-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2022; 12(1): 8-13
doi:10.5923/j.phr.20221201.02
Received: Feb. 16, 2022; Accepted: Mar. 2, 2022; Published: Mar. 15, 2022

Non-Pharmaceutical Interventions against COVID-19 Pandemic: The Knowledge of Some University Students of Human Kinetics and Health Education
Adedamola Olutoyin Onyeaso 1, Favour I. Olusanya 2, B. Pharm 2, Chukwudi Ochi Onyeaso 3
1Department of Human Kinetics and Health Education, University of Port Harcourt, Port Harcourt, Rivers State, Nigeria
2Plot 163 Toiva Street, Behind Shining Star, Opposite Lodestar Academy, Kubwa Abuja, Nigeria
3Faculty of Dentistry, College of Health Sciences / University of Port Harcourt Teaching Hospital, University of Port Harcourt, Port Harcourt, Rivers State, Nigeria
Correspondence to: Adedamola Olutoyin Onyeaso , Department of Human Kinetics and Health Education, University of Port Harcourt, Port Harcourt, Rivers State, Nigeria.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction: Non-Pharmaceutical Interventions (NPIs) have been found to be very useful in containing the spread of COVID-19 Pandemic since 2020. The knowledge of them is crucial for those involved in health education and promotion in any community, especially in poor income settings like Nigeria. This study aimed at assessing the knowledge of these interventions in a group of University students in Nigeria. Materials and Methods: A self-administered questionnaire was carried out with 202 participants, whose age ranged from 18 to 32 years, with a mean age of 22.09 years, the majority of which 68.3% were women. The data was tested using descriptive, paired samples t-test with the significance level set at P < .05. Results: Of all the NPIs surveyed, the least they knew about was wearing of face mask (70.2%), followed by staying at home as much as possible (89.6%), while they scored over 90% in the rest. The participants significantly had good knowledge of the NPIs against COVID-19 Pandemic (P <.000) and the females significantly showed better knowledge than the males (P < .000). Conclusion: The participants had good knowledge of NPIs with the female gender was associated with better knowledge. More related studies indicated for better understanding of gender association with NPIs against COVID-19 pandemic.
Keywords: COVID-19 Pandemic, Non-Pharmaceutical Interventions, Gender, University students, Nigeria
Cite this paper: Adedamola Olutoyin Onyeaso , Favour I. Olusanya , B. Pharm , Chukwudi Ochi Onyeaso , Non-Pharmaceutical Interventions against COVID-19 Pandemic: The Knowledge of Some University Students of Human Kinetics and Health Education, Public Health Research, Vol. 12 No. 1, 2022, pp. 8-13. doi: 10.5923/j.phr.20221201.02.
Article Outline
1. Introduction
- Non-pharmaceutical interventions (NPI) are actions that people and communities can take to help slowing down the spread of viruses such as SARS-CoV-2. Such community mitigation strategies, ranging from individual actions such as regularly practising good hand hygiene to more restrictive measures like limiting size of gatherings should ideally be implemented in combination and applied at the same time. [1] The mix of chosen NPI should differ based on the local transmission situation. [1] It can take several weeks before any implemented NPI can show an effect. [1] According to European Centre for Disease and Control (ECDC), [1] what everyone of can do include physical distancing, strict hand hygiene, respiratory etiquette, appropriate use of face masks, in areas where physical distancing is not possible, and stay at home if you have COVID-19 compatible symptoms. The possible actions to take when is there is community spread are to stay at home if you had direct contact with a COVID-19 case; ideally, meet with the same people, whether family friends or limit the size of gatherings, eventually close selected. Others are work from home where possible, regular cleansing of frequently touched surfaces and objects, as well as ensuring appropriate ventilation of indoor spaces. Yang et al [2] reported that COVID-19 had infected over 68 million people globally. In their age-specific susceptible-exposed-infected-recovery-death model study that considered the unique characteristics of COVID-19 to examine the effectiveness of various non-pharmaceutical interventions (NPIs) in New York City (NYC), the control policies implemented showed reduction of infections by 72% and the number of deceased cases by 76% at the end of 2020. According their report, among all the NPIs, social distancing for the entire population and protection for the elderly in public facilities was the most effective control measure in reducing severe infections and deceased cases. In a related study [3] that focused on optimal control of COVID-19 with the help of NPIs, the results gave the major NPIs as stay home, sanitizer (wash hands), early case detection (PCR Test) and face mask. According to the report [3] these NPIs would help in mitigation and reducing the size of outbreak of the disease. Other similar reports [4-6] have also affirmed the usefulness of NPIs in the control of the spread of COVID-19 pandemic. In their review of literature published during the first eight months after the first cases of COVID-19 were confirmed and reported in Wuhan, China, Sharifi and Khavarian-Garmsir [7] showed that, in terms of thematic focus, early research on the impacts of COVID-19 on cities was mainly related to four major themes, namely, environmental quality, socio-economic impacts, management and governance, and transportation and urban design. Despite the importance of NPIs known and practiced globally, there is the known challenge of some of these NPIs in the economy, which could also be as serious as the spread of the infection. Chowdhury et al [8] in their multivariate prediction modelling study opined that efficient implementation of dynamic suppression interventions confers a pragmatic option to prevent critical care overload and deaths, gain time to develop preventive and clinical measures, and reduce economic hardship globally. The varied contributions of other authors with their useful recommendations have further affirmed the global importance of NPIs. [9-27] Considering the importance of these NPIs and the need for aggressive public health education globally, and much more importantly in poor economies like Nigeria, coupled with some perceived sceptism and fake news available in the social media and general population about COVID-19 pandemic, this study was conducted to assess the knowledge of some students of Human Kinetics and Health Education in a Nigerian University about NPIs. Undergraduate students of Human Kinetics and Health Education are expected to form part of the public health education /promotion group in any population and possibly be an important part of any ‘Public Health Education/Promotion Club’ in any tertiary institution or community. Therefore, it becomes imperative that they must be knowledgeable enough to help the rest of the student population and beyond through community education.
2. Materials and Method
2.1. Study Design
- A questionnaire-based cross-sectional study was used.
2.2. Study Population
- A convenience sample was drawn among the undergraduate students of Department of Human Kinetics and Health Education in the Faculty of Education of the University of Port Harcourt, Rivers State, Nigeria. Students in this Department are drawn from the different states in Federal Republic of Nigeria. Being a Federal University, the criteria for admission of the students makes the population in the Department fairly representative of the youths in the country.As part of a bigger study carried out in March 2021 after the general COVID-19 lockdown in Nigeria, this paper addresses the knowledge of non pharmaceutical preventive measures against COVID-19 Pandemic. Out of 223 self-administered questionnaire distributed to the students, 202 properly completed theirs and were included in the final study population of 64(31.7%) males and 138(68.3%) females with mean age of 22.09 ± 2.42 (SD) years and age range of 18 to 32 years.The following null hypotheses were generated and tested:Ho1: The knowledge of non-pharmaceutical preventive measures against COVID-19 pandemic by the participants would not be statistically significant.Ho2: There would be no significant gender difference in their knowledge of non-pharmaceutical preventive measures against COVID-19 Pandemic.
2.3. Correct and Incorrect Responses of the Participants
- The responses of the participants were categorized into ‘correct’ and ‘incorrect’ responses based on whether they ticked the correct answer or the incorrect option. The correct responses were weighted 2 while the incorrect responses had 1 for purposes of further statistical analyses.
2.4. Data Analysis
- The Statistical Package for Social Sciences (SPSS) was used to analyse the data. Both descriptive statistics and paired samples t- tests were used to analyse and test the hypotheses, while the significance level was set at P<0.05.
2.5. Ethical Approval and Participants Consent for the Study
- In line with earlier explanations [28,29], approval from the University was not considered necessary because the survey was very relevant to the curriculum of study of the participants. In addition, this survey is completely non-invasive.
3. Results
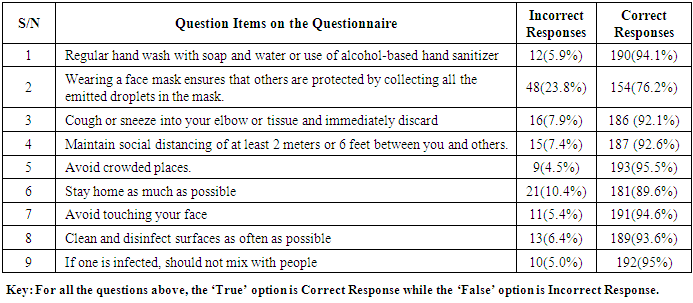
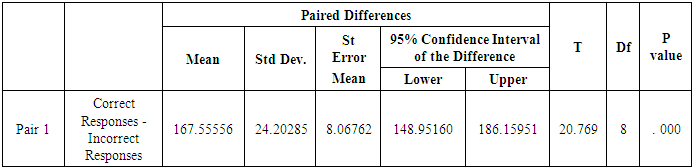
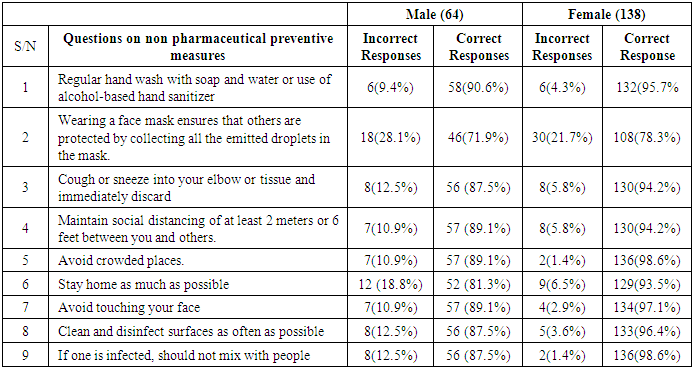
- Avoidance of crowded places was known by 95.5% of the participants, followed by 95% for infected people to isolate or stay at home and avoid mixing with other people. The least was wearing of face mask that accounted for 76.2%. Table below gives the details.
|
|
|
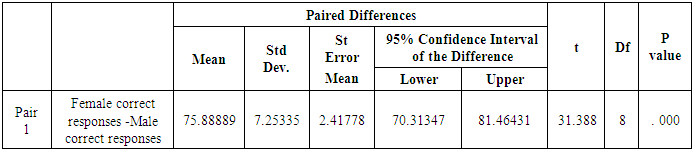
|
4. Discussion
- This Nigerian study has shown that significantly more of the participants were knowledgeable about non pharmaceutical preventive measures against COVID-19 Pandemic with the females significantly having better knowledge than the their male counterparts.Non-pharmaceutical interventions (NPI) are public health measures that aim to prevent and/or control SARS-CoV-2 transmission in the community. After vaccination, NPIs are the most effective public health interventions against COVID-19 [1]. Until a safe and effective vaccine is available to all those at risk of severe COVID-19 disease, NPI will continue to be the main public health tool against SARS-CoV-2 [1]. This is the situation in Nigeria because outside the skeptism that many Nigerians hold about the COVID-19 disease and the reports associated with the vaccines, the vaccines are still in short supply. In this Nigerian report, only 76.2% of the participants got it right. Although this study did not inquire of those who are observing these preventive interventions, this could be reflection of their belief in this known protective measure in control of the spread of this disease because watching and monitoring students and staff and members of the public here in Port Harcourt, Rivers State, Nigeria would confirm the fact that many people in the community are not keeping to this preventive measure. Kantor et al [30], in their study, reported that their respondents were most uncertain regarding the efficacy of mask and eye protection use, with 30.6 and 22.1%, respectively, unsure whether their use would slow disease spread. In a systematic review and meta-analysis carried out by Lezadi et al [31] showed that the majority of non-pharmaceutical public health interventions (NPHIs) had positive effects on restraining the COVID-19 spread. They stated further that with the problems that remain regarding universal access to vaccines and their effectiveness and considering the drastic impact of the nationwide lockdown and other harsh restrictions on the economy and people’s life, such interventions should be mitigated by adopting other NPHIs such as mass mask-wearing, patient/suspected case isolation strategies, and contact tracing.According to Lezadi et al [31], despite available evidence regarding the effectiveness of NPHs, there is still no consensus about how policymakers can trust these results as on the one hand, devastating consequences of NPHIs and on the other hand, the success of the NPHIs in combating and preventing COVID-19-related hospitalization and death. In Nigeria, with the poor state of the hospitals to accommodate hospital admission cases, it should be said that the activation of most the NPHIs did help in controlling the spread of the pandemic so far. However, it has not been without the negative impacts of these NPHIs on the economy and general standard of living of the people. Italy was in a severe epidemic status and the control measures were not sufficiently timely and effective in the beginning [32]. They added that non-pharmaceutical interventions, including contact restrictions and improvement of case recognition, play an important role in containing the COVID-19 epidemic. Following a fractional-order derivative approach, Ullah et al [33] reported that driven by extensive theoretical analysis and numerical simulation, their work further has illuminated the substantial impact of various control measures. The finding of staying at home being next to the use of face masks as the interventions with less than 90% could be explained by the fact that people find it very difficult to stay back at home as a means controlling the COVID-19 Pandemic According to European Centre for Disease Prevention and Control (ECDC), stay-at-home measures are a last-resort option due to their significant impact on both society and individuals. Targeted implementation, both geographically and temporally, is preferred and can be considered to control outbreaks which are not responding to other measures [1]. Available evidence does not prove that stay-at-home measures are more effective than other measures, such as the closing of (some) high-risk businesses [1].The current finding in this study of female participants having significantly superior knowledge of these non-pharmaceutical preventive measures compared to the males is an interesting one. Although this is analysed with caution, but it is noteworthy that reports [34,35] have shown that women make up 70% of the global health workforce and are highly represented on the front lines. They have been reported to be at high risk of frequent exposure to patients with high viral loads of COVID-19 infection [34,35]. Recent data show that, of the total healthcare workers infected with COVID-19 in Spain and Italy, 72% and 66% respectively were women [36]. There is no doubt that it will be of good public health if females have adequate knowledge of these NPIs. According to World Health Organization [37], equitable access to relevant training on infection prevention and control measures, personal protective equipment (PPE), essential products for hygiene and sanitation, and psychosocial support are critical for keeping health and social workers and their patients safe and healthy. It was further stated that these elements should take account of the specific needs of women, including differences in design and size of PPE which may compromise the protective benefit for women [37]. In fact, there is limited availability of sex and age disaggregated data, thus hampering analysis of gendered implications of COVID-19 and the development of appropriate responses [37]. Strengths and Limitations of the StudyThe study population is a fair representation of the youths from different parts of the country occasioned by the Admission Criteria being used for admission of students into Federal Government Universities in Nigeria, which ensures that admission of Nigerians from every state in Nigeria into the Federal Universities. This has made our sample to have appreciable representation of Nigerian youths. Even the gender proportion in this study could be seen as a good reflection of what obtains in the Nigerian society. However, the generalization of the results of this study should still be done with caution because of the sample size compared to the entire population of the country.
5. Conclusions
- 1. The study has revealed that the participants were significantly very knowledge about the non-pharmaceutical intervention (NPIs) against COVID-19 Pandemic with scores of over 90% in all of them except in wearing of face masks and staying at home as much as possible where they had less than 90% but over 70%.2. There was a significant gender association with their knowledge of these important non-pharmaceutical interventions against COVID-19 Pandemic with the females having significant superior knowledge than the males.
6. Recommendations
- It will be worthwhile to have more related studies with larger sample sizes, especially involving further exploration of any possible gender associations with NPIs against COVID-19 Pandemic.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML