-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2021; 11(2): 59-73
doi:10.5923/j.phr.20211102.03
Received: Jul. 19, 2021; Accepted: Aug. 6, 2021; Published: Aug. 15, 2021

Multisectoral Approach to Improving Health Care Outcomes: A Systematic Review
Njuguna K. David1, Stephen Macharia2, Evelyne Chagina3
1Health Economist, Ministry of Health, Nairobi, Kenya
2Director Planning, Ministry of Health, Nairobi, Kenya
3Public Health Analyst, World Health Organization, Nairobi, Kenya
Correspondence to: Njuguna K. David, Health Economist, Ministry of Health, Nairobi, Kenya.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Efforts to improve health have traditionally looked to the health care system as the key driver of health outcomes. However, in cases where social determinants of health and other determinants of behaviour have been ignored, health inequalities have increased. There is an increased commitment to improving health and achieving health equity through multisectoral approaches that address social, economic, and environmental factors that influence health. This systematic review summarized evidence on the effectiveness of the multisectoral approach in improving health outcomes. We included twenty articles that relied on primary studies conducted in Australia, America, Africa and Asia. Eight studies reported on a multisectoral collaboration between Agriculture, Finance, Education and Health sector. Three studies reported a multisectoral collaboration between the education and health sectors to address concerns around vaccine hesitancy. Two studies reported collaboration between education and health sectors to address sexual and reproductive health issues. One study reported collaboration between education and health sectors to address drug and substance abuse issues. Another study reported collaboration between education and health sectors to address health and nutrition issues. One study reported collaboration between activists and health sectors to address neonatal health issues. Four studies reported collaboration between faith-based and health sectors to address varied health issues. Broadly, there was sufficient evidence to conclude that the multisectoral approach was effective in improving health outcomes including increased coverage, improved medication adherence, and high rates of retention in care, cessation of drug and substance abuse, vaccine acceptance and high screening rates for breast cancer. In conclusion there is a need to push for multisectoral approach as it contributes towards realising the sustainable development agenda of “leaving no one behind” and achieving the national and global targets.
Keywords: Multisectoral approach, Health outcomes, Stakeholder groups, Health inequalities, Sustainable development goals
Cite this paper: Njuguna K. David, Stephen Macharia, Evelyne Chagina, Multisectoral Approach to Improving Health Care Outcomes: A Systematic Review, Public Health Research, Vol. 11 No. 2, 2021, pp. 59-73. doi: 10.5923/j.phr.20211102.03.
1. Introduction
- The multisectoral approach (MSA) refers to deliberate collaboration among various stakeholder groups who work together to achieve a policy outcome. These stakeholder groups include governments, civil society, interfaith collaborations and the private sector such as the health sector, environment sector, and economic [1]. While the bulk of the responsibility for achieving Universal Health Coverage (UHC) is with the health sector stewarded by Ministries of Health, MSA is required to achieve UHC since it can leverage knowledge, expertise, reach and resources in other sectors [2]. The 2030 Agenda for Sustainable Development document is ambitious and explicit about the need for integrated and sustained action across various sectors to address complex challenges such as ending extreme poverty, reducing widening economic inequality, tackling climate change, and reducing and preventing conflict. These issues are beyond the remit and resources of a single thematic sector such as health, finance, agriculture, or education, and instead call for coordinated multisectoral action [3].MSA was introduced in the 1950s during technical discussions at the Fifth World Health Assembly [4]. It was later advanced in the Alma Ata Declaration in 1978 [5], at the Thirty-ninth World Health Assembly in 1986 and the WHO publication “Intersectoral action for health – the role of intersectoral cooperation in national strategies for health for all” [6], the Ottawa Charter in 1986 [7], the international conference on intersectoral action for health in 1997 [8], the WHO report on the social determinants of health in 2008 [9] and resolution WHA67.12 of the Sixty-seventh World Health Assembly [10]. In 2011, the Rio Political Declaration called for increased engagement of all sectors, stating that “We understand that health equity is a shared responsibility and requires the engagement of all sectors of government, of all segments of society, and of all members of the international community” [11]. In 2013, the review of social determinants and the health divide in the WHO European Region recommended developing more “partnerships at all levels of government that enable collaborative models of working, foster shared priorities between sectors and ensure accountability for equity” [12]. Globally, intersectoral action for health and well-being was called for in the Sixty-seventh World Health Assembly resolution A67/R12 [13]. The 65th session of the Regional Committee for Europe discussed the working paper Promoting intersectoral action for health and well-being in the WHO European Region: health is a political choice [14], which concluded that “intersectoral action is difficult to achieve, yet it is essential for the coherence, synergy and coordination of various sectors and provides a basis for accountability in the area of health”. These documents emphasized the need for all non-health sectors engaged in national and community development to coordinate their work to protect and promote the health of all people.Through MSAs, the education sector has implemented health programs for teachers, school children and their parents [15). The European Commission (2012) argued that education helps to promote equity, social justice and social inclusion by providing inclusive, caring and culturally responsive learning communities [16]. Modern school health programs include 10 interactive components: health education; physical education and physical activity; nutrition environment and services; health services; counselling, psychological, and social services; physical environment; social and emotional climate; family engagement; community involvement; and employee wellness [17]. Through MSAs schools have provided an organized structure that is conducive for the provision of health, nutrition services as well as a key avenue for disease prevention and control. The Beijing Declaration and Platform for Action in 1995 [18] and the UN Economic and Social Council in 1997 [19] have established gender mainstreaming as the global strategy for promoting, among other things, women health. A baseline assessment of informal settlements in Nairobi showed that women compared to men are more likely to have completely lost their source income due to a health emergency such as the pandemic, have increased housework, increased tensions in the home, forgone health services and skipped meals due to extra burden of care [20]. Gender mainstreaming incorporates the integration of women’s and men's concerns into the formulation, monitoring and analysis of policies, programmes and projects. It also takes into account gender issues that have implications for individuals and community health promotion. Through the MSAs, sectors dealing with gender-based issues have ensured that a ‘gender lens’ is applied to all health plans and programs. Health promotion as well as disease prevention needs to address these differences between women and men, boys and girls in an equitable manner in order to be effective [21].Agriculture, health, and nutrition are mutually reinforcing sectors [22]. Although the health sector is often tasked with the prevention and management of undernutrition, the agriculture sector is a key player in addressing the root causes. In 1937, the League of Nations articulated similar issues in a document called “The Relation of Nutrition to Health, Agriculture and Economic Policy” [23]. Through the MSAs, health promotion has shifted from an almost exclusive focus on nutrition-specific interventions, such as exclusive breastfeeding, to nutrition-sensitive interventions, such as diverse crop agriculture promotion, food fortification and water, sanitation, and hygiene (WASH) interventions [24]. In the past year as part of the response to the COVID 19 pandemic, the Government of Kenya is implementing non-health interventions to mitigate the socioeconomic impacts of the pandemic. These included reduction in individual income tax and value-added tax rates [25]. The response also necessitated involvement of other sectors such as the Ministry of Interior for enforcement of the public health measures to prevent COVID 19 and Ministry of education to implement school health surveillance and programs.Faith-Based Organizations (FBOs) have promoted a holistic approach to health by highlighting physical and spiritual wellbeing [26]. They ride on the existing institutional and community structures, links, large audiences and influence. Moreover, they provide context-embedded health responses which resonate with communities’ values and beliefs. They also serve the needy through their work ethics, community mobilization and ability to identify beneficiaries of health interventions. Among the highest-profile faith-based MSA successes is the President's Emergency Plan for AIDS Relief (PEPFAR), established in 2003 by President Bush's and continued under President Obama's administration. PEPFAR has drawn on the human and material resources of faith-based and community organizations that recorded over 250 million prevention outreach encounters during the Bush years. Under President Obama, it was part of the larger U.S. Global Health Initiative, established in 2009. This exemplifies the promise of faith-based initiatives as part of multisector, coordinated global health efforts [27].The United Nations Sustainable Development Goal (SDG) 17 recognizes the role of partnerships in addressing sustainability issues [28]. NGOs contribute and enhance health care services through collaboration with other non-state actors and government [29]. They represent the ‘voice of the people’ at local, national and international levels [30]. They are represented in policy formulation and can also be part of monitoring activities thereby making governments accountable for not performing well at the community level [31]. One instance in which, NGOs have participated in health policy formulation is during the creation and implementation of the WHO Framework Convention on Tobacco Control (FCTC) [32].The theories of reasoned action and planned behaviour [33] state that social norms and attitudes are determinants of behavioural intention, which is a predecessor to physical behaviour [34]. Consequently, raising awareness and influencing social norms and beliefs about others’ activity levels is a critical component of health promotion. Media is at the centre of multi-sectoral collaboration and integrating their role in communication and advocacy for improved health outcomes cannot be overemphasised. Mass media includes written, broadcast, or spoken communication that reaches public audiences and serves as an important mechanism for integration into a society [35]. The mass media has promoted healthy behaviour and actively fostered positive attitudes towards healthcare utilization [36] [37]. There is a significant legacy of multisectoral collaboration to fixing health issues. It is also evident that effective multisectoral collaboration can eliminate policy implementation barriers, facilitate scale-up, and increase the impact that one sector or partner may not achieve alone. Besides, it is essential for identifying intersections between the sectors involved and identifying opportunities for collaborative planning. However, sound empirical evidence for the effectiveness of MSAs is limited. As such, this systematic review sought to summarize evidence from primary studies reporting on the effectiveness of the multisectoral approach in improving health outcomes.
2. Methods
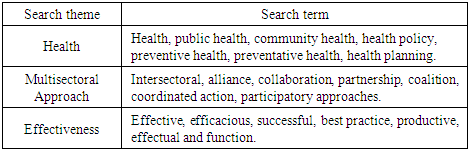
- This systematic review summarized evidence on the effectiveness of the multisectoral approach in improving health outcomes. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline [38) for systematic reviews design was adopted during the search for research articles in English. This systematic review was not registered with PROSPERO. PROSPERO is an international database of prospectively registered systematic reviews in health and social care.Search strategyA systematic search for published literature in English was conducted on PubMed and Google Scholar. References of retrieved articles and reports were screened to identify additional studies. Publication date, or publication status restrictions were not imposed. Non-empirical studies (commentaries, editorials, etc.), conference abstracts based on tertiary data, and studies that did not report multisectoral approach in improving health outcomes were excluded from the review. The search was guided by the social-ecological theory which is inherently interdisciplinary in its approach to health research and the development of health promotion programs. It integrates the community-wide, preventive strategies of public health and epidemiology with the individual-level, therapeutic and curative strategies of medicine. It also encompasses the behavioural and social sciences’ emphases on the active role played by persons and groups in modifying their health behaviour the development and testing of theoretical models describing people-environment transactions; and the importance of conducting evaluative studies to assess the cost-effectiveness and social impact of health promotion programs [39]. The keywords used in the search were Health, Multisectoral collaborations and effectiveness and their synonyms. The medical subject heading (MeSH) terms used are summarized in table 1 below.
|
3. Results
- We identified 417 articles: 385 articles through electronic databases and 32 through secondary references and hand-searching of journals. After the removal of duplicates, we screened 352 citations and pulled 151 articles for full-text articles review. Of the 151 full-text articles reviewed, we excluded 118 articles. We then excluded 13 studies during the extraction process and included 20 studies for the review (Figure 1).
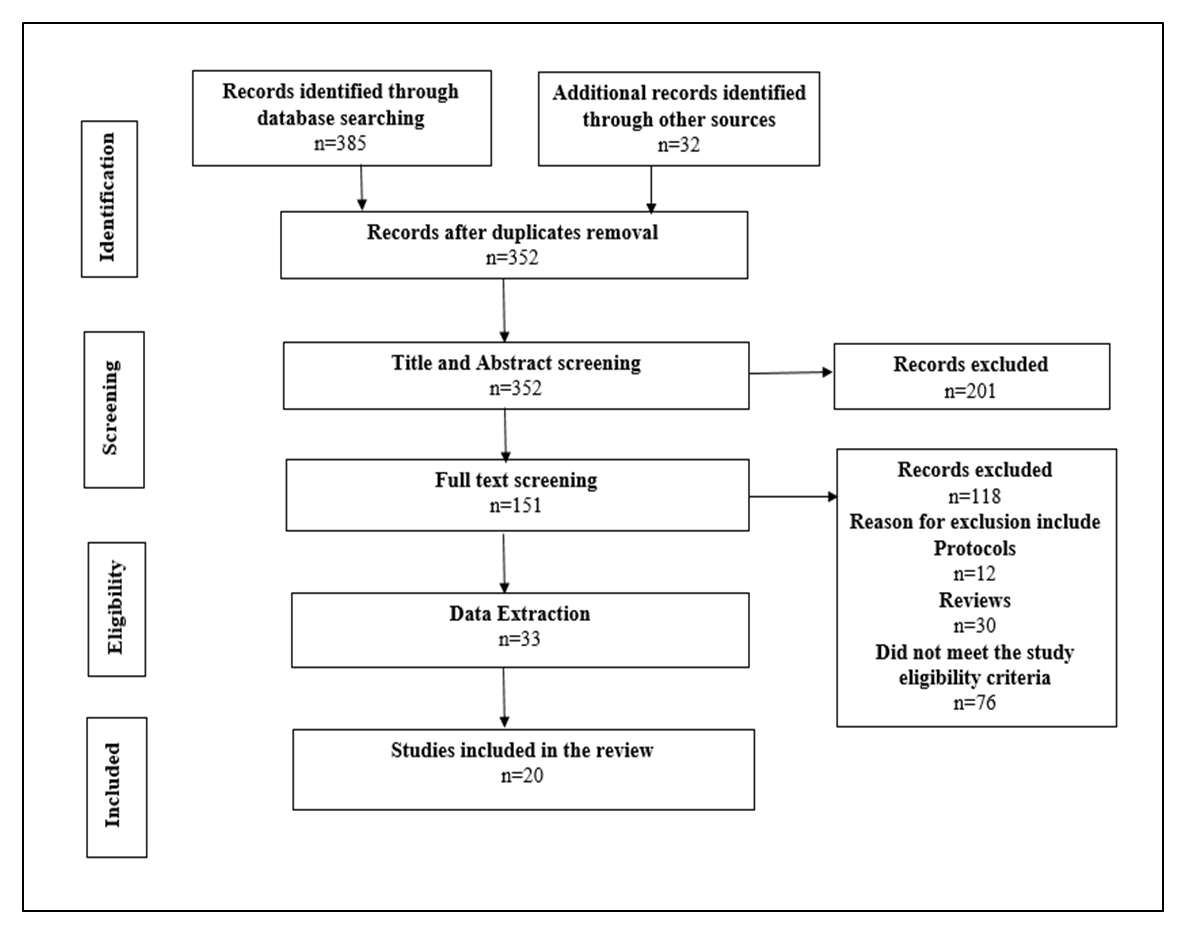 | Figure 1. Study flow diagram |
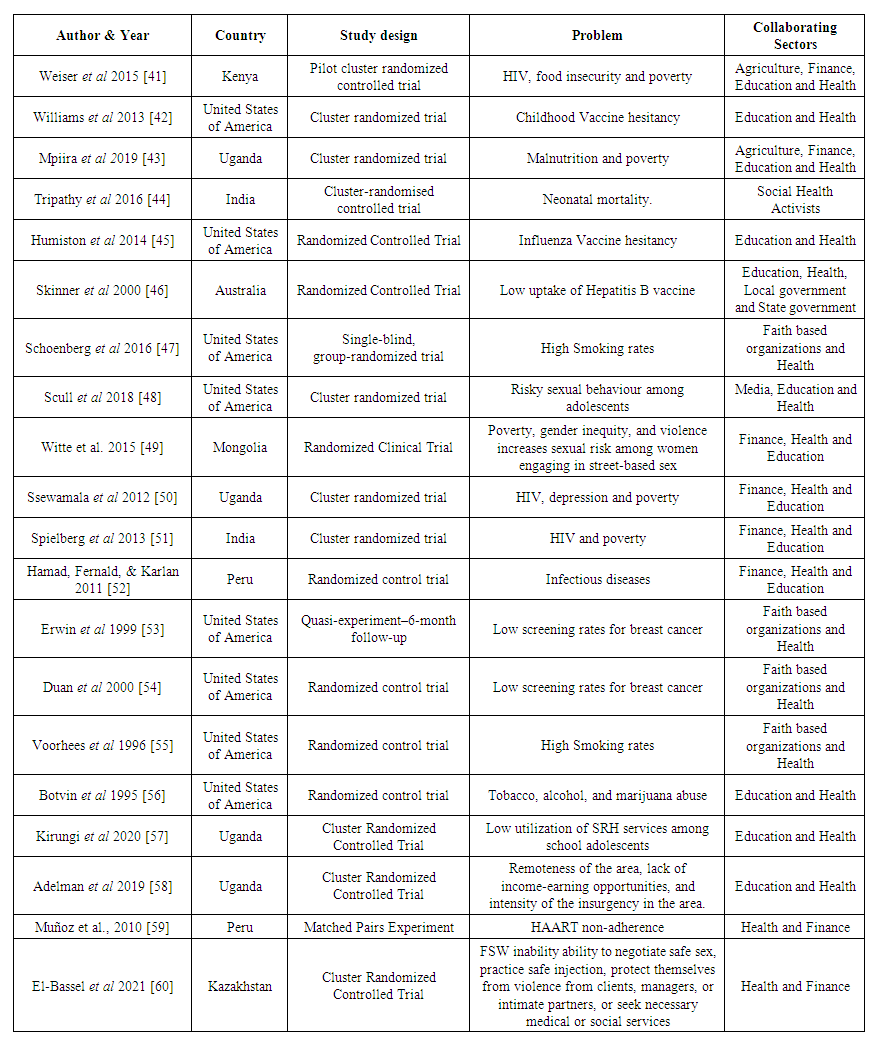 | Table 2. Study characteristics |
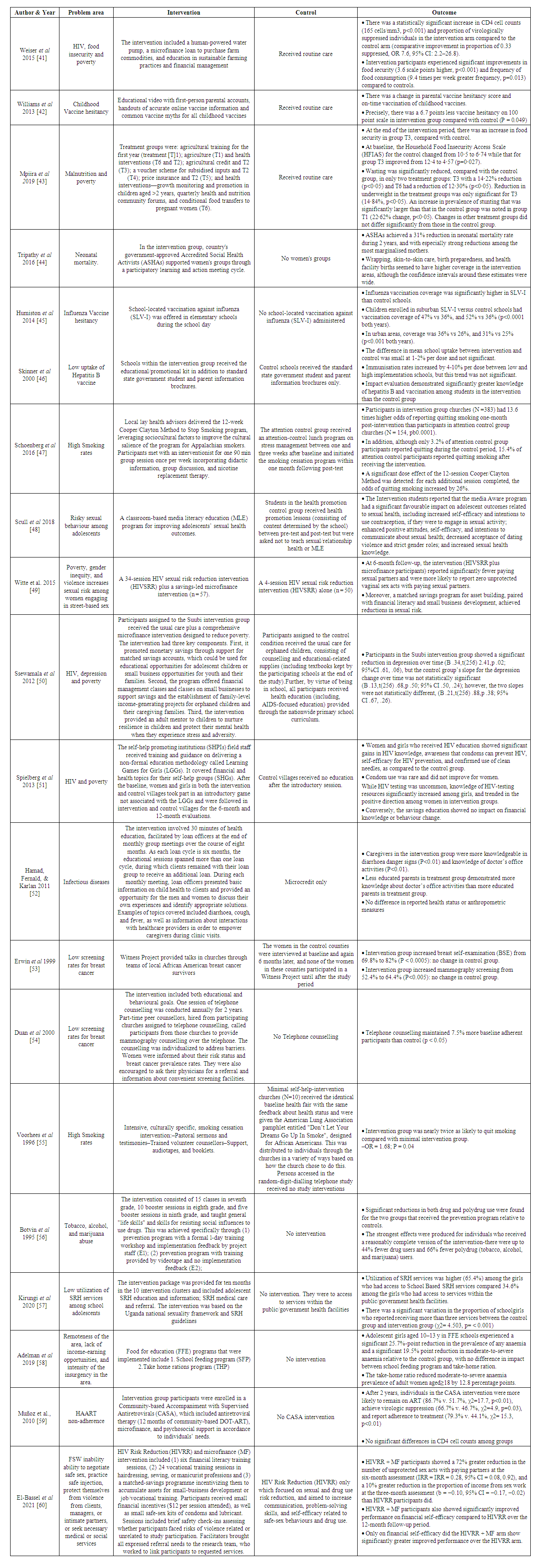 | Table 3. Summary of Evidence |
4. Discussion
- We undertook a systematic review of the effectiveness of the multisectoral approach in improving health outcomes. No such review has previously been published. The review found a broad range of stakeholders contributing to improving health outcomes. Despite the included studies being heterogeneous in terms of their geographic, economic, social, cultural, and historical contexts, we found sufficient evidence to conclude that the multisectoral approach was effective in improving health outcomes. However, the findings of this review does not reflect equal partnerships when delivering the interventions. Moreover, these studies did not identify the particular NGOs but described the contexts indicating multisectoral involvement. There is evidence of Multi-sectoral collaboration for improved nutrition and financial stability of participants. Food insecurity, poverty and poor health outcomes are linked in a vicious cycle that enhances vulnerability and worsens severity(61). Weiser et al 2015 [41] implemented a multisectoral agricultural and finance intervention which provided HIV-infected individuals with a human-powered water pump, a microfinance loan to purchase farm commodities, and education in sustainable farming practices and financial management. This intervention improved immunologic and virologic outcomes, food security, and diet quality for HIV-infected individuals suggesting that such interventions may be a promising approach to tackle the intersecting problems of food insecurity, poverty, and HIV/AIDS morbidity. Muñoz et al., 2010 [59] conducted a similar study in which a Community-based Accompaniment with Supervised Antiretrovirals (CASA), microfinance, and psychosocial support was provided in accordance to individuals’ needs. After two years, individuals in the CASA intervention were more likely to remain on ART, achieve virologic suppression, and report adherence to treatment compared to the control. Mpiira et al 2019 [43] also employed a multisectoral approach to eradicate malnutrition in pregnant women and children in Uganda. The combination of agricultural and health interventions together with the voucher scheme for subsidised agricultural inputs was generally more effective in increasing food security and reducing wasting and underweight than other treatment interventions. Witte et al. 2015 [49] assessed the efficacy of a Savings-Led Microfinance Intervention to Reduce Sexual Risk for HIV Among Women Engaged in Sex Work. They provided a 34-session HIV sexual risk reduction intervention (HIVSRR) plus a savings-led microfinance intervention and compared the findings to those of the control arm that offered a 4-session HIV sexual risk reduction intervention (HIVSRR) alone. At 6-month follow-up, the intervention participants reported significantly fewer paying sexual partners and were more likely to report zero unprotected vaginal sex acts with paying sexual partners. Besides, a matched savings program for asset building, paired with financial literacy and small business development, achieved reductions in sexual risk. El-Bassel et al 2021 [60] reported that HIV Risk Reduction (HIVRR) coupled with a microfinance (MF) intervention showed a 72% greater reduction in the number of unprotected sex acts with paying partners at the six-month assessment and a 10% greater reduction in the proportion of income from sex work compared to the controls who were only offered HIV Risk Reduction (HIVRR). Ssewamala et al 2012 [50] assessed the impact of a Comprehensive Microfinance Intervention on Depression Levels of AIDS-Orphaned Children in Uganda and reported a significant reduction in depression over time. Spielberg et al 2013 [51] conducted a study that leveraged microfinance to impact HIV and financial behaviours among adolescents and their mothers in West Bengal. They reported significant gains in HIV knowledge, awareness that condoms can prevent HIV, self-efficacy for HIV prevention, and confirmed use of clean needles, as compared to the control group. However, condom use, and HIV testing were uncommon. The savings education also showed no impact on financial knowledge or behaviour change. Similarly, Hamad, Fernald, & Karlan 2011 [52] also conducted a study in which health education was provided for microcredit clients in Peru. Caregivers in the intervention group were more knowledgeable in diarrhoea danger signs and knowledge of doctor’s office activities though no difference in reported health status or anthropometric measures. Overall, these findings highlight the need for a multisectoral approach that integrates agriculture, economic, nutrition, and health programs to improve outcomes in these sectors simultaneously. These multisectoral approaches contributes to the attainment of Sustainable Development Goals related to poverty (SDG 1), hunger (SDG 2), health (SDG 3), and education (SDG 4).Improved multi-sectoral collaboration has been initiated and promoted to enhance the acceptance of vaccines. Lack of confidence in vaccines threatens the success of vaccination programs and is responsible for decreasing vaccine coverage, increased risk of vaccine-preventable disease outbreaks and epidemics [62]. Decision making around vaccination entails a complex mix of cultural, psychosocial, spiritual, political, and cognitive factors [63]. Williams et al 2013 [42] conducted a multisectoral two-arm cluster-randomized trial which provided an educational video with first-person parental accounts, handouts of accurate online vaccine information and common vaccine myths for all childhood vaccines. There was a 6.7 points less vaccine hesitancy on 100-point scale in intervention group compared with control (P = 0.049) suggesting that a multifaceted approach can provide accurate information to parents who are concerned about the inherent safety and necessity of vaccines. Besides, it can be implemented without additional provider time, it addresses concerns prior to the clinic visit, and it can be applied under the supervision of the healthcare provider. Humiston et al 2014 [45] provided school-located vaccination against influenza (SLV-I) to curb vaccine hesitancy. Consequently, influenza vaccination coverage was significantly higher in SLV-I schools than control schools in both suburban and urban school districts. Skinner et al 2000 [46] also implemented an educational strategy to increase school-based adolescent hepatitis B vaccination. Schools within the intervention group received the educational/promotional kit in addition to standard state government student and parent information brochures. Immunisation rates increased by 4-10% per dose between low and high implementation schools, but this trend was not significant. Impact evaluation demonstrated significantly greater knowledge of hepatitis B and vaccination among students in the intervention than the control group. These finding demonstrate that schools are a key alternative delivery setting and has tremendous potential to increase vaccination coverage of school-going children. Moreover, school health activities promote equitable access to, and participation in, quality education by levelling the playing field for all students, supporting goals for equitable access and participation in a quality education [46]. Multi-sectoral collaboration involving the implementation of school health programmes has been vital in advocacy for school health policies and programmes in many countries. Education on sexual and reproductive health is a key priority in the development of a system wide Action Plan on Youth [64]. A school health education program that includes a quality sexual health education curriculum targets the development of critical knowledge and skills needed to promote healthy behaviours and avoid risks [65]. Scull et al 2018 [48] conducted a classroom-based media literacy education (MLE) program for improving adolescents’ sexual health outcomes. The intervention students reported a significant favourable impact on adolescent outcomes including, increased self-efficacy and intentions to use contraception, intentions to communicate about sexual health; decreased acceptance of dating violence and strict gender roles, and increased sexual health knowledge. Kirungi et al 2020 [57] also evaluated the effect of providing school based sexual and reproductive health services on utilization of the services among school girls aged 15-19 years attending secondary schools in Uganda. Utilization of SRH services was higher (65.4%) among the girls who had access to School Based SRH services compared 34.6% among the girls who had access to services within the public/government health facilities. These findings underscore the importance of multisectoral efforts to improve determinants of health, reduce inequities, create healthier environments, and increase coverage of health interventions. Multisectoral approaches incorporating media, education and health contributes to the attainment of sustainable development goal 3, target 3.7 which calls for universal access to sexual and reproductive healthcare services, including family planning, information and education, and the integration of reproductive health into national strategies and programmes [66]. There is also evidence of multisectoral collaboration to achieving sustainable development goal 3. target 3.5 which aims to strengthen the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol [67]. Botvin et al 1995 [56] evaluated the long-term efficacy of a school-based approach to drug abuse prevention. Significant reductions in both drug and polydrug use were found for the two groups that received the prevention program relative to controls. Reducing substance misuse is best addressed with a two-prong strategy to reduce the risk factors and increase the protective factors. In addition, there is substantial evidence of the value of school health and nutrition programs, including school feeding. Adelman et al 2019 [58] tested whether food fortified with multiple micronutrients provided in Food for education (FFE) programs reduced anaemia prevalence of primary-school-age adolescent girls, adult women, and preschool children. Adolescent girls aged 10–13 years in FFE schools experienced a significant 25.7% point reduction in the prevalence of any anaemia and a significant 19.5% point reduction in moderate-to-severe anaemia relative to the control group. While there was no difference in impact between school feeding program and take-home ration, the take-home ration reduced moderate-to-severe anaemia prevalence of adult women aged ≥ 18 by 12.8 percentage points. By improving the health and wellbeing of learners, effective school health and nutrition programs improve both access to school and health outcomes. For interventions in the schools, at a minimum, the health, and education sectors need to work together. Through multisectoral collaboration, different sectors have been able to advocate making health a priority of government and government. Public health activism refers to the collective efforts to redistribute power in ways that create more health-enabling social environments in conditions of social inequality [68]. It plays an important role in carrying out broader, long-term health campaigns for better choices. Tripathy et al 2016 [44] assessed the effect of participatory women's groups facilitated by Accredited Social Health Activists on birth outcomes in rural eastern India. The Accredited Social Health Activists supported women's groups through a participatory learning and action meeting cycle where they discussed and prioritised maternal and new-born health problems, identified strategies to address them, implemented the strategies, and assessed their progress. Consequently, they reported a 31% reduction in neonatal mortality rate in two years, especially among the most marginalised mothers. These findings showcase the ability of multisectoral approach to provide a “soft-targeting” since they are open to all, occur at a time decided by women themselves, and also take place in remote areas with marginalised groups. Taking such a multisectoral approach can leverage the inclusion and protection of marginalized groups by enhancing coverage and supporting efforts to leave no one behind.Multisectoral collaboration has opened a window for with faith-based organizations (FBOs) to address health disparities. There is evidence of the commitment to address health disparities by engaging faith-based organizations (FBOs). This is consistent with the resolution passed by the Thirty-seventh World Health Assembly, in 1984, which called upon WHO Member States to include a spiritual dimension in their health strategies based on their social and cultural patterns [69]. Schoenberg et al 2016 [47] conducted a randomized controlled trial in which a faith-placed, lay health advisor delivered smoking cessation intervention for rural residents. Participants met with an interventionist for one 90 min group session once per week incorporating didactic information, group discussion, and nicotine replacement therapy. Those in intervention group churches had 13.6 times higher odds of reporting quitting smoking one-month post-intervention than participants in attention control group churches. Also, for each additional session completed, the odds of quitting smoking increased by 26%. Voorhees et al 1996 [55] also provided an intensive, culturally specific, smoking cessation intervention which included pastoral sermons and testimonies, trained volunteer counsellors support, audiotapes, and booklets. The intervention group was nearly twice as likely to quit smoking compared with minimal intervention group.Erwin et al 1999 [53] conducted a quasi-experiment in which the Witness Project provided talks in churches through teams of local African American breast cancer survivors to increase mammography practice. The intervention group increased breast self-examination (BSE) from 69.8% to 82% and mammography screening from 52.4% to 64.4% with no change being reported in control group. These findings are consistent with that of Duan et al 2000 [54] who conducted a study to maintain mammography adherence through telephone counselling in a Church-Based Trial. This telephone counselling maintained 7.5% more baseline adherent participants than control.
5. Conclusions
- It is evident that multisectoral approach is effective in improving health outcomes through leveraging on knowledge, resources and combined strengths and expertise by contributing to health and sustainable development goals, collaborative relationships, innovation, scaling up and sustainability. Moreover, the challenging task of improving public health is better achieved by avoiding duplication of inputs and activities and subsequently increasing efficiency or efficacy. There is a need to build on local resources and structures, embed quality assurance mechanisms within implementation, and ensure relevance and adaptability to context.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML