-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research In Cancer and Tumor
2013; 2(2): 31-34
doi:10.5923/j.rct.20130202.02
Prostate Sarcoma: Rarity of the Disease and Its Survival Aspect
Azhar Amir Hamzah1, Hasmah H1, Mohammad Nor Gohar Rahman1, Azreen Syazril Adnan2, Amer Hayat Khan3
1Urology Unit, Department of Surgery, Hospital University of Malaysia, Kubang Kerian, Kelantan, Malaysia
2CKD Resource Centre, Hospital Universiti Sains Malaysia, Kubang Kerian, Kelantan, 16150, Malaysia
3Department of Clinical Pharmacy, School of Pharmaceutical Sciences, Universiti Sains Malaysia, 11800 Penang, Malaysia
Correspondence to: Azhar Amir Hamzah, Urology Unit, Department of Surgery, Hospital University of Malaysia, Kubang Kerian, Kelantan, Malaysia.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Prostatic sarcoma is an extremely rare type of adult non-epithelial malignant tumour of prostate. We report a case of 51 years old man with the urinary outflow obstruction which complicated to external compression to the rectum causing intestinal obstruction. Patient had histologically proven from prostate biopsy which showed pleomorphic prostate sarcoma. He had a complete staging assessment and it was advanced disease; prostate sarcoma with local infiltration and distant metastasis to the lung. Pelvic ultrasound was arranged for evaluation of prostate, to look for evidence of prostate abscess or prostatitis. However the result didn’t show any evidence of that. It revealed prostatomegaly with volume of 230 cm3. The diagnosis was further in dilemma. Transrectal Ultrasonography (TRUS) with prostate biopsy was planned but failed because of unbearable pain. CT-Scan Thorax and Abdomen performed to complete the cancer staging and it showed there’s evidence of lung metastasis. Patient current staging did not suitable for any surgical intervention and underwent a course of radiotherapy. Radiotherapy is a better option for patient survival.
Keywords: Prostate Sarcoma, MRI, Radiotherapy
Cite this paper: Azhar Amir Hamzah, Hasmah H, Mohammad Nor Gohar Rahman, Azreen Syazril Adnan, Amer Hayat Khan, Prostate Sarcoma: Rarity of the Disease and Its Survival Aspect, Research In Cancer and Tumor, Vol. 2 No. 2, 2013, pp. 31-34. doi: 10.5923/j.rct.20130202.02.
1. Introduction
- Non-epithelial prostatic neoplasms are very rare and it has both benign and malignant which is a highly aggressive tumour.[1] Because of the rarity of disease, it is often limited in understanding and recognition of the disease, and may pose a diagnostic challenge which requires appropriate immunohistochemistry studies, challenge in therapy and its prognosis as well.[1,2]Most lesions in this category are mesenchymal in origin, such as prostatic stromal tumours arising from specialized prostatic stroma, smooth muscle tumours, both benign and malignant, and solitary fibrous tumours. Less commonly occurring tumours include neural, germ cell and melanocytic tumours that may be derived from cells not normally present in the prostate. Some tumours have well-established extraprostatic counterparts and, when encountered, are more commonly extraprostatic/secondary in origin; these include gastrointestinal stromal tumours and most haematopoietic tumours. The majority of tumours are characterized by a spindle cell pattern with significant overlap in morphological features. They need specific immunohistochemistry staining to differentiate the type of sarcoma itself.[1] The aim writing this case is looking at other centre’s experience in managing such this rare case with their survival rate.
2. Case Presentation
- A 51 years old gentleman, who presented with history of worsening lower urinary tract symptoms for 3 months with initially treated as Benign Prostatic Hyperplasia (BPH) and started him on Alfuzocin and Finasteride. Clinical symptoms were not improving moreover he had few episodes of acute urinary retention which requiring continuous bladder drainage (CBD). The diagnosis of BPH was in doubt, as patient complains of suprapubic pain, urethral discharge, perineal pain and pain during defecation. Furthermore, he had no fever. On Digital Rectal Examination (DRE), it showed the prostate was really huge about 100 gm estimated volume, soft in consistency and very tender. He was admitted for antibiotics empirically treated for prostatitis with differential diagnosis of prostate abscess and also for further evaluation of the problems. In ward we did trial without CBD but it was failed and failed to reinsert CBD because of multiple false tract. So, suprapubic catheterization was performed.Pelvic ultrasound was arranged for evaluation of prostate, to look for evidence of prostate abscess or prostatitis. However the result didn’t show any evidence of that. It revealed prostatomegaly with volume of 230 cm3. The diagnosis was further in dilemma. Transrectal Ultrasonography (TRUS) with prostate biopsy was planned but failed because of unbearable pain. As the Prostate Specific Antigen (PSA) come back as low level; 1.9 ng/mL, assumed prostatic tumour. Magnetic Resonance Imaging (MRI) of pelvis for detail assessment of tumour was considered, unfortunately he developed intestinal obstruction which most possible the cause was external compression to the rectum secondary to huge prostate tumour. So, patient underwent surgery for trephine colostomy and at the same time examination under anaesthesia (EUA) with prostate biopsy. Inter-operative findings of EUA showed that a part of tumour had ruptured into the rectum leaving some fleshy tissue and slough. Biopsy was taken from the residual prostate and patient recovered postoperatively.MRI features represent of prostate malignancy with local involvement of urethra, rectal wall, right ischiorectal fossa and lymph nodes metastasis (Fig 1 & 2). It is likely prostatic leiomyosarcoma. Prostate tissue biopsy showed some infiltrating between normal skeletal muscle and smooth muscle. No glandular epithelium identified. It is highly cellular, composed of interlacing short fascicles and in areas forming storiform pattern of spindle shaped cells with moderately pleomorphic elongated nuclei, some with conspicuous nucleoli and eosinophilic cytoplasm. There are 19 mitotic figures within 10 HPF but no atypical forms seen. The tumour cells show strong positivity for Vemintin, focal positivity for SMA. The tumour cells are negative for Desmin, EMA, CD 117, S100 progesterone and estrogen. It is concluded as pleomorphic sarcoma differential diagnosis includes leiomyosarcoma, synovial sarcoma, stromal sarcoma.CT-Scan Thorax and Abdomen performed to complete the cancer staging and it showed there’s evidence of lung metastasis. Patient current staging did not suitable for any surgical intervention and underwent a course of radiotherapy.
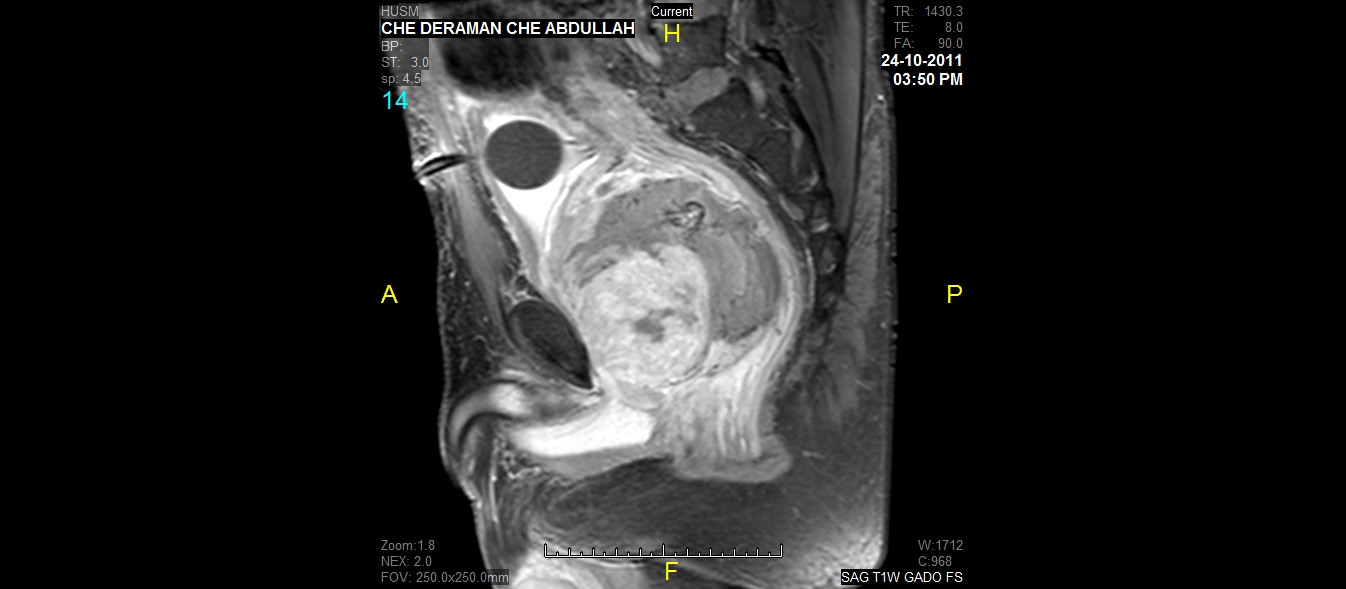 | Figure 1. This Figure Show Large Well Defined Lobulated Hetegenous Intensity Mass Occupying The Pelvic Cavity Measuring 7.4cm(ap) X 9.1cm(w) X 8.9cm(cc) Likely From Prostate Gland |
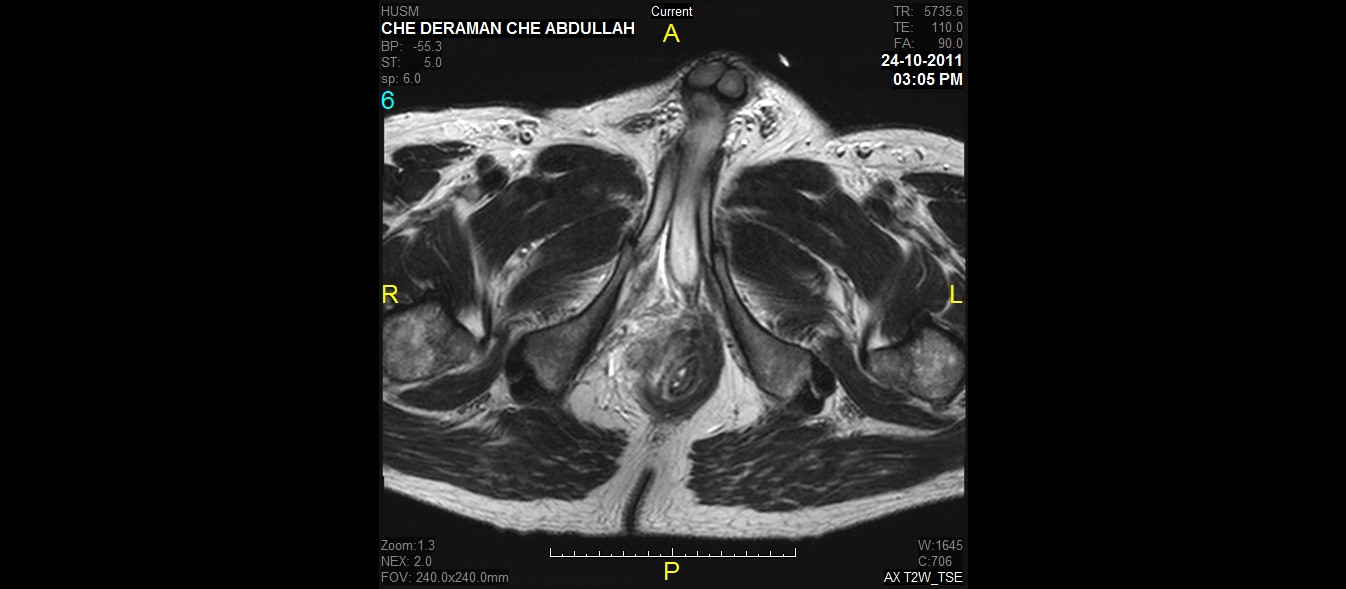 | Figure 2. The mass compresses the rectum to the left and with poor plane of demarcation with the rectal wall |
3. Discussion
- Prostatic sarcoma is an extremely rare prostate cancer type. It accounts for less than 0.1 percent of primary prostate cancer types in adults. The most common subtype of prostatic sarcoma is leiomyosarcoma and fibrosarcoma whereas rhabdomyosarcomas are the commonest histological type in children.[2] A prostatic sarcoma may occur at any age, in relatively younger men between the ages of 35 and 60, and only 25% of patients are over 40 years old. Twenty-five percent of cases are presented with metastatic diseases at the time of diagnosis. Prostatic sarcoma remains localized for a viable period of time before it spreads locally to the bladder, rectum or perineum. Over more time the tumor will spread to distant locations like the lungs, brain, bone or liver. Metastatic spreading via the lymphatics to the nodes, and haematogenously to the liver, lungs, and bone. The most common sites of distant metastasis are the lungs.[2]In adults, the presenting picture is chiefly one of obstructive uropathy, although there may be a suprapubic or perineal mass. Tenesmus, rectal bleeding, and constipation may also be present due to pressure on the rectum. Deep pelvic pain is said to be characteristic.[2]It is quiet challenging to reach the diagnosis and depending on the histological report with specific immunohistochemistry studies. But clinical assessment might give ideas or clue for the suspicion of such this rare disease. In reflect to our case, the diagnosis of non-epithelial prostate tumour need to be in the list at the first place because patient is in middle aged group and the diagnosis of benign prostatic hyperplasia would not be the cause for his symptoms of urinary outflow obstruction. Prostate tissue biopsy should be taken early as the DRE showed it was huge prostate which was not corrersponding to the estimated size according to the age and low level of PSA. Present case is not belongs to a specific type of sarcoma as the histologically shows pleomophic prostate sarcoma with the possible of leiomyosarcoma, synovial sarcoma or stromal sarcoma.Reviewing articles looking at the therapy and survival aspect for these 3 types of prostate sarcoma; which are grouped as non-rhabdomyosarcoma type, and treatment of choice is radical surgery, if complete excision is possible.[2] But in Leiomyosarcoma (LMS) type particularly, it has an aggressive clinical course. Radical surgery is a treatment option, but it is often difficult to completely resect the tumour. Nearly half of patients with resected tumours have gross residual disease after surgery.[1] External beam radiotherapy can be used as the primary modality, or following surgical debulking or incomplete extirpation. Preoperative irradiation and brachytherapy also can be given.[2]The prognosis of primary prostatic sarcoma (excluding rhabdomyosarcoma) is difficult to determine. Patients with rhabdomyosarcomas can probably be cured but those with other histological types of sarcoma eventually succumb to their disease. However, possibly because of the slower growth of these tumours, survival following a variety of therapeutic modalities may often be 5-6 years, sometimes longer.[3,4] If we are looking at survival and prognosis aspect for each differential diagnosis of this patient, Leiomyosarcoma type is more aggressive and has poor prognosis. In the series by John et al., of 14 patients, two presented with metastasis and five subsequently developed metastasis (5–45 months, mean 10.3 months).[5] Of the 14 patients, 10 died of LMS 3–72 months (mean 22 months) after diagnosis. Metastatic sites for LMS include the lung (most common), abdominal wall, brain, lymph nodes, liver, kidney, and bone.[5] In the series by Sexton et al. reported 21 adult prostate sarcomas, including 12 LMSs, in which the 1-year and 5-year actuarial survival rates were 81% and 38%, respectively.[6] Detection of prostatic LMS at an early stage and adequate surgical resection achieved prolonged disease specific survival and may give patients the best chance of cure.[7]For prostatic stromal sarcoma (PSS), Piergiuseppe et al in their case report, their patient had PSS with lung metastasis enabled underwent radical prostatectomy and followed by the radiotherapy and palliative chemotherapy with ifosfamide and liposomal doxorubicin for the lung metastasis.[8] There is only few articles published on the synovial prostate sarcoma but it is about clinicopathology aspect and do not mention about course of disease and the prognosis related.
4. Conclusions
- Prostatic sarcomas are highly aggressive malignant disease and carries poor prognosis. They have very limited therapeutic options. Perhaps, early diagnosis and complete surgical excision may or may not follow by radiotherapy offer better long term survival.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML