-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2022; 12(1): 1-7
doi:10.5923/j.phr.20221201.01
Received: Jan. 20, 2022; Accepted: Feb. 8, 2022; Published: Feb. 24, 2022

Perceived Psychological Distress about COVID-19 Pandemic among University Students in Uyo, South- South Nigeria
Henry E. Jombo 1, Victory E. Iyanam 2, Alphonsus U. Idung 2
1Department of Psychiatry, University of Uyo, Uyo, Akwa Ibom State, Nigeria
2Department of Family Medicine, University of Uyo, Akwa Ibom State, Nigeria
Correspondence to: Henry E. Jombo , Department of Psychiatry, University of Uyo, Uyo, Akwa Ibom State, Nigeria.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The spread of COVID-19 disease on a global scale has posed a serious public health challenge worldwide. The psychological impacts of COVID-19 on mental wellbeing on university students are still being investigated. Studies that report the mental health risks of COVID-19 on university students are scarce. This study was conducted using an online self-administered questionnaire, perceived stress scale (PSS) to assesses the level of psychological distress and associated factors among university students in South-South Nigeria during the COVID-19 pandemic. The mean age of respondents was 21.5 years SD 5.4 consisting of 40.1% males and 59.9% females. The prevalence of psychological distress was 63.6%. High psychological distress was related to proximity to COVID-19 cases, exposure to suspected or confirmed cases of COVID-19 (p<0.001), female gender (p<0.001), being married (p=0.001), experience of COVID-19 related financial hardship (p<0.001) and having underlying medical conditions (p<0.001).
Keywords: COVID-19 Pandemic, Psychological distress, University students, Nigeria
Cite this paper: Henry E. Jombo , Victory E. Iyanam , Alphonsus U. Idung , Perceived Psychological Distress about COVID-19 Pandemic among University Students in Uyo, South- South Nigeria, Public Health Research, Vol. 12 No. 1, 2022, pp. 1-7. doi: 10.5923/j.phr.20221201.01.
Article Outline
1. Introduction
- The COVID-19 disease started in Wuhan, China in December, 2019 and has spread rapidly to all regions, cultures and countries worldwide and was declared a pandemic by the World Health Organization (WHO) on the 11th of March 2020 [1,2].COVID-19 infective agent is an RNA virus belonging to the Orthocoronavirinae family, which also includes other causal agents of pandemics such as Middle East respiratory syndrome (MERS-CoV) and severe acute respiratory syndrome (SARS-CoV). [3]. The infectious agent spreads rapidly by the respiratory route or contact with secretions. Its main symptoms are nasal congestion, a continuous cough, dyspnoea, fever, tiredness and occasionally, diarrhoea and central nervous system disturbances and could also be asymptomatic [4]. Human-to-human transmission has become the principal route of spread leading to a high number of cases of the disease worldwide. This has posed a serious public health challenge because in many countries, weak and inadequate healthcare systems and lack of economic resources add to the difficulty in containing the spread and management COVID-19 diseases [4-6].Containment measures such as social distancing, isolation of cases, closure of schools and businesses, traffic restriction, hand washing with alcohol based sanitizers and use of facial masks and are among the most adopted strategies in different cultures and countries [7-8].Recent studies have reported association between COVID-19 disease and increased vulnerability to psychological distress, sadness, anxiety and depression. Also, Studies from have reported association between persons in quarantine and the likelihood of psychological distress and increased vulnerability to sadness, anxiety and other symptoms of psychological distress [9-11].University students may be a vulnerable group for psychological distress because of stresses commonly associated with transitions to adulthood [12-13]. The impact of quarantine, social isolation, financial strain, the threat of infection and prolonged school lockdown, socio-demographic peculiarities may constitute risk for increased psychological distress among university students [10,11].Since the beginning of the COVID-19 pandemic, most of the global containment efforts have been directed at limiting its spread within the communities. However, much less attention is paid to the psychological consequences of the COVID-19 pandemic. This study aims to determine the psychological stress level and associated factors in a university community.
2. Materials and Methods
2.1. Procedure
- Ethical approval for this study was obtained from the University of Uyo Research and Ethics Committee. This was a cross-sectional study of University of Uyo students which was conducted in September 2020 using an Internet-based self-administered questionnaires. The participants in this study were recruited through social media (WhatsApp). The students who indicated willingness to participate in the study could open a link to get information about the study and give consent to proceed in participation. Eligibility criteria included being 18 years of age, residency in Nigeria and being a student of the University of Uyo.
2.2. Measures
2.2.1. Structured Socio-Demographic Questionnaire
- A socio-demographic questionnaire designed by the authors was used to obtain demographic information. Measures evaluated included socio-demographic details (age of the patient and family member, gender, educational status, marital status, religion, monthly family income, place of residence, history of contact with covid-19 cases). Participants were asked to indicate sources of distress from a check list of sources of distress during the COVID-19 pandemic.
2.2.2. Perceived Stress Scale
- The psychological distress of the respondents was measured using the 10 item perceived stress questionnaire [14]. Perceived stress scale (PSS) has been widely used by researchers in many cultures as a screening tool to determine whether an individual is at risk of developing a psychiatric disorder. It has been found to be reliable and well-validated in many cultures in industrialized and developing countries. It consists of 10 items, each one assessing the severity of a mental distress over the past few weeks. Each item is accompanied by five responses, typically being ‘never’, ‘almost never’, ‘sometimes’ and ‘fairly often’ and ‘very often’. Each item was scored using a 4-point Likert-type scale (from 0 to 4) to generate a total score ranging from 0 to 40. The positive items were scored from 0 to 4 and the negative ones from 4 to 0. The severity of psychological distress was categorized as: 0-13 (low stress), 14-26 (moderate stress) and 27-40 (high stress). Higher scores represented higher psychological distress. This instrument has been used in previous Nigerian study [15].
2.2.3. COVID-19 Exposure
- Exposure to COVID-19 was assessed by several nominal questions requiring yes/no answer. They were asked whether they had been exposed to suspected or confirmed COVID-19 cases in the past one month.
2.2.4. Social Support
- This was measured by Oslo 3-item social support scale. Respondents who scored 3–8, 9–11, and 12–14 were categorized as poor, moderate and strong social support respectively. The questionnaire have been widely used and validated in Nigeria [16-18].Participants were asked to rate financial distress experienced by the family during the COVID-19 pandemic. Responses ranged from 1 (no financial stress) to 5 (significant financial stress).The study instruments were piloted among 10 participants who were subsequently excluded from the study. This was to assess the test-retest reliability of the instruments. The numerical scores correlated well with pearson’s moment correlation coefficient of 0.76, 0.74 respectively for perceived stress scale, social support questionnaires. The instruments were thus adjudged reliable.DATA ANALYSIS: Descriptive statistics such as frequencies, mean and standard deviation were computed for socio-demographic characteristics of study participants. Inferential statistics such as chi square was used to determine the relationship between outcome and independent variables. Significant variables were entered into a logistic regression analysis model to determine predictors of psychological distress. Significance was computed at p < 0.05.The Statistical package for the social sciences 20 (SPSS Inc., Chicago, IL, USA) program was used for statistical analysis.
3. Result
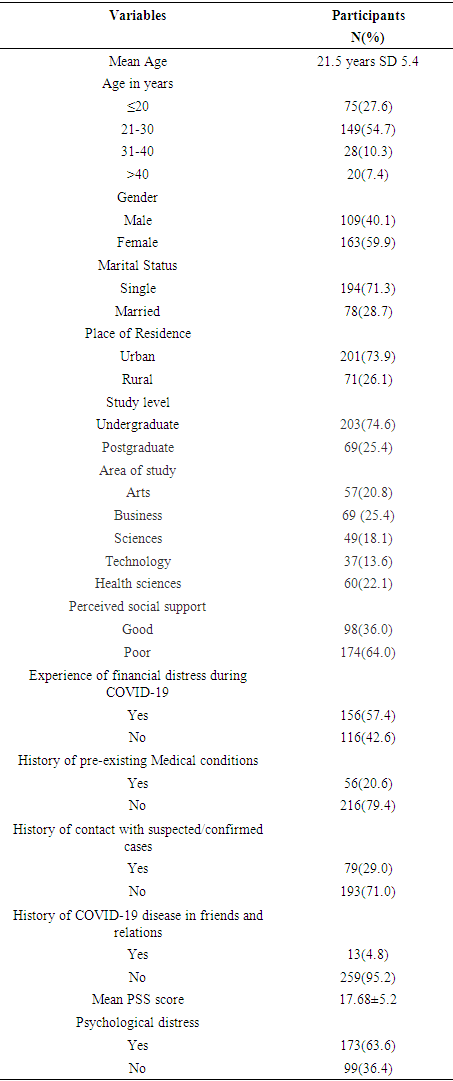
- Respondents’ characteristics.A total of two hundred and fifty two students participated in the study. The mean age of participants was 21.50 ± 5.4.years. Most participants were female (59.9%), single (71.3%), undergraduate students (74.6%), 87.2% of respondents had no history of pre-existing psychological or mental illness. 79.4% had no history of underlying medical conditions and most participants reported experiencing a financial strain during COVID-19 pandemic (57.4%).
|
|
|
4. Discussion
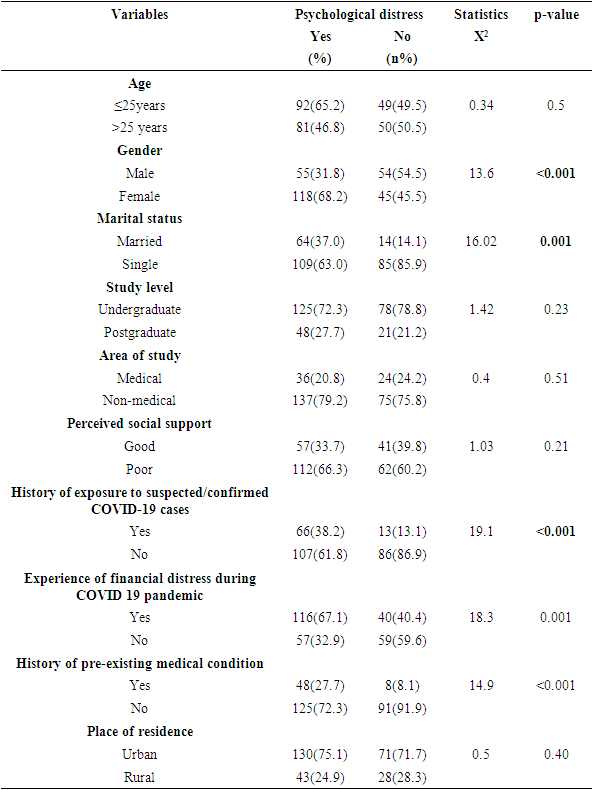
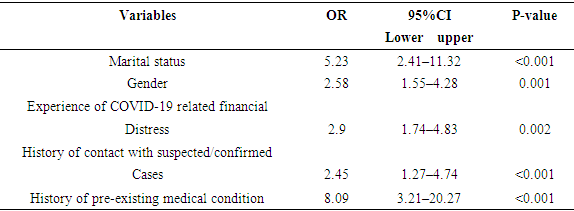
- This study assessed the prevalence of COVID-19 related psychological distress and related factors among university students in a tertiary educational institution in the South-South region of Nigeria. The COVID-19 pandemic has impacted college students’ coursework, stress levels, and perceived psychological health. Recent studies have indicated that high proportions of university students have experienced increased levels of psychological distress since the onset of the current COVID-19 pandemic [19,20].In the present study, the prevalence of psychological distress among university students was 63.6%. The prevalence level of psychological distress in the current study is in consonance with studies which have similar prevalence rates [21-22]. It is however in disagreement with other studies which have reported much lower prevalence of psychological distress [23-25]. Differences in reported rates of psychological distress across studies may be due to differences in the instruments used to measure stress, the sample size and characteristics and existing socio-cultural differences among countries [26]. The high level of distress observed in our sample may in part be related to the fact that university students being largely in the adolescence and early adulthood period may be at risk of increased psychological stress, in the light of challenges commonly associated with transitions to adulthood. Previous studies had reported high levels of psychological distress among the general populace during the SARS pandemic [13,27-30]. Demographic factors had varying impact on the level of psychological stress in our sample. In this study, gender was a factor in increasing the risk of developing psychological distress among university students. Female students reported greater levels of psychological distress scores compared to the male counterparts. This is consistent with previous research findings [22,31-33]. Plausible explanation for gender bias in developing psychological distress may in part be attributed to gender-specific conditions like menstrual cycle changes, pregnancy, miscarriage which may play additive role in promoting psychological stress in the female respondents [34,35].The marital status of respondents in our sample predicted the risk of increased psychological distress. This could be related to the fear of being source of infection to family members and friends. This is in agreement with recent studies which have reported that proximity to suspected or confirmed cases of the illness or exposure to COVID-19 cases was a factor in developing psychological distress [22,36]. The role of adverse socioeconomic factors in promoting psychological distress during COVID-19 pandemic was supported in this study. We found a significant relationship between poor financial status and the risk of developing psychological distress. This finding is similar to previous studies which have reported that financial hardship was an independently predictor of psychological distress. [36-39]. The negative economic consequences of COVID-19 disease have been on a global scale. Recent studies from many developing countries have reported high psychological distress in the general populace. Poor healthcare funding, inadequate healthcare facilities, paucity of qualified / specialist healthcare professionals, widespread poverty prevalent in many developing countries and have been cited as factors for increased psychological distress in these countries [40-43]. In the present study, Lack of widespread COVID-19 diagnostic testing, lack of efficacious treatments and lack of personal protective measures have been cited by a high proportion of respondents as reasons for high psychological distress. This is in agreement with recent studies from developing countries which have reported similar findings [36,40]. The presence of underlying medical conditions was associated with a high level of psychological distress in this study. Respondents with any underlying chronic medical conditions had higher psychological distress scores compared to those without such medical conditions. Recent studies have reported significant links between having an underlying chronic medical conditions and greater risk of developing psychological distress about COVID-19 disease [44,45]. This may be related to the fact that older adults and people of any age who have underlying medical conditions have worse illness prognosis [44].
5. Study Limitations
- This study has some limitations. The cross-sectional nature of the study with a single period of data collection may not allow for a good estimation of psychological distress status of this community which may fluctuate with time following waves of different strains of COVID-19 disease. Causal relationship between independent and outcome variables cannot be established in cross-sectional studies therefore, the finding of this study must remain exploratory. The specific nature and characteristics of our sample may also restrict the generalization of our findings. Also, the mental health status of participants was measured using self-report questionnaires. This might lead to an over-estimation of mental health worries by participants due to recall bias and recall difficulties [46].
6. Conclusions
- A high level of psychological distress exists in the university students’ community due to the ongoing COVID-19 pandemic. The high stress levels could impact the mental health of individuals, including students. Psychological support programs should be incorporated into response strategies in combating the COVID-19 disease in vulnerable groups to promote mental wellbeing and limit mental health consequences of the pandemic.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML