-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research In Cancer and Tumor
2013; 2(1): 10-21
doi:10.5923/j.rct.20130201.02
Obstacles to Sustaining Cancer Care Multidisciplinary Team Meetings: An Australian Survey
Tamara Shulman1, Christopher Bain2, Gitesh K. Raikundalia3, Rajesh Sharma1
1Western & Central Melbourne Integrated Cancer Service, Melbourne, 3002, Australia
2Alfred Health, Melbourne, Prahran, 3181, Australia
3College of Engineering and Science, Victoria University, Melbourne, 8001, Australia
Correspondence to: Gitesh K. Raikundalia, College of Engineering and Science, Victoria University, Melbourne, 8001, Australia.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Our aim is to further understand the process, participation and operations of cancer multidisciplinary team meetings in Australia based on the experience and knowledge of participants. Our objective was also to identify obstacles to effective and sustainable multidisciplinary team meetings, particularly how information and communication technology could assist in overcoming these obstacles. We used an online nationwide survey applying a convenience sampling method. While participants in cancer care in Australia believe multidisciplinary team meetings represent best practice cancer care both now and in the future, major obstacles to the sustainability and effectiveness of the model include increased workload and lack of support including financial, administrative and technological. A number of ripple effects of multidisciplinary team meeting implementations threaten the sustainability of this best practice model. We do not believe that these are failures of the model but rather obstacles that can be overcome through the implementation of recommendations that are well worth the effort required. Whilst these obstacles fall into a number of categories, each with potentially unique solutions, improvements in technological support are certainly seen as a key part of the suite of solutions, along with better funding support for participants and more efforts towards improved meeting governance.
Keywords: Australia, Information Systems, Multidisciplinary Communication, Neoplasms, Workload
Cite this paper: Tamara Shulman, Christopher Bain, Gitesh K. Raikundalia, Rajesh Sharma, Obstacles to Sustaining Cancer Care Multidisciplinary Team Meetings: An Australian Survey, Research In Cancer and Tumor, Vol. 2 No. 1, 2013, pp. 10-21. doi: 10.5923/j.rct.20130201.02.
Article Outline
1. Introduction
- Multidisciplinary care (MDC) can be defined as “an integrated team approach to health care in which medical and allied health care professionals consider all relevant treatment options and develop collaboratively an individual treatment plan for each patient”[1]. Multidisciplinary Team Meetings (MDMs) in cancer care are often established to discuss the treatment plan for a patient with cancer by reviewing their physical, supportive care and emotional needs[2]. These meetings are attended by a variety of health professionals who will differ depending on the type of cancer under discussion. Examples of health professionals in attendance could be radiologists, nurses, pathologists, medical oncologists surgeons and allied health and supportive care professionals[3,4]. Allied health professionals primarily include social workers, occupational therapists, physiotherapists, speech pathologists, dieticians, orthotists and music therapists. Various resources, such as radiology films or reports, and pathology samples or reports are brought to the meeting and discussed by the team[5].Substantial evidence has been documented about the ability of MDMs to contribute to better patient survival rates[6], increased patient satisfaction[7], reduced costs[3], increased recruitment into clinical trials[8] and shorter waiting time to treatment[9]. The benefits of this model of care have also been demonstrated in a variety of tumor streams, for example, in lung cancer care[10] and in colorectal cancer care[11]. Work from Scotland[12] also shows that staging of oesophago-gastric cancer was significantly improved through a presentation at a MDM.Based on this evidence, it is difficult to dispute many of the benefits of MDMs; however, one of the anecdotal barriers to clinicians participating in MDMs is the increased workload. There is also an organizational burden involved in planning patient discussions and accessing relevant results for presentation in the meetings, including radiology and pathology findings.To our knowledge, only two published pieces of research regarding workload involved in MDMs for participants are available. Hence, this work is very new and explores an unknown area with regard to workload. First, the work of Nouraei and colleagues[13] investigated increasing the “efficiency” of MDMs for head and neck cancer, based at the Department of Ear, Nose and Throat Surgery at Charing Cross Hospital in London, England. These researchers performed a system analysis of the process behind MDMs. From this, the researchers revised the process and a new intranet-based computer system was developed to support the revised MDM process. The overall efficiency of the MDM was increased by 60%. Efficiency in this context is ‘defined as the ratio of incomplete to total MDM episodes before and after introduction of the database’[13, p. 116].The second piece of research was by Kane[14] who investigated work processes and time requirements for radiologists and pathologists at St James’s Hospital in Dublin, Ireland. The researchers studied and analysed MDMs for one month. They discovered various problems associated with conducting MDMs, such as the enormous amount of time participants spend in meetings, preparing for the meetings and the repeated difficulty in coordinating the availability of material for review.Most work on MDC in Australia has been done for breast cancer. A multidisciplinary team may consist of health care professionals such as a medical oncologist, radiation oncologist, breast care nurse and pathologist[15]. The National Multidisciplinary Care Demonstration Project[16] was a major initiative of the Australian Government Department of Health and Ageing for provision of:• “information about the process, impact, acceptability and cost of the provision of MDC for women with breast cancer in Australia”• “information about MDC that would be applicable to other cancers and other chronic diseases”, and• “recommendations about the implementation of MDC for breast cancer in Australia taking into account possible funding structures” (p. 4)Seven recommendations arose from this Project that assist in exploiting MDC. An example of a recommendation is:• Recommendation 7: models for hospital funding and payment schedules for specialists and general practitioners must be amended to include strategies of MDC.The Australian Government’s national cancer agency, Cancer Australia, offers guidance on the implementation of MDC[17]. Their web site provides:• guides, such as “Multidisciplinary care for advanced disease: a guide for cancer health professionals”• tools and proformas, such as “Treatment plan proforma”• reports, such as “What is multidisciplinary care?”, that can also assist in implementing MDC.In addition to this, there are national- and state-based tools and proformas for implementing MDC. For instance, the Victorian Government has developed a multidisciplinary meeting toolkit that assists in meeting protocols and practice[18]. The Government has also written a 2011 report on the status of MDMs occurring in that state[19].A literature review of work in MDC by the Victorian Government[20] covers a variety of issues in MDC. Certain findings reported, such as insufficiency of administrative support and the need for better documentation, concur with our own findings.Our key overarching goal in conducting an online nationwide survey was to help understand the issues related to workload and other obstacles to the sustainability of the cancer care MDM model in Australia. Once understood, we could make recommendations and direct our effort to address these barriers with a focus on the potential benefits of information and communication technology (ICT).To help understand these obstacles and identify opportunities for improvement, questions were focused on four key themes:• What involvement do clinicians and administrative personnel have in MDMs?;• What are the participants’ views about MDMs?;• What are the issues related to workload that exist in running MDMs?; and,• How is ICT currently used, or may be used, to assist MDMs?These are overarching themes for our study. Our survey contained more specific questions but elicited responses that address these themes.
2. Methods
- An online survey of participants in Australia was used to collect data pertaining to MDMs. The survey had Human Research Ethics Committee (HREC) approval from Victoria University.The web-based survey was developed using the specialist online survey creation tool, Survey Monkey ©[21] . The survey principally contained closed-ended questions that can be found in the Appendix. Participants were able to fill in survey responses from any web-enabled computer to which they had access. At no stage were participants able to be individually identified.A range of recruitment techniques were used including public advertisements at the Clinical Oncological Society of Australia and International Association of Cancer Registries (COSA-IACR) 2008 Joint Scientific Meeting in mid-November 2008. Emails inviting participation were also sent out to relevant groups across Australia in cancer networks, health services and professional bodies and colleges.
3. Results
3.1. Survey Responses and Demographics
- The data was automatically stored electronically by Survey Monkey, and then exported to Microsoft Excel for subsequent initial analysis. In total, 339 surveys were completed. From these responses, an initial distinction was made between respondents who had attended at least one MDM in the last six months (MDM Attendees) and those who had not (non-MDM Attendees). Of the responses received, 267 were ‘MDM Attendees’, 51 were ‘non-MDM Attendees’ and 21 were invalid responses. This distinction was made to target examination and analysis to the responses from MDM Attendees. These individuals were more likely to provide insight into the themes under discussion.
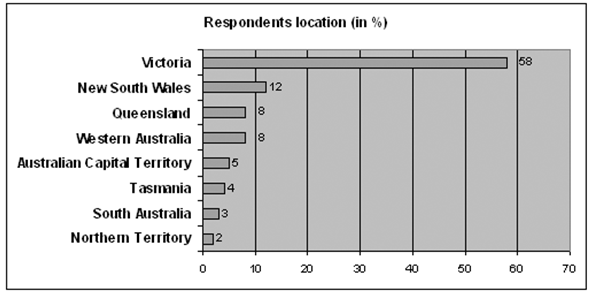 | Figure 1. Respondents’ Location |
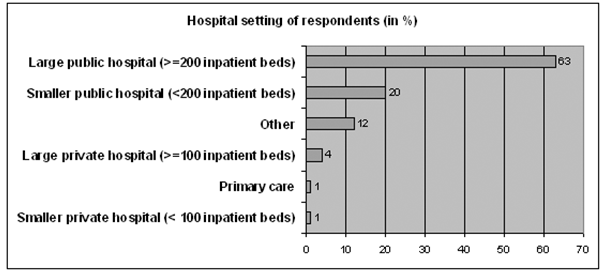 | Figure 2. Hospital setting |
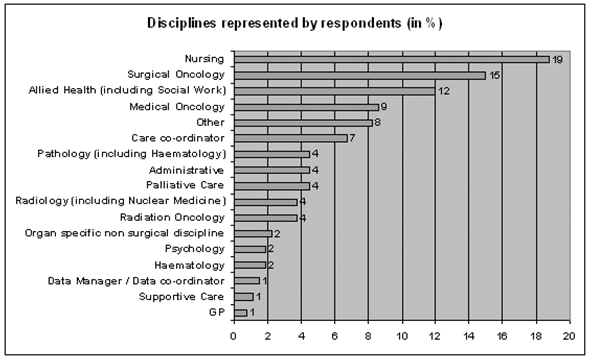 | Figure 3. Respondents’ discipline |
3.2. Limitations of the Research
- There are several important points to note in considering the methods used in conducting this survey and examining its findings.We used a convenience sampling approach in this survey. With this type of approach there is always the risk of sample bias. For instance, it may be that only the most “visible” or opinionated stakeholders have replied to the survey, thus we may have missed quieter or less visible members of the cancer care community. Equally, permeation into certain sub-sections of the cancer community may have been sub-optimal in some cases, despite rigorous efforts to ensure that this did not occur. For example, penetration into the ranks of junior healthcare staff was low despite efforts to target people and programs in charge of junior medical staff.Another limitation is that respondents from the following key stakeholder groups were under-represented:• Remote and rural staff• GPs• Staff from private hospitals• Haematologists• Psychiatrists and Psychologists• Organ specific non-surgical staff (e.g. respiratory physicians, dermatologists and endocrinologists)This may simply reflect the current pattern of MDM implementation or a barrier to successful implementation outlined in the discussion section of this article. Another plausible explanation, however, is that these groups are truly under-represented amongst attendees of MDTs in the Australian context. This would be a finding of note. Further research would be required to delineate which of these two possibilities is in fact the case.We aimed to survey at least 200 MDM participants across Australia and received responses in excess of 330 relevant professionals. This number is sufficient to provide a useful picture of the current state of activities related to MDMs.Despite our frank assessment of the potential limitations of the survey, it should be noted that this is the first work of its kind and we believe it provides an extremely useful initial assessment of the issues confronting those responsible for implementing and sustaining the MDM model in the Australian context, moving the debate down the path from anecdote towards evidence.
4. Discussion
- In this section of the paper we will discuss some of the insights and lessons gleaned from the survey, set against some of the relevant literature. It may appear that some results are conflated with accepted use of information systems. This can be expected since use of information systems is applied to MDMs, and in evaluating MDMs, we are discovering issues related to information systems use.
4.1. Identified Obstacles to the Sustainability of MDMs
- There were two major barriers identified that threaten the sustainability of MDMs. These are increased workload and lack of support. There are also several other obstacles that will be highlighted.
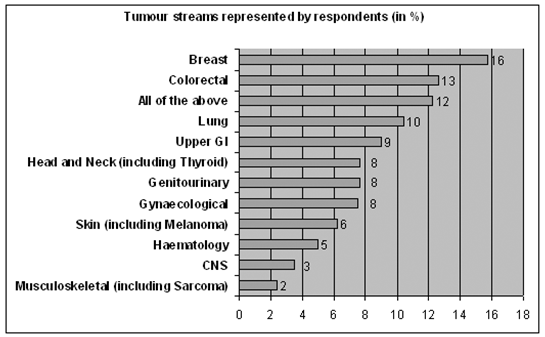 | Figure 4. Tumour streams represented by respondents |
4.1.1. Workload
- The impact of MDMs on workload has not been well anticipated or dealt with by funders and organizations. The majority of participants attend an MDM at least once per week, with nearly 30% attending at least two per week. Over a third of respondents stated that their job plan (“role”) does not contain adequate time to attend MDM meetings. The survey data was further analysed to see if these results were the same when looking at Victoria compared to other states, metropolitan compared to regional respondents and medical compared to non-medical respondents. The only difference detected was that 46% of the medical respondents felt that their job plan does not contain adequate time to attend MDM meetings while this percentage was only 31% for the non-medical respondents.Respondents reported that there is often a lack of understanding and appreciation for the time commitment required that is not reimbursed. This can be a huge strain on small departments such as nuclear medicine or pathology and radiology who have representatives at almost every MDM, which could add up to four meetings a week. One of the respondents commented: “MDTs have had a significant impact on anatomical pathologists time and there has been NO attempt to provide extra funding for extra pathologists or extra assistants within departments for MDTs. My three to four hours a week for MDTs is multiplied in our department of 8 pathologists with between 11 and 14 depending on the week, MDTs serviced by us each week, to a very significant workload that hospitals and government and Cancer Councils have not recognized.”In a report completed by the Western & Central Melbourne Integrated Cancer Service (WCMICS) the conclusion drawn was as follows. At the current time, it is not feasible to implement billing for haematology multidisciplinary meetings using MBS item numbers 871 and 872 at two of the hospitals because of two reasons: (1) The small amount of revenue generated being outweighed by the administration costs of the billing process; (2) The billing requirement of having four medical specialties attend the MDM is unable to be met due to pathology and radiology workforce shortages.It is not only the attendance at a MDM that is creating the issue of workload but there is a great amount of time spent in meeting preparation and follow up as well. Much of the preparation and follow up work is done before or after hours and can often interfere with clinical duties. Approximately 5.6% of respondents spent 60-119 minutes preparing for a MDM and about 10% spent between 30-59 minutes in preparation. Even higher percentages were seen regarding time involved in following up from a MDM. Twenty-seven percent of the respondents spent 30-59 minutes and approximately 10% spent 60-119 minutes in follow up activity per meeting.It would have been interesting to have had more respondents from the junior workforce given they have a significant role in helping to prepare for, run and follow up from these meetings. The recommendation for remuneration for those that are committed to MDMs was consistent across many of the respondents. One representative’s comment was “I believe that the MDT attendance and participation needs to be included in primary expectations of roles and funding for the attendance should be included in clinicians’ remuneration” while another noted “The meetings I attend are after hours and as a non-doctor I am not reimbursed for my attendance.”
4.1.2. Lack of Support
- It was clear from responses that the lack of support for MDMs has a significant impact on the increased workload. The lack of, and need for, administrative support for MDMs was one of the most common topics documented throughout the comments received from the surveys. One respondent observed that MDMs “Have increased work load of consultants significantly. In some cases our MDMs have proven to be unsustainable due to poor attendance of members, lack of admin and IT support etc.” A similar sentiment was echoed by another respondent; “lack of understanding of resources needed to support these meetings particularly in rural regional areas, not efficient to use highly skilled nurses to prepare for MDT meetings.”The critical need for administrative support is in organizing the meeting, booking the room, ensuring participants are aware of the meeting details, ensuring all preparatory work is complete, documenting the discussion of the meeting and following up appropriately. Without someone dedicated to this role, many MDM participants spend extra time engaged in these types of activities or delegate the planning and running of the meetings to junior staff. One survey respondent suggested that “The organization of the meeting needs to incorporate increased preparation time so that people are prepared to discuss the treatment plan at the MDM and the outcome can be obtained quicker.” Fifty-five percent of the respondents agreed that there was too much time involved in having to document all the relevant patient data and information. It was recommended that the administrative support is well versed medically to allow for more independent work with minimal involvement of the participants. Poor administrative support can deter people from attending meetings out of frustration as one respondent note that their radiologist is “constantly annoyed by films not being available and stops coming to meetings.”The role of administrative support is becoming even more critical as technology is being rolled out to support MDMs; conduct of some MDMs becomes more sophisticated by linking together through WebEx © technology and phone conferencing with real-time desktop sharing[22]. Despite the number of comments about meetings being “chaotic and badly organized” as one respondent commented, when respondents were asked whether there was a clear process for discussing patients during the MDM, the majority thought there was a clear process as seen in Figure 5.
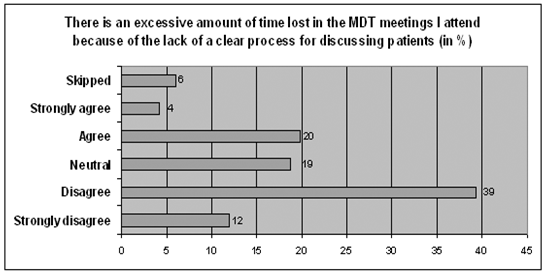 | Figure 5. Time lost in the MDT meetings due to the lack of a clear process for discussing patients |
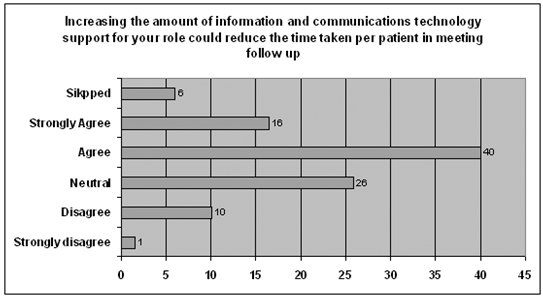 | Figure 6. Reduction in time taken per patient in meeting follow up by increasing the amount of ICT support |
4.2. Recommendations
- After analysing the survey results, we were able to assemble a number of actionable recommendations to address the barriers to successful MDMs in our area of the world. These recommendations are relevant to a range of stakeholders, and any given stakeholder group (clinicians, hospital administrators, policy makers and funders) may have a role in championing, or otherwise supporting, the individual recommendations. For example, in the case of a “Guide to chairing MDMs”, funders could provide financial support for the development of such a guide, clinicians could have a role in providing content input, and hospital administrators could have a role in supporting or even mandating its use in a given health service or facility. It is envisaged that these possible streams of activity represent some practical steps that can be taken to further support the functioning of MDMs, together with attracting further resources in support of them. Implementing these recommendations will be the next phase of work in improving MDM practice. We believe these recommendations are potentially of use nationwide and are as follows:1. Best practice ICT support. ICT support is critical to an effectively run and productive MDM. An audit of the ICT solutions that have been implemented by hospitals to support MDMs and an assessment of their benefits and challenges would help to support hospital decision making. A comprehensive document with detailed information would help to ensure the right decisions are made in selecting the appropriate and effective ICT solutions. This would be extremely timely as many organizations are selecting the software to use to support their MDMs. Even organizations that have implemented software already can benefit as they are constantly seeking to refine and improve their systems.2. Techniques and methods to reduce workload. MDM participants commit copious time and energy into these meetings. Often the workload is intense and above and beyond the normal working hours or days. An assessment of strategies being undertaken by hospitals to reduce workload would be helpful to share and disseminate. This may include reimbursement models or other incentive schemes as well as streamlined processes. There are tremendous amounts of time and energy that go into the preparation, running and follow-up of MDMs. It is evident from the survey results that there is great variability in these practices. Some respondents stated that this type of work “relies entirely on the goodwill of participants”, while other meetings have excellent support staff who organize all aspects of the meetings. Every hospital is unique and there is a great opportunity to learn from others’ best practices.3. Effectiveness review (including economic analysis). Survey responses indicated some skepticism with regard to the cost and clinical effectiveness of MDMs and have discouraged some from accepting and implementing the model. One respondent commented that “It is interesting in an era of evidence-based medicine that MDTs have become accepted as inevitability when the evidence in terms of clinical-effectiveness and cost-effectiveness remains unproven.” Other comments picked up on the variability between MDM practices and that this “is testimony to the lack of evidence for or against them.” This signals the need for an effectiveness review to prove whether these meetings are in fact worth the effort and cost involved.4. Endeavoring to involve allied health staff. Current MDMs are very medically focused and although many allied health staff attend the meetings, they are generally not active participants. Comments from allied health respondents noted that they felt excluded from the discussion and often sit at the back of the room. One nursing staff respondent remarked that they “do not have the opportunity to participate verbally at all and are often made to feel that we should not be there.” It is critical that the time of these integral healthcare workers is not wasted and used in the most efficient way to benefit the patients. Further thought and research needs to go into how to best involve these professionals in MDMs.5. Guide to chairing MDMs. As evident from the survey respondents’ comments, an effective chair is instrumental to the success of a MDM. As one comment noted “the success of a MDTM depends mostly on the leadership of the meeting.” These meetings are complex, involve many participants and occur over a short period of time. The role of the chair can be very challenging and should not be undermined. Becoming an effective chair cannot be expected to come naturally to everyone and it is important to ensure that they are equipped with the tools and knowledge to run an effective MDM. This should also assist in reducing meeting variability. One respondent’s comment after observing a number of different meetings over a year “is that there is a great need for training of some of the meeting leaders.”
5. Conclusions
- From the results of this research we conclude that MDMs are viewed as a core and essential part of best practice cancer management. However, we also conclude that, based on a nationwide online survey, the innovation of MDMs has been accompanied by some unintended consequences that threaten the sustainability of the model. We do not believe that these are failures of the model but rather obstacles that can be overcome through the implementation of recommendations that are well worth the effort required.Whilst these obstacles fall into a number of categories, each with potentially unique solutions, improvements in ICT support are certainly seen as key part of the suite of solutions, along with better funding support for participants, and more efforts towards improved meeting governance. These findings represent a challenge for governments, health services and all participants in MDMs in terms of implementing effective change.
ACKNOWLEDGEMENTS
- We wish to acknowledge the support of the staff of the WCMICS Directorate in undertaking this work, in particular the efforts of Michelle Fleming who was heavily involved early on in the work.
Appendix
- Questionnaire: Australia Wide Cancer MDT Workforce and Workflow Survey Section 1 - Demographics and BackgroundMy age group• <30• 31-40• 41-50• 51-60• 60+My gender• Male • Female My state (Tick more than one if applicable, for e.g. if you work in the border area)• QLD• SA• VIC• NSW• NT• TAS• WA• ACTThe geographic setting in which I predominantly work is:• Regional/Rural • Inner metropolitan • Outer metropolitan• RemoteThe healthcare delivery setting in which I predominantly work is:• large public hospital (>=200 inpatient beds)• smaller public hospital (<200 inpatient beds) • large private hospital (>=100 inpatient beds)• smaller private hospital (< 100 inpatient beds) • primary care• OtherMy primary professional group is: {skips to specific questions for medical disciplines and nursing disciplines, e.g., consultant, registrar, resident, etc.} • Medical Oncology• Hematology• Radiation Oncology• Surgical Oncology• Organ specific non surgical discipline (e.g., Respiratory Medicine, Dermatology)• Palliative Care• Nursing• Allied Health (including Social Work) • Administrative• GP• Radiology (including Nuclear Medicine)• Pathology (including Hematology) • Psychiatry• Psychology• Supportive Care • OtherSkip Questions(Medical discipline)I am• Consultant or• Registrar or• Resident(Nursing discipline)My primary discipline is• Ward Staff• Outpatient Staff• Chemotherapy Day Unit• Clinical Nurse Consultant• Nurse practitioner(Allied Health)My primary discipline is• Social Work• Occupational Therapy•
 Physiotherapy• Speech pathology• Audiology• Pharmacy• Other(GP)I am • Fully qualified• RegistrarWhat tumor group(s) or stream(s) do you predominantly work with?:• Genitourinary• Lung• CNS• Hematology• Breast• Skin (including Melanoma)• Musculoskeletal (including Sarcoma)• Upper GI• Colorectal• Gynaecological• Head and Neck (including Thyroid)• All of the aboveDo you attend MDT meetings (at least 1 in the last 6 months) for the discussion of cancer patients in “your” or “other” organization? NoYes (please specify 1 for private. 2 for public or 3 for both)If no to both, thank you for participating, otherwise please continue with survey.Section 2 - MDT Meeting InvolvementThe geographic setting in which you predominantly attend MDT meetings is:• Regional/Rural • Inner metropolitan • Outer metropolitan • RemoteThe healthcare delivery setting in which you predominantly attend MDT meetings is:• large public hospital (>=200 inpatient beds)• smaller public hospital (<200 inpatient beds) • large private hospital (>=100 inpatient beds)• smaller private hospital (< 100 inpatient beds) • collaborative, across multiple organizations (entirely virtual)Your job role in relation to the MDT meetings you attend is predominantly (tick as many as apply)• Meeting support, e.g., administrative role• Data management, e.g., data manager, data collection• Clinical expertise – regarding patient management – medical and nursing • Clinical expertise – regarding patient management – allied health • Diagnostic service expertise including radiology, pathology, hematology and nuclear medicine• Information recipient, e.g., to understand more about the patients you care for or will be required to assess • Other – please state How often have you attended MDT meetings for the discussion of cancer patients in the last year? • Once every 6 months or less• Between once every 6 months and once every 2 months• About once per month • About once per fortnight• About once per week • Twice per week • Between 3 and 5 times per week • More than 5 times per week How long do these meetings last on average? • Less than 30 minutes • 30-60 minutes • 60-90 minutes • More than 90 minutes At these meetings, how long is each patient discussed for on average? • Less than 5 minutes • 5-10 minutes • 10-30 minutes • 30- 50 minutes • Greater than 50 minutesPlease indicate on the scale below, the extent to which you concur with the following statementThe extent to which information and communications technologies currently support your role in relation to the conduct of the meetings.• Extremely unsupportive • Unsupportive • Neither supportive nor unsupportive, • Supportive• Extremely supportive Please indicate on the scale below, the extent to which you concur with the following statementIncreasing the amount of information andcommunications technology support for your role could reduce the time taken per patient in the conduct of the meetings• Strongly disagree• Disagree• Neutral• Agree• Strongly agree In the MDT meetings you predominantly attend, how is patient related data and information documented during the meeting most commonly:• Written by hand for subsequent use • Written by hand for subsequent (after the meeting) manual entry into an electronic medium• Written by hand for subsequent (after the meeting) scanning by scanning software • Entered directly into a relevant electronic vehicle by a member of the administrative or data management staff • Entered directly into a relevant electronic vehicle by a member of the clinical staff • Other – please state Section 3 - MDT Meeting Preparation Participants in MDT meetings may be involved in a range of preparatory activities to be ready for MDT meetings. Such activities could include:• documenting information to be presented at the meeting• booking facilities (including rooms and video conferencing links)• collating information (including investigation results) from multiple sources • notifying patients so that may attend • informing participants of meeting arrangements How much of your time is involved in preparatory activities for the meetings you attend on average? • Less than 30 minutes per meeting • 30-59 minutes per meeting • 60-119 minutes per meeting • 120-179 minutes per meeting• 180-239 minutes per meeting • More than 240 minutes per meetingPlease indicate on the scale below, the extent to which information and communications technologies currently support your role in relation to meeting preparation. (1 = extremely unsupportive, 3 = neither supportive nor unsupportive, 5 = extremely supportive)
Physiotherapy• Speech pathology• Audiology• Pharmacy• Other(GP)I am • Fully qualified• RegistrarWhat tumor group(s) or stream(s) do you predominantly work with?:• Genitourinary• Lung• CNS• Hematology• Breast• Skin (including Melanoma)• Musculoskeletal (including Sarcoma)• Upper GI• Colorectal• Gynaecological• Head and Neck (including Thyroid)• All of the aboveDo you attend MDT meetings (at least 1 in the last 6 months) for the discussion of cancer patients in “your” or “other” organization? NoYes (please specify 1 for private. 2 for public or 3 for both)If no to both, thank you for participating, otherwise please continue with survey.Section 2 - MDT Meeting InvolvementThe geographic setting in which you predominantly attend MDT meetings is:• Regional/Rural • Inner metropolitan • Outer metropolitan • RemoteThe healthcare delivery setting in which you predominantly attend MDT meetings is:• large public hospital (>=200 inpatient beds)• smaller public hospital (<200 inpatient beds) • large private hospital (>=100 inpatient beds)• smaller private hospital (< 100 inpatient beds) • collaborative, across multiple organizations (entirely virtual)Your job role in relation to the MDT meetings you attend is predominantly (tick as many as apply)• Meeting support, e.g., administrative role• Data management, e.g., data manager, data collection• Clinical expertise – regarding patient management – medical and nursing • Clinical expertise – regarding patient management – allied health • Diagnostic service expertise including radiology, pathology, hematology and nuclear medicine• Information recipient, e.g., to understand more about the patients you care for or will be required to assess • Other – please state How often have you attended MDT meetings for the discussion of cancer patients in the last year? • Once every 6 months or less• Between once every 6 months and once every 2 months• About once per month • About once per fortnight• About once per week • Twice per week • Between 3 and 5 times per week • More than 5 times per week How long do these meetings last on average? • Less than 30 minutes • 30-60 minutes • 60-90 minutes • More than 90 minutes At these meetings, how long is each patient discussed for on average? • Less than 5 minutes • 5-10 minutes • 10-30 minutes • 30- 50 minutes • Greater than 50 minutesPlease indicate on the scale below, the extent to which you concur with the following statementThe extent to which information and communications technologies currently support your role in relation to the conduct of the meetings.• Extremely unsupportive • Unsupportive • Neither supportive nor unsupportive, • Supportive• Extremely supportive Please indicate on the scale below, the extent to which you concur with the following statementIncreasing the amount of information andcommunications technology support for your role could reduce the time taken per patient in the conduct of the meetings• Strongly disagree• Disagree• Neutral• Agree• Strongly agree In the MDT meetings you predominantly attend, how is patient related data and information documented during the meeting most commonly:• Written by hand for subsequent use • Written by hand for subsequent (after the meeting) manual entry into an electronic medium• Written by hand for subsequent (after the meeting) scanning by scanning software • Entered directly into a relevant electronic vehicle by a member of the administrative or data management staff • Entered directly into a relevant electronic vehicle by a member of the clinical staff • Other – please state Section 3 - MDT Meeting Preparation Participants in MDT meetings may be involved in a range of preparatory activities to be ready for MDT meetings. Such activities could include:• documenting information to be presented at the meeting• booking facilities (including rooms and video conferencing links)• collating information (including investigation results) from multiple sources • notifying patients so that may attend • informing participants of meeting arrangements How much of your time is involved in preparatory activities for the meetings you attend on average? • Less than 30 minutes per meeting • 30-59 minutes per meeting • 60-119 minutes per meeting • 120-179 minutes per meeting• 180-239 minutes per meeting • More than 240 minutes per meetingPlease indicate on the scale below, the extent to which information and communications technologies currently support your role in relation to meeting preparation. (1 = extremely unsupportive, 3 = neither supportive nor unsupportive, 5 = extremely supportive)  Increasing the amount of information andcommunications technology support for your role could reduce the time taken per patient in meeting preparation. Please indicate below the extent to which you agree with this statement: (1 = strongly disagree, 3 = neutral, 5 = strongly agree)
Increasing the amount of information andcommunications technology support for your role could reduce the time taken per patient in meeting preparation. Please indicate below the extent to which you agree with this statement: (1 = strongly disagree, 3 = neutral, 5 = strongly agree)  Section 4 - MDT Meeting Follow Up Participants in MDT meetings may be involved in a range of follow up activities after the completion of MDT meetings. Such activities could include:• documenting information to be presented at the meeting (on paper or electronically) • booking investigations and following up results • notifying patients of the meeting recommendations• filing paperwork (e.g., in the patient’s paper record) • sending letters to participants or GPs How much of your time is involved in follow up activities for the meetings you attend on average • Less than 30 minutes per meeting • 30-59 minutes per meeting • 60-119 minutes per meeting • 120-179 minutes per meeting• 180-239 minutes per meting • More than 240 minutes per meeting Please indicate on the scale below, the extent to which information and communications technologies currently support your role in relation to meeting follow up. (1 = extremely unsupportive, 3 = neither supportive nor unsupportive, 5 = extremely supportive)
Section 4 - MDT Meeting Follow Up Participants in MDT meetings may be involved in a range of follow up activities after the completion of MDT meetings. Such activities could include:• documenting information to be presented at the meeting (on paper or electronically) • booking investigations and following up results • notifying patients of the meeting recommendations• filing paperwork (e.g., in the patient’s paper record) • sending letters to participants or GPs How much of your time is involved in follow up activities for the meetings you attend on average • Less than 30 minutes per meeting • 30-59 minutes per meeting • 60-119 minutes per meeting • 120-179 minutes per meeting• 180-239 minutes per meting • More than 240 minutes per meeting Please indicate on the scale below, the extent to which information and communications technologies currently support your role in relation to meeting follow up. (1 = extremely unsupportive, 3 = neither supportive nor unsupportive, 5 = extremely supportive)  Increasing the amount of information and communications technology support for your role could reduce the time taken per patient in meeting follow up. Please indicate below the extent to which you agree with this statement: (1 = strongly disagree, 3 = neutral, 5 = strongly agree)
Increasing the amount of information and communications technology support for your role could reduce the time taken per patient in meeting follow up. Please indicate below the extent to which you agree with this statement: (1 = strongly disagree, 3 = neutral, 5 = strongly agree)  Section 5 – Opportunities to Examine the Workload on MDT Participants Please indicate the extent to which you concur with the following statements on the 1 to 5 scale (1 = Strongly disagree, 3 = neutral, 5 = Strongly agree). All questions are in relation to the MDT meetings you predominantly attend. • There is an excessive number of patients who require an additional or re-discussion at the MDT meetings I attend (e.g., because the right staff were not present, the right information was not present)
Section 5 – Opportunities to Examine the Workload on MDT Participants Please indicate the extent to which you concur with the following statements on the 1 to 5 scale (1 = Strongly disagree, 3 = neutral, 5 = Strongly agree). All questions are in relation to the MDT meetings you predominantly attend. • There is an excessive number of patients who require an additional or re-discussion at the MDT meetings I attend (e.g., because the right staff were not present, the right information was not present)  • There is an excessive amount of time lost in the MDT meetings I attend because of sub optimal leadership of the meeting
• There is an excessive amount of time lost in the MDT meetings I attend because of sub optimal leadership of the meeting  • There is an excessive amount of time lost in the MDT meetings I attend because of the lack of a clear process for discussing patients
• There is an excessive amount of time lost in the MDT meetings I attend because of the lack of a clear process for discussing patients • There is too much time involved in tracking down or preparing the radiology (including CT) and PET results required for discussion in the MDT meetings I attend
• There is too much time involved in tracking down or preparing the radiology (including CT) and PET results required for discussion in the MDT meetings I attend • There is too much time involved in tracking down or preparing the pathology (including hematology) results required for discussion in the MDT meetings I attend
• There is too much time involved in tracking down or preparing the pathology (including hematology) results required for discussion in the MDT meetings I attend • There is too much time involved in having to document or collate all the relevant patient data and information (e.g., clinical history, referral letters, previous meeting discussions) before the MDT meetings I attend
• There is too much time involved in having to document or collate all the relevant patient data and information (e.g., clinical history, referral letters, previous meeting discussions) before the MDT meetings I attend • There is too much time involved in having to document all the relevant patient data and information (including proposed treatment plans and needs) during the MDT meetings I attend
• There is too much time involved in having to document all the relevant patient data and information (including proposed treatment plans and needs) during the MDT meetings I attend • There is too much time involved in having to document all the relevant patient data and information (e.g., the patients’ consent for the treatment plan, the fact that certain recommended investigations occurred and what the results were) after MDT meetings I attend
• There is too much time involved in having to document all the relevant patient data and information (e.g., the patients’ consent for the treatment plan, the fact that certain recommended investigations occurred and what the results were) after MDT meetings I attend • There is too much time involved in preparing correspondence to relevant organizations or individuals (e.g., referring external specialists, or GPs) as a result of the MDT meetings I attend
• There is too much time involved in preparing correspondence to relevant organizations or individuals (e.g., referring external specialists, or GPs) as a result of the MDT meetings I attend At our MDT meetings we discuss the following patient groups (Macaskill 2006) – please circle all answers that are relevant: • all new• some new• all benign• some benign• all recurrence• some recurrenceSection 6 - Participant Support for MDT meetingsThe following questions address the level of participant support for the MDT meeting concept.For each of the following questions, please indicate on the 1 to 5 scale (1 = absolutely disagree, 3 = unsure, 5 = absolutely agree) the extent to which you concur with the following statements • MDTs improve the quality of care received by patients
At our MDT meetings we discuss the following patient groups (Macaskill 2006) – please circle all answers that are relevant: • all new• some new• all benign• some benign• all recurrence• some recurrenceSection 6 - Participant Support for MDT meetingsThe following questions address the level of participant support for the MDT meeting concept.For each of the following questions, please indicate on the 1 to 5 scale (1 = absolutely disagree, 3 = unsure, 5 = absolutely agree) the extent to which you concur with the following statements • MDTs improve the quality of care received by patients  • The advent of the MDT has had a positive effect on my morale
• The advent of the MDT has had a positive effect on my morale • The advent of the MDT has had a positive impact on training
• The advent of the MDT has had a positive impact on training • MDTs are cost effective
• MDTs are cost effective • I do not believe MDTs are a passing fad
• I do not believe MDTs are a passing fad • My job plan (‘role’) contains adequate time to attend MDT meetings
• My job plan (‘role’) contains adequate time to attend MDT meetings
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML