-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2023; 13(2): 51-62
doi:10.5923/j.phr.20231302.02
Received: Sep. 6, 2023; Accepted: Sep. 21, 2023; Published: Sep. 22, 2023

Drivers of a Functional Integrated HIV/NCDs Care Model for a Sustainable Healthcare System; Lessons from Nakuru County, Kenya
Njuguna David1, 2, Caroline Kawila Kyalo2, Eunice Muthoni Mwangi3
1Department of Planning, Ministry of Health, Nairobi, Kenya
2Department of Health Systems Management, School of Medicine and Health Sciences, Kenya Methodist University, Nairobi, Kenya
3Department of Population Health, Aga Khan University, East Africa
Correspondence to: Njuguna David, Department of Planning, Ministry of Health, Nairobi, Kenya.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Healthcare financing and resourcing have always been of great concern to low- and middle-income countries and households. Stakeholders must devise innovative ways to remain in operation amidst reducing financing and dynamic disease etiology to ensure that there is consistent access to quality healthcare services. The integration of Human Immunodeficiency Virus (HIV) and non-communicable disease (NCD) services has emerged as a crucial approach to optimize healthcare delivery and improve health outcomes. NCD and Human HIV programs are currently managed separately, despite frequent interconnections. The study aimed to conduct a regression analysis of an HIV/NCD integration model for healthcare providers to improve the performance of healthcare services in Nakuru County. Methods: This study explains the effect of the explanatory variables - institutional support, health information processes, pooled resources, and collaboration-on the explained variable- Healthcare System performance-, utilizing a multiple regression model. Organizational culture was also used to moderate the relationship between the explanatory variables and the explained variable. Data were collected from a representative sample of 123 healthcare workers drawn from 106 healthcare facilities providing both HIV/NCD services in Nakuru County, Kenya. The explanatory and moderating variables were selected based on their potential to influence healthcare system performance. The regression models were adjusted for potential confounding variables to ensure the robustness of the findings. Results: In the Multivariate analysis, organizational culture was significant in moderating the relationship between the integration of health services and the performance of the healthcare system, with a p-value of less than 0.05. Specifically, health facilities that embraced a team-oriented organization culture in delivering HIV/NCD service treatment and care were 2.142 times more likely to achieve sustainability of the services as compared to those that did not adopt a team-oriented organization culture. These results were statistically significant at a 95 percent confidence level. The findings of the study also revealed that institutional support in monitoring outcomes had a positive and significant influence on the performance of the healthcare system. Health information processes have a significant influence on healthcare system performance in Nakuru County. Health facilities that utilized functioning information systems during the provision of HIV/NCD services were 1.987 times more likely to achieve sustainability of the services compared to those without such systems. The findings also indicate that the performance of the healthcare system in Nakuru County was significantly influenced by human resources and funding models. Conversely, the findings suggest that there is no significant association between the collaboration guidelines and the performance of the healthcare system in Nakuru County. Conclusions: This study highlights the importance of cultivating a team-oriented organizational culture within healthcare facilities and a need for institutional support. Additionally, the availability and the ability to leverage on available resources contribute greatly to the sustainability of services, leading to a better-performing healthcare system. These findings can guide healthcare providers in developing strategies and interventions to enhance the integration of health services and improve overall healthcare outcomes.
Keywords: HIV, NCDs, Integration, Healthcare System, Performance
Cite this paper: Njuguna David, Caroline Kawila Kyalo, Eunice Muthoni Mwangi, Drivers of a Functional Integrated HIV/NCDs Care Model for a Sustainable Healthcare System; Lessons from Nakuru County, Kenya, Public Health Research, Vol. 13 No. 2, 2023, pp. 51-62. doi: 10.5923/j.phr.20231302.02.
Article Outline
1. Introduction
- The prevalence of non-communicable diseases (NCDs) on a global scale is persistently rising, resulting in approximately 41 million deaths every year. This staggering number accounts for approximately 71% of all deaths worldwide [1]. The rise in the burden of NCD among HIV-positive people is evident therefore, integrating these two services will improve efficiency and enhance the utilization of NCD services [2]. Vertical care for HIV in sub-Saharan Africa has enabled health services to concentrate their resources on addressing a single condition. This targeted approach, coupled with the implementation of differentiated models of care that facilitate convenient access to medications for people living with HIV (PLHIV), has resulted in positive outcomes for this population. However, effectively managing NCDs among PLHIV remains a significant health system challenge in the region [3].The determinants of HIV/NCD integration are multifaceted and influenced by various factors, including epidemiological, health system, and socio-cultural considerations. The health system factors significantly impact the integration of HIV and NCDs care. Consequently, integration processes in service delivery depend substantially for their success on the characteristics of the health systems in which they are embedded [4]. Health systems in sub-Saharan Africa often face limited resources, including healthcare personnel, infrastructure, and funding. Shortage in staff numbers was also found to be a barrier to integrated care in Tanzania as well as in Thailand [5,6]. The vertical care model, which has been successful in managing HIV, may pose challenges when integrating NCDs care due to its specialized focus. Health system strengthening, capacity building, and resource allocation are vital for facilitating the integration of services, ensuring access to essential medications, and enabling coordinated care for individuals living with both HIV and NCDs.Effective governance and leadership play a crucial role in shaping healthcare system performance in the integrated care model for HIV/NCD. Governance models influence choices, consents and approaches, responsibility, reporting and authority. Even though it is a constitutional requirement that it is a medical requirement and patients' access to health services, programs define integrated services differently [7]. Clear lines of accountability, strong leadership, and effective governance structures are essential for coordinating and aligning efforts across different healthcare sectors and stakeholders. Collaboration between public health authorities, healthcare providers, community organizations, and civil society is vital for promoting integrated care, ensuring resource allocation, and implementing evidence-based practices. Adequate governance mechanisms and leadership strategies that foster collaboration and coordination are fundamental for achieving high-performance healthcare systems in the integrated care model. Insufficient political commitment, and leadership required to integrate NCD services at the Primary Health Care (PHC) level and weaknesses in governance structures, intersectoral coordination and funding have been identified as health system barriers to integration of NCD to PHC services [8].Accurate and timely information is a critical component of healthcare system performance in the integrated care model for HIV/NCDs. A health information system integrates data from personal records, facility services and organizational records for policymaking and healthcare services management [9]. Robust health information systems that capture and exchange relevant data and facilitate information sharing among different healthcare providers and sectors are essential. Comprehensive electronic health records, interoperability of systems, and standardized data collection and reporting tools enable effective monitoring, evaluation, and quality improvement. Additionally, health information systems that prioritize patient-centered care and facilitate shared decision-making can enhance patient engagement and empowerment, leading to improved health outcomes. However, a study by [10] observed that in the attempt to create an integrated encounter patient form, healthcare providers were overburdened by the level of information required in one form, hence forms were eventually separated to be disease-specific.The availability, distribution, and capacity of the healthcare workforce significantly impact healthcare system performance in the integrated care model for HIV/NCDs. Adequate staffing levels, appropriate skill mix, and ongoing professional development are crucial for delivering high-quality integrated care. Training programs that equip healthcare providers with the necessary knowledge and skills to manage both HIV and NCDs are essential. Additionally, interdisciplinary collaboration and team-based care models promote effective communication, coordination, and continuity of care. Strengthening the health workforce and investing in capacity building initiatives are key determinants of healthcare system performance in the integrated care model [11].Understanding the drivers of healthcare system performance in the integrated healthcare model is essential for optimizing care delivery and sustaining service delivery. Contextual factors governance and leadership, financing models, health information systems, and the health workforce all play significant roles in shaping the performance of the healthcare system. Understanding the drivers of integration is essential for developing effective strategies to address the complex healthcare needs of individuals living with long term conditions. The knowledge also contributes to the broader goal of achieving universal health coverage and promoting health equity, ensuring that individuals living with long-term conditions have equitable access to quality care and services. Regression analysis offers a valuable approach to understanding the drivers of HIV/NCD service integration. By examining the relationships between various factors, stakeholders can gain insights into the key drivers and barriers to health services integration. As such, this study aimed to assess the drivers of healthcare system performance in an integrated care model for HIV/NCDs in Nakuru County in Kenya with a purpose to leverage on the available resources and sustaining service delivery.
2. Methods
- Study Design This was a cross sectional study, with mixed methods approach. The study employed Philosophy of positivism and interpretivism approaches, to best understand the health system performance as well as investigate the extent to which explanatory variable influences the endogenous variable. An exploratory design was applied to test the hypothesis developed while a descriptive design will be applied to quantify outcomes. Correlations revealed the relationship between the explanatory and endogenous variables [12]. According to Isaac and Michael (1995), descriptive studies systematically describe a research interest accurately [13]. Therefore, the study design provided an opportunity for detecting the strength of the relationship between the explanatory and endogenous variables. The goal was to make prediction on which variable to invest on more for improved healthcare system performance. The study design adopted gave a thorough and accurate description by determining what, why and how the situation could be improved and also ensures that there was minimum bias in collection of data.Target PopulationThe study target population was 146 facilities involved in HIV/NCD care at the healthcare facilities having Comprehensive Care Clinics (CCCs) in Nakuru County. The facilities have common observable characteristics. Nakuru county was selected due to high HIV/NCD comorbidities.Inclusion Criteria i. Licensed healthcare providers of all cadres involved in HIV and NCD service delivery per site.ii. Willingness to give informed written consent.Exclusion Criteria i. Students, interns, casual employees ii. Unwilling to give informed consent.There was no provision for substitution of sampled study participants and there was no replacement of the preselected study participants.Sample Size Determination The study was conducted at the health facilities in Nakuru county which had a total of 146 health facilities with a HIV clinic. The sample size (n) for the health facilities was calculated using the Cochran formula shown below.
 Where;n =Sample sizeN =Population sizep =Average proportion of records expected to meet the criteria. 50% or 0.5 is recommended if the prevalence is unknown.e = Margin of error deemed to be acceptable. In this case, we used 5%.Z =is a mathematical constant defined by the confidence interval. In this case, we used 1.96 for a 95% confidence level.Calculationsi. First estimate where population size is not known.
Where;n =Sample sizeN =Population sizep =Average proportion of records expected to meet the criteria. 50% or 0.5 is recommended if the prevalence is unknown.e = Margin of error deemed to be acceptable. In this case, we used 5%.Z =is a mathematical constant defined by the confidence interval. In this case, we used 1.96 for a 95% confidence level.Calculationsi. First estimate where population size is not known.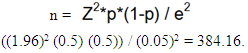 ii. Finite population correction (for known population size)
ii. Finite population correction (for known population size)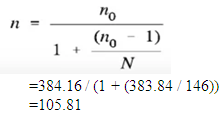 iii. Adjust for design effect (DEFF) DEFF is the extent to which the sampling error departs from the sampling error used in simple random sampling. For simple random or stratified random samples, the value is 1.0 as we do not account for DEFF. For cluster samples, 2.0 is recommended where cluster samples are small and numerous. = n*D= 105.81 *1Thus n =105.81iv. Expected response rate.The expected response rate for this study will be 100% or 1. Thus the sample size after adjusting for response rate was. =n /1 =105.81/1=105.81Using the above formula, a total of 106 out of 146 facilities were included in the study. From the 106 facilities, two respondents at each facility were targeted, two filled the structured questionnaire. These respondents were the Facility in charge, healthcare workers stationed at the CCC and or health care worker at the facility. A total of 212 healthcare providers were expected to complete the structured questionnaires in the study. Data CollectionPrimary data collection was done using a structured questionnaire with questions on demographic characteristics, explanatory and endogenous variables. An electronic data collection approach using an Open Data Kit (ODK) mobile phone data collection and analysis platform was employed to facilitate fast data entry, integration, processing for real time usage, allowing analysis with minimal need for further data cleaning and faster modification based on real time feedback. Data collection took place between Month of February and May 2023. The researcher asked questions, filled in, and completed a form per respondent through the ODK collect app on the mobile phone after login into the app. Completing the questionnaire in the ODK took place both online and offline depending on the internet connectivity. Once the form has duly been filled it was uploaded when the connectivity to internet is secure and marked sent on ODK collect app. The researcher was able to edit the sent forms although they can be viewed until they are deleted in the platform. The duly filled questionnaire was transmitted to SPSS for secure storage and analysis. Data was edited, examined for errors and omission then cleaned up. Data was subjected to statistical analysis and descriptive analysis using SPPS. Data was subjected to descriptive and qualitative analysis.Ethical Considerations This study upheld ethical standards at all stages of implementation (A. Mugenda, 2008) and sought formal approval from the KeMU Science and Ethics Review Committee (SERC) approval number KEMU/ SERC/ HSM/27/ 2022, the National Council of Science, Technology and Innovation (NACOSTI) License number NACOSTI/P/23/22899 and the County Department of Health (REF:NCG/CDPH/RES/VOL.1/2023/667) as well as Health facilities. Assurance on confidentiality on feedback provided by respondents was done as informed consent was sort from them. Data collected was kept confidential and only the researcher has access. Study results will be communicated through Kenya Methodist University devoid of falsification of data, manipulation of data analysis or misrepresentation of results.Data AnalysisA Chi-square test was done to determine the relationship between the variables affecting HIV/NCDs services integration. Bivariate logistic regression analysis to determine variance in the identified variables was conducted. A p-value of 0.05 was set for statistical significance.To test the hypotheses, two conditions were set such that given H0 and H1, set α = 0.05, the rule is that reject H0 if the p-value is less than α else fail to reject H0: where.1. H0: Null Hypothesis: H0i: βi =0. Where, (i=1, 2, 3, 4, 5)2. H1: Alternative Hypothesis: H1i: βi ≠ 0. Where, (i = 1, 2, 3, 4, 5)For a binary logistic regression output of P > 0.05, reject the null hypothesis H0 and accept alternative hypothesis H1 otherwise fail to reject the null hypothesis H0 for P-values less than 0.05. The regression output provides the corresponding p-values while the Nagelkerke R squared was used to determine statistical significance for each explanatory variable.Empirical ModelsWhen determining the influence of health care services integration for improved health system performance in Nakuru County the binary logistic regression model was utilized. Health system performance was measured in terms of its sustainability. In this model, the sustainability score was=0 if the healthcare system was not sustainable and was =1 if the healthcare system was deemed to be sustainable. In this investigation, the hypothesized empirical relationship can be illustrated as follows:
iii. Adjust for design effect (DEFF) DEFF is the extent to which the sampling error departs from the sampling error used in simple random sampling. For simple random or stratified random samples, the value is 1.0 as we do not account for DEFF. For cluster samples, 2.0 is recommended where cluster samples are small and numerous. = n*D= 105.81 *1Thus n =105.81iv. Expected response rate.The expected response rate for this study will be 100% or 1. Thus the sample size after adjusting for response rate was. =n /1 =105.81/1=105.81Using the above formula, a total of 106 out of 146 facilities were included in the study. From the 106 facilities, two respondents at each facility were targeted, two filled the structured questionnaire. These respondents were the Facility in charge, healthcare workers stationed at the CCC and or health care worker at the facility. A total of 212 healthcare providers were expected to complete the structured questionnaires in the study. Data CollectionPrimary data collection was done using a structured questionnaire with questions on demographic characteristics, explanatory and endogenous variables. An electronic data collection approach using an Open Data Kit (ODK) mobile phone data collection and analysis platform was employed to facilitate fast data entry, integration, processing for real time usage, allowing analysis with minimal need for further data cleaning and faster modification based on real time feedback. Data collection took place between Month of February and May 2023. The researcher asked questions, filled in, and completed a form per respondent through the ODK collect app on the mobile phone after login into the app. Completing the questionnaire in the ODK took place both online and offline depending on the internet connectivity. Once the form has duly been filled it was uploaded when the connectivity to internet is secure and marked sent on ODK collect app. The researcher was able to edit the sent forms although they can be viewed until they are deleted in the platform. The duly filled questionnaire was transmitted to SPSS for secure storage and analysis. Data was edited, examined for errors and omission then cleaned up. Data was subjected to statistical analysis and descriptive analysis using SPPS. Data was subjected to descriptive and qualitative analysis.Ethical Considerations This study upheld ethical standards at all stages of implementation (A. Mugenda, 2008) and sought formal approval from the KeMU Science and Ethics Review Committee (SERC) approval number KEMU/ SERC/ HSM/27/ 2022, the National Council of Science, Technology and Innovation (NACOSTI) License number NACOSTI/P/23/22899 and the County Department of Health (REF:NCG/CDPH/RES/VOL.1/2023/667) as well as Health facilities. Assurance on confidentiality on feedback provided by respondents was done as informed consent was sort from them. Data collected was kept confidential and only the researcher has access. Study results will be communicated through Kenya Methodist University devoid of falsification of data, manipulation of data analysis or misrepresentation of results.Data AnalysisA Chi-square test was done to determine the relationship between the variables affecting HIV/NCDs services integration. Bivariate logistic regression analysis to determine variance in the identified variables was conducted. A p-value of 0.05 was set for statistical significance.To test the hypotheses, two conditions were set such that given H0 and H1, set α = 0.05, the rule is that reject H0 if the p-value is less than α else fail to reject H0: where.1. H0: Null Hypothesis: H0i: βi =0. Where, (i=1, 2, 3, 4, 5)2. H1: Alternative Hypothesis: H1i: βi ≠ 0. Where, (i = 1, 2, 3, 4, 5)For a binary logistic regression output of P > 0.05, reject the null hypothesis H0 and accept alternative hypothesis H1 otherwise fail to reject the null hypothesis H0 for P-values less than 0.05. The regression output provides the corresponding p-values while the Nagelkerke R squared was used to determine statistical significance for each explanatory variable.Empirical ModelsWhen determining the influence of health care services integration for improved health system performance in Nakuru County the binary logistic regression model was utilized. Health system performance was measured in terms of its sustainability. In this model, the sustainability score was=0 if the healthcare system was not sustainable and was =1 if the healthcare system was deemed to be sustainable. In this investigation, the hypothesized empirical relationship can be illustrated as follows: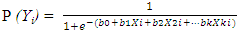 | (1) |
3. Findings
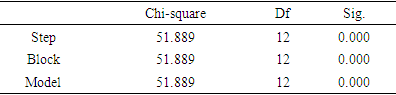
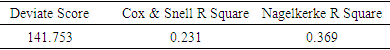
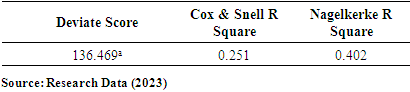
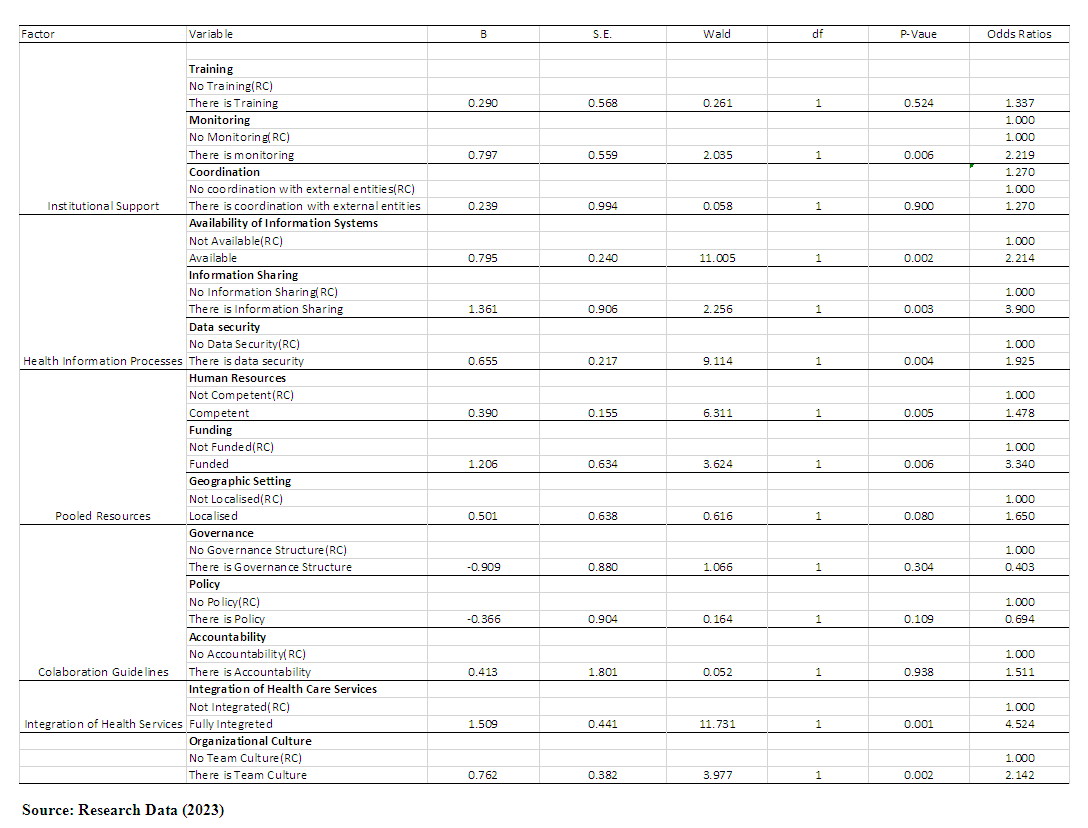
- Hypothesis TestingTo determine the drivers of a functional Integrated HIV/NCDS care model for a sustainable healthcare system in Nakuru county, five hypotheses were tested. The endogenous variable was healthcare system performance categorized as “sustainable” and “not sustainable”. This was achieved by consolidating all responses on healthcare system performance and sustainability test scores computed. The questionnaire had four items measuring the sustainability of HIV/AIDS and NCD services measured on a five-point Likert scale. Sustainability test scores ranging from 4 to 12 implied that HIV/AIDS and NCD services are not sustainable while scores above 12 implied that HIV/AIDS and NCD services are sustainable in Nakuru County. The initial tests were done using the chi-square test of significance. Chi-square is suitable when determining the existence of a relationship between two categorical variables. In this study, all the variables are categorical. The chi-square values were obtained by running cross-tabulations in SPSS version 24. Binary logistic regression was then used to determine the cause-and-effect relationship among the study variables. Binary Logistic regression is used to predict a dichotomous outcome variable. In this study, the outcome variable was dichotomous.Hypothesis 1Ho: Institutional support of HIV/NCD integrated services has no significant influence on Healthcare System Performance. This was achieved by cross-tabulating responses on institutional support of HIV/NCD integrated services and health system performance. Institutional support had three parameters namely, training, monitoring and coordination with external stakeholders. Healthcare systems performance was measured using its sustainability. Pearson’s chi-square results for training and performance of health systems were, χ2 = 0.125, n = 198, p = 0.835. For monitoring and performance of health systems, χ2 = 3.578, n = 198, p = 0.044 while for coordination with external entities and performance of health systems, χ2 = 0.480, n = 198, p = 0.652. This implies that only monitoring of integrated HIV and NCD services is associate with the performance of healthcare systems in Nakuru County. Hypothesis 2The study also sought to determine whether HIV/NCD integrated health information processes influence the performance of the healthcare system in Nakuru County. To guide the achievement of this objective, the following hypothesis was formulated. H0: HIV/NCD integrated health information processes have no significant influence on Healthcare System Performance. Information processes had three domains namely, Availability of information systems, data sharing methods, and information security. Health systems performance was assessed in terms of its sustainability. Each domain of availability of information systems was cross tabulated against the health system sustainability. For availability of information systems and performance of health systems, Pearson’s chi-square, χ2 = 9.955, n = 198, p = 0.001. For information sharing and performance of health systems, χ2 = 12.285, n = 198, p = 0.001 while for information security and performance of health systems, χ2 = 6.486, n = 198, p = 0.001. This implies that all the domains of information processes are significant predictors of healthcare systems performance. Hypothesis 3The study also aimed at establishing whether HIV/NCDs integrated pooled resources influences performance of healthcare system in Nakuru County. To guide the achievement of this objective, the following hypothesis was formulated and tested at 5% level of significance. Ho: There is no significant influence of HIV/NCDs integrated pooled resources on Healthcare System Performance. Pooled resources had three domains namely, human resources, funding models and geographic setting. Each domain was cross tabulated against the performance of health systems measured in terms of their sustainability. The results of the analysis were as follows: For human resources and performance of healthcare systems, Pearson’s chi-square, χ2 = 4.122, n = 198, p = 0.049. For funding models, χ2 = 12.203, n = 198, p = 0.001, while for geographic setting, χ2 = 4.122, n = 198, p = 0.049. These results indicate that human resources and funding models are significant predictors of health system performance in Nakuru County, but geographic setting is not associated with health system performance in Nakuru County. Hypothesis 4The study also aimed at establishing whether HIV/NCD integrated collaboration guidelines influence performance of healthcare system in Nakuru County. Integrated collaboration guidelines included governance structures, policy requirements and accountability. To guide the achievement of this objective, the following hypothesis was formulated and tested at 5% level of significance.Ho: HIV/NCD integrated collaboration guidelines significantly influence Healthcare System performance.The Pearson’s chi-square results were as follows; governance structure, χ2 = 0.783, n = 198, p = 0.271, Policy requirements, χ2 = 2.076, n = 198, p = 0.118, for accountability, χ2 = 0.503, n = 198, p = 0.742. These results imply that all the collaboration guidelines are not significantly associated with performance of healthcare system in Nakuru County. Hypothesis 5The study also aimed at establishing whether integration of HIV/NCD services and performance of healthcare system has significant influence on Health system performance. To guide the achievement of this objective, the following hypothesis was formulated and tested at 5% level of significance. Ho: The relationship between integration of HIV/NCD services and performance of healthcare system has no significant influence on Health system performance. The results of the analysis were as follows; Pearson’s chi-square, χ2 = 17.939, n = 198, p = 0.001. These results indicate that integration of healthcare services is associated with health system performance in Nakuru County. Multivariate AnalysisThis section presents the results of logistic regression analysis. Logistic regression was carried out to establish the cause-and-effect relationship that exist between the outcome variable and the predictors. The chi-square results earlier discussed only demonstrated whether a relationship exists between the endogenous and each explanatory variable. The chi-Square test was critical in evaluating the interdependence of the variables by establishing if an association between them exists. However, it did not show the cause-and-effect relationship existing between each predictor variable and the outcome variable. Consequently, binary logistic regression was done to establish the cause-and-effect relationship existing among the study variables. Logistic regression is applied when the endogenous variable is binary in nature. In this case, the endogenous variable was healthcare system performance measured in terms of its sustainability. The predictor variables are institutional support, health information processes, pooled resources, and collaboration guidelines. Organizational culture is the moderating variable. Logistic regression also facilitated in determining the influence of each explanatory variable on the endogenous variable. The results of the analysis are as follows.Relationship between integrated HIV/NCD services and performance of healthcare controlling for the effect of organizational culture.
|
|
|
 | Table 4. Multivariate logistic regression results without Moderator |
|
 | Table 6. Parameter Estimates with moderator |
4. Discussion and Conclusions
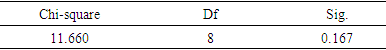
- This study unveils groundbreaking findings regarding the integration of HIV and NCD services. The significance of these findings extends beyond their novelty, as they have far-reaching implications for healthcare systems and patient care. Integrating HIV and NCD services is crucial in addressing the complex needs of individuals living with both conditions, as they often require comprehensive and coordinated care. By presenting these novel findings, this study contributes to the advancement of healthcare practices and policies, particularly in the context of HIV/NCD integration.The results of Pearson's chi-square tests indicate that only the monitoring of HIV/AIDS and non-communicable disease (NCD) services is significantly associated with the performance of health systems in Nakuru County. The lack of significant associations between training and coordination with external entities with health system performance suggests that these factors may not directly impact overall health system performance. The implication is that Nakuru County should prioritize strengthening monitoring mechanisms for HIV/AIDS and NCD services to improve health system performance. This includes implementing robust data collection, analysis, and feedback systems to identify gaps and areas for improvement. Additionally, while training and coordination efforts should not be disregarded, alternative strategies may need to be explored to enhance their effectiveness in translating into improved health system performance. Contrary to the suggestions put forth by Balzer et al., (2015), our research findings reveal that health workers in Nakuru County are already well-trained and benefit from ongoing training programs facilitated by external partners [14]. Consequently, the primary focus should be on monitoring progress to ensure the effective implementation of existing plans and prompt corrective actions when necessary. The viewpoint presented by Guezennec et al. (2016) further emphasizes the importance of regular assessments to identify successful strategies and areas requiring improvement [15].The study found that all the domains of information processes, including the availability of information systems, information sharing, and information security, were significant predictors of health system performance. The statistical analysis showed significant associations between these domains and health system performance, indicating their importance in determining the overall effectiveness of the health systems. These findings are in agreement with those of [10,16,17] who found that the availability of fully functional HIS, seamless flow of information in an integrated system, and the security of HIS are key drivers to success operation of healthcare organizations because they enable timely evidence-based decision making. These findings highlight the need to prioritize the development and implementation of robust information systems, promote effective information-sharing practices, and ensure adequate measures for information security within health systems. By addressing these domains, policymakers and stakeholders can work towards improving the performance and outcomes of health systems.The findings also indicate that the performance of the health system in Nakuru County is significantly influenced by human resources and funding models. The findings on skilled and adequate human resources as reported by [5,6] are quite important in improving performance of an organization, hence this finding is in agreement with the current finding of this study. Funding models and investments in health system as reported by [18]; [19] are also key drivers to access and utilization of healthcare services hence with proper financing arrangement that protect the patients from financial burden would enhance better sustainability of the health system. These results underscore the critical need to invest in and give priority to the recruitment, training, and retention of healthcare professionals. Additionally, it is crucial to establish sustainable funding mechanisms that can support the provision of high-quality healthcare services. It is also essential to take into account local factors and adapt interventions and strategies accordingly. By addressing these crucial factors, policymakers and stakeholders in Nakuru County can collaborate toward enhancing the overall performance and outcomes of their health systems.In contrast, the findings suggest that there is no significant association between the collaboration guidelines (governance structure, policy requirements, and accountability) and the performance of the healthcare system in Nakuru County. This indicates that other factors or variables may exert a stronger influence on the system's performance in this context. While collaboration guidelines may not directly impact performance, it is essential for policymakers and stakeholders to consider other factors that can contribute to enhancing the healthcare system's effectiveness. These factors may include human resources, funding models, information systems, and quality improvement initiatives. By prioritizing these areas, policymakers can strive to improve the overall performance and outcomes of the healthcare system in Nakuru County.Finally, the results indicate a significant association between the integration of healthcare services and the performance of the health system in Nakuru County. These finds are in agreement with those of [20,21,22] who introduced different models of integration. The first model acknowledges the complexity patterns and interrelationships in an integrated care model and regards healthcare as a complex adaptive system. Then a six-domain model is used in managing chronic care including the community, self-management support, health system clinical information system, and decision support. Then integrated chronic disease management guarantees a flawless evolution to assisted selfcare and improves the quality of care through an approach of embracing the health system building blocks that this study is advocating for. These findings are supported by previous researchers as highlighted. This means successful integration is driven by a phased approach of implementation for better performance and sustainability of the health system. These findings underscore the importance of promoting and investing in initiatives that facilitate the integration of healthcare services to enhance the overall quality, efficiency, and effectiveness of care delivery in the region.The results of the multivariate analysis demonstrate the significance of organizational culture in shaping the behavior and practices within the healthcare system. A culture that promotes collaboration, communication, and innovation fosters a positive work environment and facilitates effective teamwork among healthcare providers. This, in turn, can lead to improved coordination of care, streamlined processes, and better patient outcomes. The results of the analysis contradict the findings of [7] and [23], who emphasized the importance of institutions adhering to standard guidelines, regulations, and a conscious sense of their setting to achieve success and legitimacy. They emphasized the significance of institutions ensuring legitimacy through adherence to established guidelines, regulations, and a conscious understanding of their context. These factors contribute to the success and effectiveness of healthcare institutions. Given these contradictory findings, further research is needed to reconcile the differences and gain a comprehensive understanding of the relationship between healthcare service integration, adherence to guidelines, regulations, and overall health system performance. Future studies could explore the specific contextual factors that may influence the association between integration and success, as well as the potential interaction between adherence to guidelines and integration. The establishment of clear guidelines and policies play a crucial role in ensuring the effective management of both HIV and NCDs [24]. It is important for policymakers, healthcare administrators, and practitioners in Nakuru County, to consider both perspectives when formulating strategies and making decisions regarding healthcare service integration. This includes balancing the benefits of integration with the need to adhere to established guidelines and regulations to ensure legitimacy and optimize overall system performance. A nuanced approach that takes into account the unique context and characteristics of the healthcare system in Nakuru County will be crucial in achieving successful outcomes.The omnibus test of model coefficients, as indicated by the significant p-value (p<0.01), suggests that the model has a strong predictive ability when considering all the study variables as a block. This finding has important implications for the validity and reliability of the regression analysis. It indicates that the predictor variables included in the model have a significant relationship with the response variable, providing confidence in the model's ability to accurately predict and explain the outcomes of interest. Researchers and practitioners can have confidence in utilizing this model to make informed decisions and draw meaningful conclusions based on the relationships identified between the predictor and response variables. Moreover, in this study, the chi-square results from the Hosmer-Lemeshow test (χ2 = 11.660, p = 0.167) indicate that the null hypothesis, which suggests that the model is fit, cannot be rejected. This finding implies that the logistic regression model used in this study is appropriate and possesses significant predictive ability. The implications of this result are that the model can be relied upon for making predictions and drawing conclusions related to the study's objective. Researchers and practitioners can have confidence in the model's fit and use it as a valuable tool for understanding and predicting the binary outcomes of interest.Conversely, the results of the Nagelkerke pseudo-R-squared statistic, indicate that the five explanatory variables considered in the model account for approximately 36.9% of the variations in health system performance in Nakuru County. However, it is important to note that about 63.1% of the variation in healthcare performance remains unexplained by the variables included in this study. This finding highlights the need for further research in this area to identify and understand the additional factors that influence healthcare performance, especially as the country moves towards the implementation of universal healthcare. Conducting more comprehensive studies can provide deeper insights into the determinants of health system performance and guide policymakers in implementing effective strategies to improve healthcare outcomes. In conclusion, the integration of HIV and NCD care is crucial for providing comprehensive and efficient healthcare to individuals living with both conditions, as they often face complex health challenges and require coordinated and integrated care. By identifying the determinants of integration, this study provides insights that can inform policymakers, healthcare administrators, and practitioners in developing strategies and interventions to strengthen health systems and improve the integration of HIV and NCD services. This ultimately leads to better health outcomes and enhanced quality of care for individuals affected by HIV and NCDs. Policymakers, healthcare administrators, and practitioners can leverage these findings to develop evidence-based strategies and interventions that strengthen health systems, enhance service integration, and ultimately improve health outcomes for individuals affected by HIV and NCDs. The usefulness of our study lies in its ability to guide decision-making, resource allocation, and the implementation of integrated care models, thereby fostering more effective and patient-centered healthcare delivery. In summary, our study provides invaluable insights that have the potential to drive substantial improvements in the integration of HIV and NCD services, ultimately leading to enhanced quality of care and improved health outcomes for the affected population.
5. Recommendations
- On institutional support - the study recommends that the top management, middle level managers and mangers at the operational level need to enhance monitoring of outcomes which is crucial for Nakuru County to achieve better results in sustaining the integrated care models within a healthcare system. Institutions should leverage on already skillful trained healthcare workers by ensuring clarity in what is expected of them and ensuring that their performance measures are clear for easy monitoring. Success during planning leads to success in performance.Health Information Processes - Health Information managers should ensure enhancement and seamless flow of information processes. This would be best supported by electronic data processing tools. There is need to ensure they sustain centralized data source with tight security and privacy measures on the data and the information. Pooled Resources- The program leads, county management teams, hospital boards, facility in charges are the key drivers to ensuring human resources, information resources, financial resources through the funding models and physical resources within the health sector are shared, well utilized in every institution providing healthcare services for purposes of continuous care and sustainability of services provided.Collaborative guidelines were not found to significantly influence sustainability/ performance of the healthcare system; however, health workers should be in the fore front to creating awareness to all stakeholders of the provided governance structures and policies in place to facilitate access to care for patients with multiple conditions. Health facilities should support patients to access care from a single point this would enhance saving of time and cost. This would also improve the client’s experience. Health sector stakeholders should enhance a collaborative-team oriented organization culture approach to providing and receiving health care services.
Areas of Further Research
- Future research can look into specific NCD integration. This study generally looked at HIV/NCD services integration without being specific on the type of NCD.
Declarations
- Consent to publish.Not applicable.Conflict of InterestThe authors declare no conflict of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML