-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2022; 12(3): 69-77
doi:10.5923/j.phr.20221203.02
Received: May 6, 2022; Accepted: May 26, 2022; Published: Jun. 13, 2022

Spousal Communication in Decision Making During Pregnancy in Northern Ghana
James Dakura 1, Adadow Yidana 2, Robert Kuganab-Lem 3
1Department of Global and International Health, School of Public Health, University for Development Studies, Tamale, Ghana
2Department of Social and Behavioral Change, School of Public Health, University for Development Studies, Tamale, Ghana
3Institute of Research, Environment, Water, Health and Development, Tamale Technical University, Tamale, Ghana
Correspondence to: Adadow Yidana , Department of Social and Behavioral Change, School of Public Health, University for Development Studies, Tamale, Ghana.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Despite all the interventions put in place to improve maternal and child health, little has been done on spouses' communication during pregnancy and how it impacts maternal health decision-making. The study sought to unravel the influence of spousal communication when they are pregnant on maternal health decision-making. The study used a mixed-method approach involving 218 pregnant women, six midwives, and village health volunteers from three communities and three health facilities in the district, respectively were interviewed. In-depth interviews with the midwives and village health volunteers were selected purposively; interviews were conducted with pregnant women at the three health facilities selected using stratified sampling. From the study, 96.8% indicated that they often discuss issues concerning their health with their husbands, while only 3.2% did not. Again, 97.2% stated they often discuss their pregnancies with their husbands, while 2.3% did not, and 0.5% did not remember whether they did. From the study, issues such as quarrels, shyness, and husbands' jobs responsibility, making them have little time to communicate, were some of the barriers to spousal communication. About 64% scored high in male involvement in maternal health decision-making during the antenatal care period, while about 36% of males scored low in maternal health decision-making. Male involvement in maternal health decision-making was found to be influenced by age. Though some fathers communicate with their wives, the number is not encouraging. The District Health Management Team must take practical steps to encourage and support the formation of father-to-father support groups in the district, just as there is a mother to mother support group, and ensure that such groups are sustainable and functioning.
Keywords: Spouse, Decision-Making, Pregnancy, Communication
Cite this paper: James Dakura , Adadow Yidana , Robert Kuganab-Lem , Spousal Communication in Decision Making During Pregnancy in Northern Ghana, Public Health Research, Vol. 12 No. 3, 2022, pp. 69-77. doi: 10.5923/j.phr.20221203.02.
Article Outline
1. Background
- There is an estimated 200 million pregnancy in the world, every year. Pregnancy is а normal process that results in a series of both physiological and psychological changes in women. Pregnancy isn’t а disease; it is a normal, unique and powerful experience. [1,2].Healthy conversation between spouses during pregnancy is a central measure of maternal well-being and is often not noted with the aid of fitness programs in developing nations [3]. Although communication exists between spouses during pregnancy, it is not clear for partners who participate in contact even during pregnancy that parenthood is the greatest and most rewarding experience [4]. Constructive communication may lead to psychological well-being and protect against stressors, including worry during pregnancy. Research suggests that anxiety disorders constitute many health problems [5-9]. Men ought to have communicated and accompanied their wives to and from antenatal clinics [10].Several studies examined how spouses collectively contribute to each other's psychological and physical health [11]. The spouses ' health and well-being attitudes are usually the same and tend to meet per period [12]. This is partly due to assorted copulating: humans usually select a partner that is the same in outlook and characteristics, as well as fitness-related habits such as meals, physical exercise, smoking, liquor intake, and BMI [12].The Shared assets hypothesis suggests that agreement can be a purpose of the point that spouses pair a life habit and similar worries; partners usually will have existing joint surrounding, gather possessions, eat collectively, and share a common linkage [13]. Spouses' day-to-day activities are entangled, and each partner's traits, disposition, approaches, conduct, fitness, anxiety, and life habit affect each other. Thus, the shared control of couples can be favorable or harmful to fitness and well-being [13]. As enshrined in the third Sustainable Development Goals (SDGs), "Ensure healthy lives and promote well-being for all ages," refining healthiness status remains a worldwide and nationwide agenda. Factors that may result in a lack of male spouses' interest in maternal and child well-being include lapses in communication among researchers and policymakers, health practitioners, and the final consumers of the service delivery [14]. The conversation rate between spouses denotes communication in the marital dyad [15]. The mere existence of a significant other is not essentially protecting; worried matrimony is itself a primary basis of worry and, at the same time, limits the ability of a partner to strive for aid in extra connections [16]. A quality marriage beautifies one's complete sense of safety, and nuptial grief raises fitness risks [4,17]. The relationship between life gratification and nuptial excellence is resilient to the existence of fulfillment's relations to either one's work or fitness [18]. Different studies have been conducted on the spousal relationship during pregnancy, including male involvement in maternal health decision-making in Nkwanta South District [19]; factors influencing male participation in antenatal care in the Kumasi Metropolis [20]; analysis of maternal mortality in Wa [21]; men's involvement in care and support during pregnancy and childbirth in Gambia [3]; understanding couple communication and family planning in Zambia [22]. Of all these studies, none discussed spousal Communication during Pregnancy. The objective was to assess spousal Communication during Pregnancy and maternal health decision-making in the Nadowli-Kaleo District of the Upper West Region.
2. Methodology
2.1. Study Setting and Design
- The study took place in the Nadowli-Kaleo District, one of the eleven districts in the Upper West Region of Ghana. The study was a descriptive cross-sectional hospital-based. This approach was helpful because it utilizes qualitative and quantitative data [23]. The study participants comprised married women who were pregnant and living with their husbands, midwives, traditional birth attendants, and village health volunteers.
2.2. Inclusive and Exclusion Criteria
- The inclusion criteria include women who were pregnant and attending ANC at the hospitals and health centers, including health workers in the communities. The exclusion criteria include Pregnant but cohabitating women and pregnant women whose spouses were not within the study catchment area.
2.3. Sampling
- The sample size was determined using Cochran's formula;
 A stratified sampling technique was employed to classify the health facilities into strata, the two hospitals were considered stratum one, and the health centers were considered stratum two. Both hospitals in stratum one were considered in the study, while a simple random sampling technique was employed to select a health centre from stratum two, which contains ten (10) health centres. Participants who participated in the study in the three health facilities were selected using probability proportional to size sampling technique. A sample size of 385 pregnant women who were married in the target population was selected. Purposive sampling was employed to select six traditional birth attendants, village health volunteers, and midwives in any three communities and the three health facilities in the district, respectively.
A stratified sampling technique was employed to classify the health facilities into strata, the two hospitals were considered stratum one, and the health centers were considered stratum two. Both hospitals in stratum one were considered in the study, while a simple random sampling technique was employed to select a health centre from stratum two, which contains ten (10) health centres. Participants who participated in the study in the three health facilities were selected using probability proportional to size sampling technique. A sample size of 385 pregnant women who were married in the target population was selected. Purposive sampling was employed to select six traditional birth attendants, village health volunteers, and midwives in any three communities and the three health facilities in the district, respectively. 2.4. Pre-testing
- Questionnaire and interview guides were pre-tested at the Wa Regional sanatorium for precision, uniformity, and tolerability of questions to interviewees. The required adjustments were inputted, and the questionnaire was made ready for the actual fieldwork.
2.5. Data Collection Techniques and Tools
- The techniques for data collection were surveys and interviews. The data collection tools were structured questionnaires and interview guides for quantitative and qualitative data. The researcher used Dagaare (the primary local language spoken in the study area) and English in the data collection process.
2.6. Data Processing and Analysis
- The quantitative data were analyzed using Excel and the Statistical Package for Social Sciences (SPSS) version 25.0. The qualitative data were analyzed using content analysis by arranging them into themes identified in the discussion guide. Qualitative data were analyzed using a constant comparison content analysis methodology after defining common themes that would address research questions, based on field notes and transcripts from In-depth interviews [24].
2.7. Ethical Clearance
- Ethical clearance was obtained from Kwame Nkrumah University of Science and Technology Committee on Human Research, Publication and Ethics (CHRPE) Board with reference number CHRPE /AP/089/20 before data collection commenced. Before conducting the survey, approval to carry out the study was also obtained from the Department of Community Health and Family Medicine of the University for Development Studies. An introductory letter from Ghana Health Services (GHS) with reference number GHS/UWR/TP-51 was also sent to the study area for approval before administering questionnaires.
3. Results
3.1. Sociodemographic Characteristics of Respondents
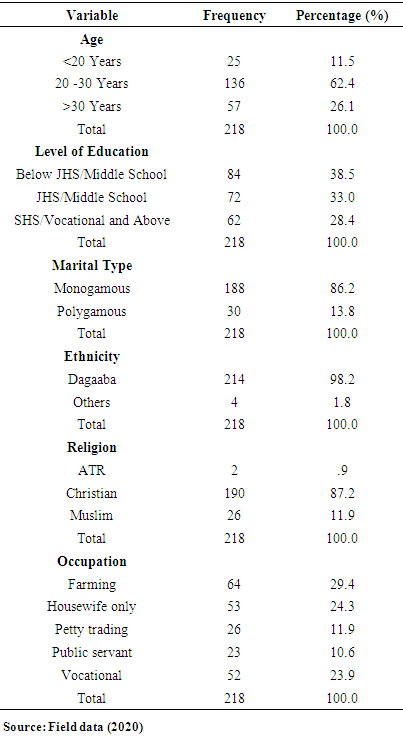
- From table 1, 62% of respondents were aged 20 to 30 years, 11.5% were less than 20 years, and 26.1% were above 30 years. Again, 38.5% of attained education below Junior High School or Middle school, 33.0% were in Junior High School (JHS) or Middle school, while 28.4% were in Senior High School (SHS) or Vocational and above. Also, 86% were found in a one-husband one-wife marriage, while the remaining 14% were in a polygamous marriage. Respondents were into various categories of Occupation, of which 29.4% were farmers, 24.3% were housewives only, 11.9% were petty traders, and 10.6% were public servants. On ethnic lines, 98.2% were Dagaaba, while the remaining were Kassenas, Akans, and others, constituting 1.8%. In terms of religion, 87.2% were Christians, 11.9% were Muslims, and 0.9% of them practiced African Traditional Religion.
|
3.2. Prevalence of Spousal Communication on Health During the Pregnancy
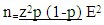
- Communication is a very important ingredient in every relationship or marriage. Figure 1 indicates whether respondents often discuss their health and pregnancy with their husbands during the period of gestation. The majority of respondents (96.8%) indicated that they often discuss issues concerning their health with their husbands, while only 3.2% did not. Again, most respondents (97.2%) stated that they often discuss their pregnancy with their husbands.
 | Figure 1. Prevalence of spousal Communication on health during the pregnancy period (Source: Field data (2020)) |
3.3. Issues Couples Often Discuss Other than Health Matters
- In-Depth Interview were held at health facilities and communities; some participants expressed their views on issues couples often discuss other than health. A midwife opined that; "They concentrate more on how to care for the woman in terms of getting logistics, finances, and the money to cater for the woman instead of talking about their health."-----A midwife with five years' experience.
3.4. Barriers to Spousal Communication on Health During Pregnancy
- Regarding what prevents them from having a conversation with their husbands during pregnancy, they indicated that; "Because of my husband's kind of work (mason work), he does not have time for me to have a serious conversation with him. He normally comes late, and he is tired. Also, he is not the talkative type" [smiling]. (Pregnant woman 1) Another respondent indicated that;"You don't know my husband. Anytime I complain about my health or pregnancy, he will say I am lazy, and he does not like me to talk about anything that has to do with money. Talk to him, and he is inside the room. Should I call him"? (Pregnant woman 2)Generally, village health workers/volunteer midwives and Traditional Birth Attendants recruited for In-Depth Interviews believed that there exists inadequate spousal communication during pregnancy, contrary to results from pregnant women. It is often not clear to health care providers the barriers to spousal communication during pregnancy; "I cannot tell whether cultural or religious beliefs affect spousal Communication during Pregnancy, but I believe there are none. Lack of spousal Communication can lead to inferior psychosis, so communication is necessary during pregnancy. If the communication is well established during pregnancy, I think everything will be okay. The husband will be able to provide everything the woman needs, and there will be nothing hidden. We know that what the mother gets during pregnancy (nutrients) is what the baby gets (nutrients). If there is proper communication and the husband can take care of the woman well, it will translate into a healthy baby". (ANC In-charge with over ten years' experience).
3.5. Male Involvement in Maternal Health Decision Making During ANC
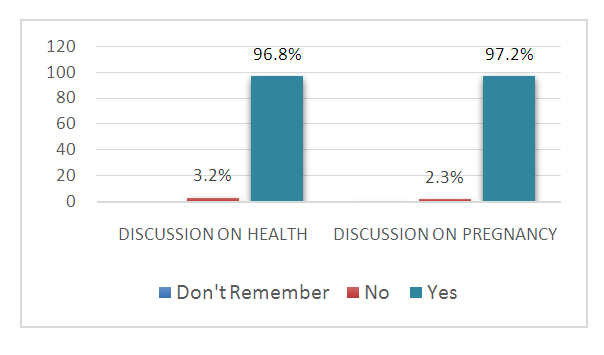
- Males are expected to be involved in decision-making concerning matters related to maternal healthcare. Male involvement improves women's access to healthcare during pregnancy. Figure 2 explains males' involvement in women's Antenatal care (ANC). A higher majority of males (83.9%) did encourage or ask their spouses to attend ANC. However, most males (67.0%) never attended ANC with their spouses. Again, 59.2% support their spouses with transportation to ANC, while 40.8% never did.
 | Figure 2. Male involvement in maternal health decision making during ANC periods (Source: field data (2020)) |
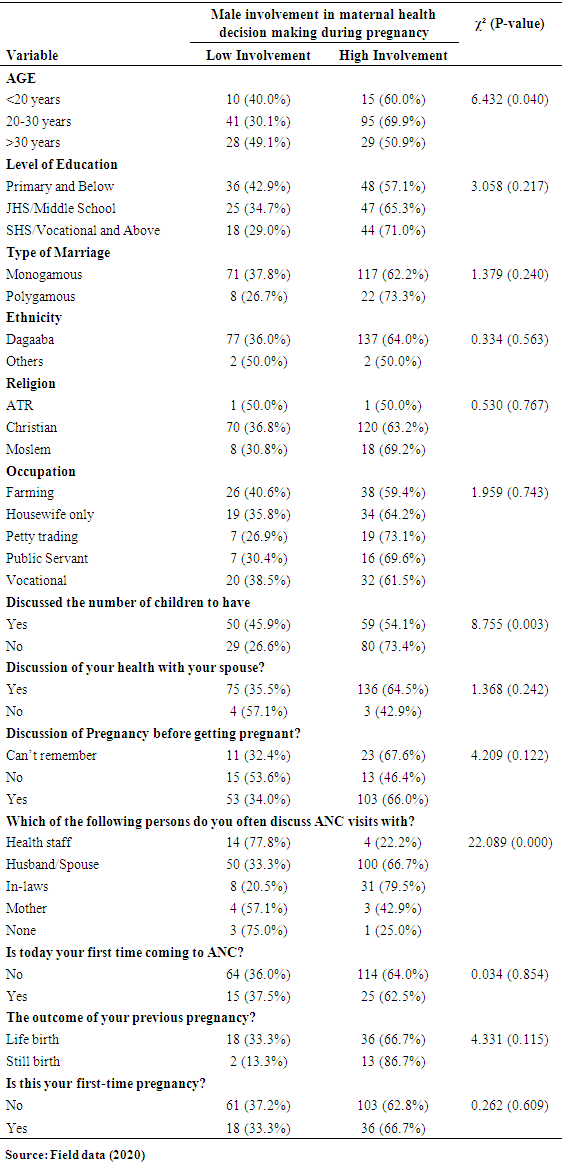
3.6. Factors Influencing Male Involvement in Maternal Health Decision Making During Pregnancy
- In this study, a bivariate analysis was employed using cross-tabulations in the SPSS version 25.0 program. Factors such as sociodemographic characteristics, spousal communications, and health characteristics were measured and analyzed to see how they impact male involvement in motherly fitness choice-making during ANC periods. Each independent variable was cross-tabulated with the dependent variable (i.e. level of males involvement in maternal health decision making during the ANC period) to investigate the association between the two variables. The χ² value tested the power of the association. The statistical significance of χ² was tested by the P-value of 0.05 as a criterion.
3.7. Age and Level of Male Involvement in Maternal Health Decision Making
- As illustrated in table 2, two variables showed a strong (χ²=6.432) and a statistically significant relationship (p-value = 0.040). Women in the age group of 20-30 were more likely to have their spouses involved in maternal health decision-making during the ANC period than other women in the age group <20 years and age group >30 years.
3.8. Number of Children to Have and the Level of Male Involvement in Maternal Health Decision Making
- It can be seen from table 2b that there is a strong (χ²=8.755) and significant (p=<0.003) association between whether or not respondents discussed with a spouse the number of children to have and the level of male involvement in motherly fitness choice-making during ANC period.
3.9. Discussion of ANC Visit with Spouse and Level of Male Involvement in Maternal Health Decision Making
- The results show strong evidence (χ²=22.089) of a relationship between the two variables. Respondents who discussed their ANC visits with their spouses and their in-laws were more likely to score high in their male counterparts' involvement in motherly fitness decision-making during ANC. Compared to those who discussed with Health staff and their mothers, none with a statistically significant p-value of 0.000. As recorded in Table 2, the rest of the measured variables did not show significant relationships with males' taking part in motherly fitness choices during the ANC period.
|
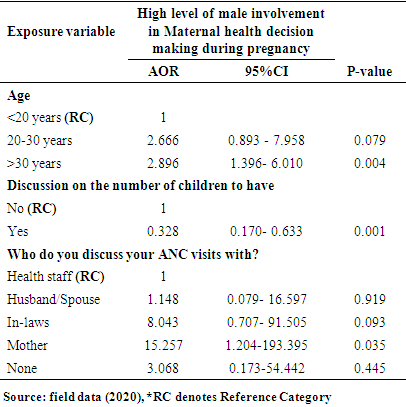
3.10. Logistic Regression Analysis
- The Logistic regression analysis was done where all the independent variables were matched against the dependent variable using Binary Logistic Regression. Those independent variables which have shown statistically significant relationships with the dependent variable in the bivariate analysis were included in the multivariate model.Results from table 3 show a NagelkerkeR-square value of 0.221, which means that 22.1% of the variation in male involvement in maternal health decision-making during antenatal periods is explained by the factors in the model, while other factors explain 77.9%. The results showed a significant relationship between the respondent's age, whether they discuss how many children to have with a spouse, who respondents discuss ANC visits with, and their male counterparts' level of involvement in maternal health decision making during the ANC. The odds of respondents in the aged >30 years group whose spouses have a high level of participation in maternal health decision making during the ANC is almost three times the odds of belonging to the <20 years group [(AOR: 2.896, 95% CI: 1.396-6.010, p=0.004)]. The odds of respondents who discussed with their spouses the number of children to have, whose spouses have a high level of involvement in maternal health decision making during antenatal is less than half times the odds of respondents who did not discuss the number of kids to have with their spouses [(AOR: 0.328, 95% CI: 0.170-0.633, p=0.001)]. Again, the odds of respondents who discussed their ANC visits with their mothers, whose spouses have a high level of involvement in maternal health decision making during ANC is about fifteen times the odds of belonging to respondent groups who discussed their ANC visits with a health staff [(AOR: 15.257, 95% CI: 1.204-193.395, p=0.035)].
|
4. Discussion
- There is a high-level prevalence of spouses communicating about their health and pregnancies. However, others do not remember holding any discussion during pregnancy, which should be a cause of worry. The results support the claim that inter-spouse conversation is occasionally considered an indicator of safe family planning activity, where pairs practice contraceptives usage correctly and regularly without suffering any side effects, thereby improving their health [25]. A conversation between spouses is a central step toward growing men's contribution to family planning and procreative health [26]. Similarly, in a study, a significant percentage of respondents had discussed their health with their husbands, but whether discussing translated into the husbands being involved in the decision-making process is an issue [27]. As indicated by [28], spousal communication can self-reliantly envisage the joy of marriage and a higher marital gratification, including being healthy. The study found out that the most communicated issue by spouses during pregnancy is farm activities, followed by several other issues, including financial issues, play, and household provisions. Others reportedly did not discuss anything concerning their well-being during pregnancy, which is detrimental to the male spouses taking part in the decision-making process regarding the pregnant spouses' health. Confirming this, two village health volunteers indicated; "They concentrate more on caring for the woman, getting logistics, finances, and getting the money to cater for the woman instead of talking about their health." (Female village health volunteer). "Men always communicate more on foodstuffs, and most of them concentrate on their work, and after they come back from farms they are only interested in what to eat, and after having eaten they are outside again with their male colleagues, drinking, sometimes too the husband and wife might not even engage in any discussion during pregnancy just because of little quarrel." (Male village health volunteer). Thus, emphasis is on how to feed the pregnant spouse, while little attention is on the decisions that could influence her pregnancy outcomes. The study found that female spouses tend to confer with friends in situations of little communication, thereby limiting male spouses' knowledge of maternal health, corroborating [29] similar findings. The implication is that once there is no communication on health during pregnancy, little or even no decision will be reached by spouses even though most pregnant women tend to obey their husbands, as espoused by [30] that just 2.7% of the decision to pursue health care comes from husband and wife. The remaining 97.3% is a mixture of characteristics present in the family. Health workers believed that there is inadequate spousal communication during pregnancy, contrary to respondents' claim. Respondents were usually not properly prepared for delivery, which could be attributed to inadequate spousal communication. The data reveals male spouses' fear of financial obligation, which corroborates [31], where men complain of mood swings and the high cost of escorting their pregnant wives to seek maternity care. Barriers to spousal communication also corroborate [32], which suggests that obstacles that prevent men from partaking in motherly well-being include the low level of knowhow, societal disgrace, being shy and embarrassed, task obligation, area hassle, non-couple pleasant maternal health offerings, and hospital coverage restrictions. Again, [20] study reported cultural causes as hindrances to male participation in maternal well-being. In that study, men saw maternal health issues as women's responsibility. The men understood that their only manly duty was to provide money to pay off any debt that might arise and make sure a male relation from either their family or partner's family escorted their wives or partners to the fitness facility.In settings where couples' communication is limited and male dominance is manifested, male involvement in reproductive health becomes challenging [33,34]. However, in the current assessment, the level of male spouses in motherly fitness choice-making during the ANC was high. Although the study revealed a higher involvement of male spouses in maternal health decision-making, it recorded a low level of men accompanying their wives to ANC clinics, which was revealed as a result of inadequate communication between spouses.On the contrary, male involvement in procreative fitness is daunting in nations where customarily distinct male-female roles hinder males from participating in Sexual and Reproductive Health [27]. Likewise, a study in Zambia by [22], proposed that intra-spousal conversation among couples was not rare or not even practical. Surprisingly, another study revealed that only 2.7% of the decision to seek health care comes from husband and wife, and the rest 97.3% is a combination of personalities found in the family [30,35,36]. However, in [37], he realized a changing trend in attitudes towards traditional norms. Even though there has been an absence of males in history, womenfolk are now becoming more voiced about needing backing in pregnancy and childbirth from their significant others, which supported what was found in this study since there was no cultural hindrance to male involvement in maternal health decision making. A number of factors such as the age of spouses, discussion with a partner, discussion ANC visits with mothers, spouses' level of education, and fear of the sight of blood and newborn were found to be associated with male involvement in maternal health decision-making during pregnancy. Interestingly, other studies did not find sociodemographic characteristics to influence male involvement in maternal health decision-making [19]. Again, [38] argued that negative conversations between couples and gender inequality constrain women's access to care services. This assertion corroborates results from this study's qualitative data in that once there was communication between the husband and pregnant wife, she would access ANC on time, and other health issues were discussed and noted. However, the study did not identify any cultural factors affecting spousal Communication during Pregnancy, but rather shyness and sheer ignorance on the part of spouses contributing to a lack of Communication during Pregnancy were classified as barriers. And this shyness in Communication about Pregnancy by spouses corroborated what was revealed by [3].
5. Conclusions
- Most respondents discussed their health and pregnancy with their husbands during the antenatal period. Aside from spouses' health, the other most discussed issue among spouses was their farm work. Couples also discussed household provisions, romance, and finances. However, a significant proportion of the respondents were found not to communicate on any issues pertaining to their lives. Barriers to spousal communication were generally due to quarrels, the nature of husbands' jobs making them have little time to communicate, mood swings among pregnant women, and husbands' fear of financial commitment. More than half of the respondents scored high concerning their male counterparts' involvement in maternal health decision-making during the ANC period. However, male spouses accompanying their female spouses to seek health care were still thriving.
Declaration
- Ethical approval: Ethical approval was obtained from Kwame Nkrumah University of Science and Technology Committee on Human Research, Publication and Ethics (CHRPE) Board with reference number CHRPE /AP/089/20.Consent for publication: All authors have consented to the submission and possible publication.Availability of data: Data is available on request.Competing of interest: There is no competing interest. Source of funding: The study was self-financed.
ACKNOWLEDGEMENTS
- We acknowledged the role played by the participants in this study area. We also acknowledged the contribution of the healthcare staff who helped us in the study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML