosis of a variety of lesions that occurring in the oral cavity and oropharyngeal region are essential part for the evaluation of the oral health of any population. Several studies on oral and oropharyngeal lesions have been done in India, Pakistan and many other regions of UK and USA, but not much yet have been done in our country [15]. The purpose of the present study was to record and analyse histological types, demographic profile, epidemiological factors, sites of tumour origin and to find out the possible etiological factors associated with oral and oropharyngeal lesions. A variety of non-neoplastic and neoplastic lesions can involve the oral cavity and oropharyngeal region. In present study, the affected age ranges from 35 to 90 years with mean age of 58.21 years. Two different studies done by Modi et al. and Kosam et al. reported the age group as 3-90 and 8-85 years respectively [16]; [17]. The gender distribution shows higher number of males (58%) cases, though the difference with female was not significant. The finding was similar to Gupta et al. [3]. The contributing factor for male predominance in our study may be due to smoking.Out of total 69 patients, malignant neoplastic lesions 62(90%) occurring in maximum number of cases. Similar observations were also reported by Modi et al., [16] (53.4%), (82.5%) [3]; (74%) [17], (85%) [18], (72%) [19], (93%) [20] and (98%) [21]. Remaining 5(7%) cases were diagnosed as nonneoplastic lesions, 2 (3%) as benign tumours [21]. The predominance of malignant tumours may be due to the fact that many clinically benign tumours, tumour like conditions and non-neoplastic lesions were not sent for histological examination. The study place North East Medical College is a tertiary care hospital, which receives mostly referred suspected cases of malignant lesions. Other than these, in Bangladesh the most common habit of non-smoking and smoking tobacco and betel nut with jorda or shada pata (tobacco leaf) may be the predisposing cause of predominance of malignant tumours in the study. Among the oral and oropharyngeal lesions 19(27%) cases were originated from tongue followed by 13 (18.8%) from buccal mucosa and 7(10.1%) from pyriformis fossa. In our study tongue was most common site (42%) of lesions which was concordance with the studies of Ahluwalia et al. and Sankara Narayanan et al. [22]; [23]. The buccal mucosa, retromolar trigon, tongue and floor of the mouth were also found the most frequent sites by Rahman in Bangladesh [24]. It was observed in various published literature that oral malignancies were anatomical more frequent in the anterior parts (buccal mucosa, anterior 2/3 of the tongue, alveolus, lips and base of tongue).Squamous cell carcinoma with varying differentiation ranked first in this study among the histopathological types of malignant tumours. In present study well differentiated squamous cell carcinoma was most common histologic variety (94%). It was in concordance with the studies done by Patel and Pandya, and Ahluwalia et al. [8]; [22]. Pyogenic granuloma ranked first in the present study among the histopathological type of benign tumour. This was accordance with finding observed by Gupta et al. [3]. Oral medicine specialists and pathologists play primal roles in the early diagnosis, prevention and follow-up systems of oral cancer [25]. They act the biopsy systems in oral pathological activities that determine lesions; therefore, strategies are malleable for the disease management process of the sensed lesion [26]. Maxillo-facial surgeons take part in cardinal point in management generally to regenerate the function of jaws and maxillo-facial tissue after tumor obliteration. For transmutation of the patients’ psychological precondition, they regenerate the serviceable and decorative imperfection with prosthetic construction carried out by prosthodontist in the maxillo-facial region [26]. With an oral and maxillo-facial surgeon’s counseling, to improve the life quality of the patient, the maxillo-mandibular dentures were constructed by an experienced prosthodontist. The patient of oral cancer is chewing and he/she is silent under the control period of time in uneventful status. The controlling system is a multifactorial method including diverse factors and limitations with a capricious impact should be measured in the decision-making procedure for management of oral and oropharyngeal cancer. On the other hand, ssurvival rates are significantly higher among patients diagnosed with HPV-positive than HPV-negative oropharyngeal cancer [40,41]. However, approximately 20% of patients diagnosed with HPV-positive oropharyngeal cancer experience cancer progression or die within 5 years [42]. Retrospective studies suggest that detection of oral HPV-16 DNA after completion of curative treatment may help to identify patients at increased risk for recurrence of HPV-positive oropharyngeal cancer [46,47,48]. This study is leading to detection of subclinical disease at stages amenable to therapy associated with low morbidity and high survival rates [50,51,52]. But, another study stated the higher prevalence of infection among smokers, which are consistent with smoking-induced oral mucosal immunosuppression [49]. Recently, sensor technology including artificial intelligence, internet of everything, machine-learning tools have been used to analyze factors that could influence the probability of survival, including TNM stage and WHO grade [34]. The ISNAH system is essential of sensor technique for the treatment of oral and oropharyngeal cancer, which implies positively Impact of Sensor Networks towards Animals and Human beings [37]. Moreover, the TNM cataloguing of cancer staging is included on assessment of the magnitude of the crucial tumor (T), entanglement of locoregional lymph nodes (N) and distant metastases (M). This cataloguing is vital for treatment planning, assessing risk of recurrence, and estimate of inclusive survival.
5. Challenges
- Treatment of patients with cancer of the oral cavity and oral-pharynx is a challenge for the surgeon and oncologist [1] due to unwanted augmentation of oral cancer. Blood flow and blood volume within maxilla-facial tissue are also reported to be elevated in comparison with therapy-altered tissue with corresponding flexible in installation time [27]. Cutting-edge sensor technology is misused for histopathological data bouncing and displaying false interface at science laboratory and sharing report with patients and doctors [37,53].
6. Conclusions
- This study concludes an idea of the national scenario about histomorphological pattern of oral and oropharyngeal lesions. The findings are malignant in majority of oral cavity and oropharyngeal lesions. Tongue was the most common site for neoplastic lesion of oral cavity and oropharynx. Carcinoma was most common, with squamous cell carcinoma as the commonest histological variety. Therefore, accurate diagnosis and staging of these oral cancers are prerequisites for choice of optimal treatment. National Comprehensive Cancer Network guidelines recommend that patients with head and neck SCC (HNSCC) undergo routine clinical surveillance for cancer recurrence [43]. The study recommends future research trajectories of a new dynamic system to drive methodological agenda to make better health management in connection with National Health Policy and Sustainable Development Goals 2030.
7. Disclosure
- Data AvailabilityThe data are being used to support the findings of this research work are available from the corresponding author upon request. Competing InterestsThe authors declare no potential conflict of interests in this research work.
ACKNOWLEDGEMENTS
- The authors acknowledged the authority of Northeast Medical College & Hospital (NEMCH), Sylhet, Bangladesh for kind support.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML