-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2021; 11(2): 44-58
doi:10.5923/j.phr.20211102.02
Received: May 28, 2021; Accepted: Jun. 16, 2021; Published: Jun. 26, 2021

Opportunities and Challenges for HIV/AIDS and Non-Communicable Diseases Integration: A Systematic Review of Different Models of Integrated Care
Njuguna K. David1, Oren Ombiro2, Caroline Kawila3
1Health Economist, Ministry of Health, Nairobi, Kenya
2Public Health Specialist, Department of NCDs, Ministry of Health, Nairobi, Kenya
3Health System Management Expert, Department of Health Systems Management, School of Medicine and Health Sciences, Kenya Methodist University, Nairobi, Kenya
Correspondence to: Njuguna K. David, Health Economist, Ministry of Health, Nairobi, Kenya.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

It is evident that HIV and Non-Communicable diseases (NCD) programs often intersect. However, HIV services are stand alone and decentralized making it attractive to patients in peripheral facilities, and retaining them in care. In contrast, NCD care is provided using a centralised model, with the majority of care provided by hospitals. Patients have limited access and commonly present late with symptoms of complications. Therefore, HIV/NCD integration would strengthen the health systems capacity to address the full range of needs for HIV patients, at both the population and individual level. This systematic review explores the pertinent opportunities and challenges for HIV/NCD integration in comparison to different models of integrated care. Twenty studies with some conducted in America, Africa and Asia that heavily relied on primary data and implied that HIV/NCD integration increases the utilization of healthcare services and improve health outcomes were examined. Three studies reported increased utilization and improved outcomes through a population-based model of integrated care, however, reported challenges with linkage to care, loss to follow up and low levels of male involvement. Seventeen studies reported on individual models of integrated care which translated into impressive health outcomes including efficiency gains in staffing, increased coverage, improved medication adherence, and high rates of retention in care. One study reported on a case management approach that was found to be more effective when supporting integrated services for depressed HIV patients. The review findings show that intense efforts are needed to improve male involvement, invest in point of care technologies, reduce the return visit rates and provide streamlined care to reduce the loss to follow up for individual-based models of integrated care. There is diversity in integration models combining HIV and NCD services, and they have the potential in yielding positive patient and service delivery outcomes when implemented within appropriate contexts.
Keywords: HIV/AIDS, Non-Communicable Diseases, Models of integration, Opportunities, Challenges
Cite this paper: Njuguna K. David, Oren Ombiro, Caroline Kawila, Opportunities and Challenges for HIV/AIDS and Non-Communicable Diseases Integration: A Systematic Review of Different Models of Integrated Care, Public Health Research, Vol. 11 No. 2, 2021, pp. 44-58. doi: 10.5923/j.phr.20211102.02.
1. Introduction
- The World Health Organisation (WHO) defines integration in healthcare systems as “bringing together inputs, delivery, management and organization of services related to diagnosis, treatment, care, rehabilitation and health promotion” to “improve access, quality, user satisfaction and efficiency” [1,2]. Moreover, the WHO recognises the importance of integrated care and recently developed a ‘Framework on integrated people-centred health services’ calling for fundamental change in the funding, management, and delivery of health services [3]. The compelling reasons to integrate healthcare services include the fact that the underlying determinants of the major health challenges are similar and synergistic. The key beneficiaries of health services are often the same, integration of care minimizes duplication of scarce resources, and promotes efficiency [4]. Integrating healthcare also improves the effectiveness of outcomes and enhances the sustainability of health, social and environmental goals broadly [5].In 2019, 38 million people in the globe were living with HIV, 1.7 million people became newly infected with HIV, while 690,000 people died from AIDS-related illnesses [6]. Non-communicable diseases (NCDs), also known as chronic diseases cause 71% of all deaths globally. More than 15 million people aged between 30 and 69 years die every year from an NCD and 85% of these "premature" deaths occur in low- and middle-income countries [7]. The disability-adjusted life year (DALY) burden from NCDs was estimated to be 37% in low-income countries in 2015 [8]. NCDs, including cardiovascular disease, diabetes, cancer, and mental health problems, are common among people living with HIV (PLHIV) and threaten the progress of HIV treatment programs [9]. This can be attributed partly to HIV infection [10,11] and the complications of long-term antiretroviral therapy [12–14]. HIV services are stand-alone and are vertically delivered. Besides, they are decentralized and delivered by task shifting, which enables the treatment of many patients [15]. In contrast, health service coverage for NCDs remains very low [16,17]. The interventions for NCDs are rarely included in national primary care packages and are often paid for via out-of-pocket medical payments, which can lead to catastrophic health expenditure and impoverishment [18]. The global AIDS response is primarily donor-supported and addresses HIV and common opportunistic infections, with limited focus on other conditions [19].Consequently, there are significant gaps in the cascade of care for NCDs in countries that are on track to meeting the aspirational 90-90-90 targets [20]. There is a need to coordinate efforts and achieve synergies to benefit patients. The epidemiologic transition and double disease burden from chronic infections and Non-communicable diseases (NCDs) worldwide require re-engineering of healthcare delivery systems [21]. HIV/NCD integration is the coordination, co-location, or simultaneous delivery of HIV and NCD services to people who need them when they need them [9].Various models and approaches to integrated care have been applied based on different objectives. Individual models of integrated care deal with individual coordination of care for high-risk patients with multiple conditions, to facilitate the appropriate delivery of health care services and overcome fragmentation between providers [22]. Case management is an example of an individual model of integrated care. It ensures coordination of a patient’s care through the assignment of a case manager who assesses the patient’s and carer’s needs, develops tailored care plan, organizes and adjusts care processes accordingly, monitors the quality of care and maintains contact with the patient and carer. A patient-centred medical home is another example. It is physician-directed and provides care that is accessible, continuous, comprehensive, coordinated and delivered in the context of family and community [23].Disease-specific integrated care models provide better integration of care for people with certain diseases and long-term conditions such as diabetes mellitus, cardiovascular diseases, chronic obstructive pulmonary disease (COPD) and bronchial asthma [24–28]. The chronic care model is one such model that aims to meet the needs of people with chronic illnesses and provide a comprehensive framework for the organization of health services to improve their outcomes. It suggests a shift from acute, episodic and reactive care towards care that embraces longitudinal, preventative, community-based and integrated approaches [29].Population-based models of integrated care shifts the healthcare system from a narrow model of acute care targeted at the individual patient, to one that focuses on the health and overall wellness of the broader population it serves [30]. Kaiser Permanente (KP) is one such model and is based on stratification of the population and supply of different services based on needs. It ensures the population receives promotion and prevention services to control exposure to risk factors. The majority of chronic care patients receive support for self-management of their illness and high-risk patients receive disease and case management, which combines self-management and professional care [23].While these models of integrated care aim to achieve continuity of care and address the complex needs of patients with chronic conditions, there is a lack of clarity in the actual degree of integration and the bottlenecks experienced specifically in the context of HIV/NCD integration. To date, documentation of health system challenges and opportunities presented for HIV/NCD integration using different models is limited. As such, this systematic review sought to unravel the pertinent opportunities and challenges for HIV/NCD integration using different models of integrated care.
2. Methods
- This systematic review explored the opportunities and challenges of HIV/NCD integration using different models of integrated care. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline [31] for systematic reviews design was adopted during the search for research articles in English. This systematic review was not registered with PROSPERO.Search strategyA systematic search for published literature in English was conducted on PubMed and Google Scholar. References of retrieved articles and reports were screened to identify additional studies. Publication date, or publication status restrictions were not imposed. Non-empirical studies (commentaries, editorials, etc.), conference abstracts based on tertiary data, and studies that did not examine HIV/NCD integration were excluded from the review. The keywords used in the search were HIV, integration and chronic diseases and their synonyms. The following Medical Subject Heading (MeSH) terms were used: ‘HIV’ and/or ‘Acquired Immunodeficiency Syndrome’ combined with one or more of the terms ‘hypertension’, ‘heart diseases’, ‘cardiovascular diseases’, ‘diabetes’ ‘cancer’, ‘lung disease’, ‘pulmonary disease, chronic obstructive, ‘asthma’, 'mental health', 'depression' and ‘primary health care. Additionally, we used the non-MeSH search terms ‘non -communicable diseases’ and ‘out-patient department and integration’.Study eligibilityThe following inclusion criterion were considered for all publications and reports;• Population: HIV positive patients presenting with NCDs. There were no geographical restrictions (Globally). • Intervention: Integration of HIV/NCD healthcare services.• Comparator: There was no comparator for this review.• Outcome: The outcome measures were the available opportunities for implementation of various integration models and the challenges experienced with the implementation of these models.All studies that reported on the effects of different models of HIV/NCD integration using quantitative, qualitative and mixed methods were included specifically including the following:• Studies reporting actual integration experiences.• Studies reporting screening or treatment for HIV within a service targeting other NCD or vice versa.• Studies describing services provided in health facilities or the community and concerning any adult population.Exclusion criteriaFull texts and abstracts were excluded if• They were not primary studies e.g. reports, literature reviews.• They did not describe HIV/NCD integration.• Studies published in languages other than English.Study selectionTwo individuals independently reviewed these articles. Titles and abstracts of the identified selected studies were screened to exclude duplicates and studies not relevant to the topic. The eligible titles and abstracts were then reviewed in full text. Data ExtractionFull-text articles that fit the inclusion criteria were extracted into a matrix (MS Excel file) for the following implementation-related content: title, author, publication year, country, disease condition, integrated care model, challenges and opportunities. All disagreements were re-examined jointly and appropriate corrections made for all studies included in the review. All information related to the study objective was then presented in narrative form.Assessment of methodological qualityAssessment of the risk of bias in included studies was done using the recommended risk of bias tools. The reviewed literature was then summarised after the team was convinced that the evidence was certain using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) tool [32].
3. Results
- Overall characteristics of publicationsA total of 516 published journal articles were identified, however only 478 were legit. These were screened by title and abstract for inclusion. 253 studies were included in the full-text screening after which 178 studies were excluded after lacking concrete information that could inform the review, leaving 75 records that were assessed and for data extraction. in the process of extraction, a further 55 studies were excluded. Only 20 studies were finally included for the review (Figure 1). 13 out of 20 publications, originated from Africa, five from the United States of America, one study originated from Asia and one from North America. All articles were published in peer-reviewed journals between the years 2000 and 2020. The external validity of these studies is clear because the most studies discuss the generalizability of their results. Due to the heterogeneity in study design, intervention types, participants, and outcomes, a meta-analysis was not conducted but instead, the review presents a summary of the articles and a synthesis of their results and outcomes where available. Table 1 summarizes the study characteristics and the findings.
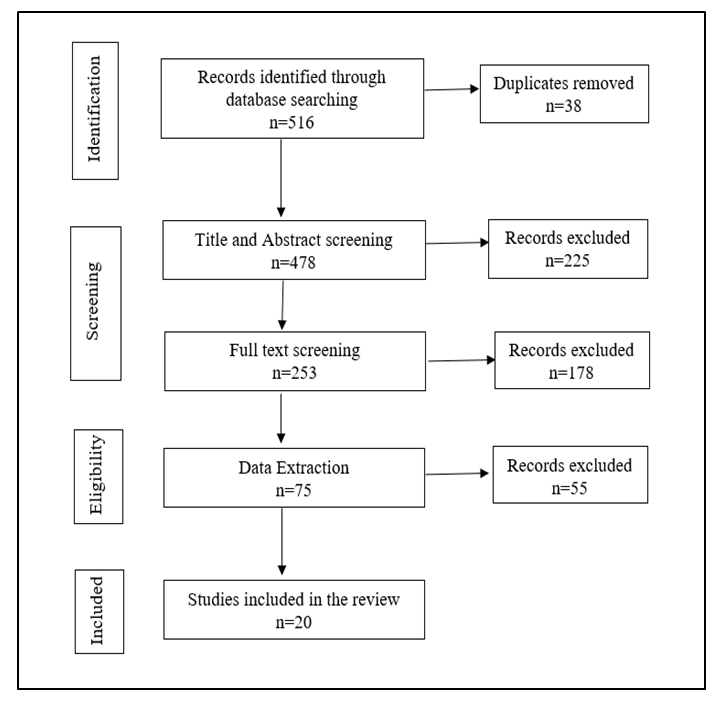 | Figure 1. Study flow diagram |
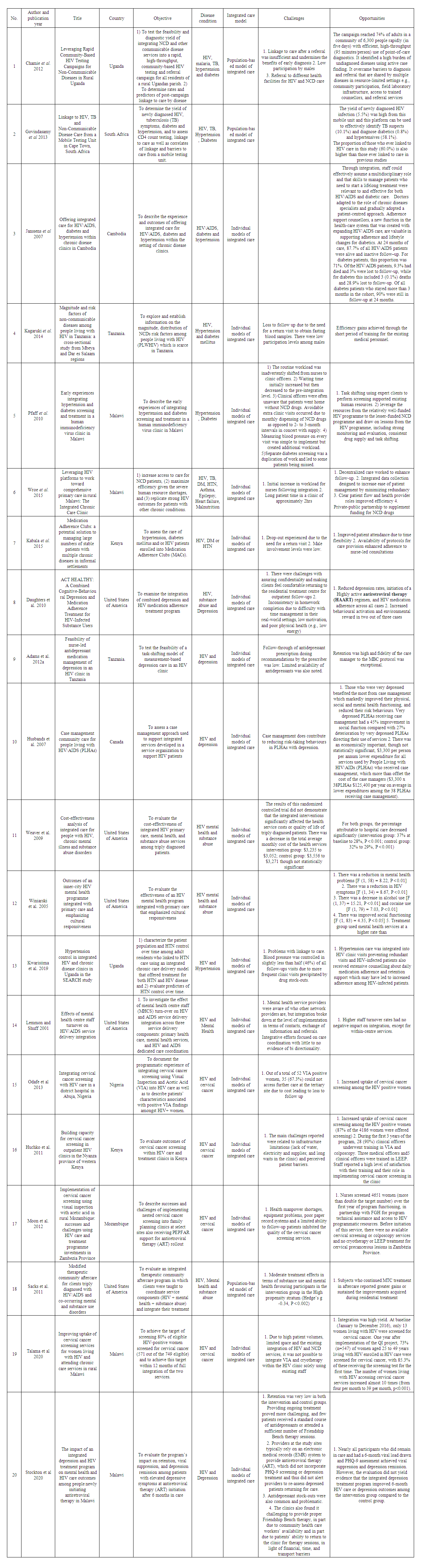 | Table 1. Summary of findings |
4. Discussion
- This study review provides the first direct comparison of the different models of integrated care. It offers a unique look at HIV/NCD context since populations are increasingly demonstrating comorbid NCDs, such as hypertension, diabetes, kidney disease, depression, cervical cancer, and substance abuse with HIV. Population-based models of integrated care as demonstrated by Chamie et al 2012 [33] and Govindasamy et al 2013 [34] show increased utilization of services and identified high burden of undiagnosed diseases through active case finding. The increased service utilisation can be attributed to the extensive community mobilisation that led to improved awareness and created more opportunities for access to integrated services unlike before. These findings suggest that the opportunity to increase utilization of integrated HIV/NCD services through the population-based models of integrated care needs to be embraced broadly as this may be effective in resource-constrained settings. These findings are consistent with those of study done in rural Kenya that offered community-based HPV screening at pop-up tents during a two-week phase of a community health campaign. The community health campaigns had 60% uptake compared to the control community where women were referred to their local government health facility for testing, resulting in 37% uptake [35]. Sacks et al. 2011 also evaluated an integrated therapeutic community aftercare program in which clients were taught to coordinate service components [HIV + mental health + substance abuse] and integrate their treatment. They also reported gains or sustained improvements during residential treatment [36]. This suggests that empowering the patients increase positive treatment outcomes while reducing the burden on healthcare resources and capacities.Something to note is the low male involvement levels in population-based models of integrated care. Barker 2014 hypothesizes that involving men in the HIV/NCD program addresses gender inequity, acknowledges men's capacity to act as agents of change and can support men to challenge pre-existing roles and norms surrounding masculinity, intimate partner relationships and parenting [37]. This points to the need for greater incorporation of gender-transformative conceptual approaches into population-based models of integrated care, with effective measures built in to develop the evidence base for their impact on a broad range of health and gender equity outcomes [38]. Moreover, linkage to care is a challenge in population-based models of integrated care. These findings indicate the need for intensive interventions including transport vouchers, community escorts and supportive counselling, to ensure ART-eligible patients link to care and initiate ART promptly [39]. Individual models of integrated care have been widely implemented for the integration of HIV with NCDs such as HIV/AIDS, diabetes, hypertension, epilepsy, asthma, mental illnesses, substance abuse and cancer [40,41,50–56,42–49]. The opportunities presented by the individual models of integrated care were efficiency gains in staffing and improved coverage of NCD care. Janssens et al 2007 showed that with integration, staff effectively assumed a multidisciplinary role and the skills to manage patients who were required to start a lifelong treatment for both HIV/AIDS and diabetic care. Doctors adapted to the role of chronic diseases specialists and gradually adopted a patient-centred approach while adherence support counsellors, a new designation that was created with expanding HIV/AIDS care supported adherence and lifestyle changes for diabetics [40]. Task shifting was also implemented by Pfaff et al. 2010 [42] and Wroe et al 2015 [43] where expert clients were used to performing screening thereby, supported existing human resources. These findings are consistent with those of Callaghan et al who demonstrated that task shifting is a viable and rapid response to sub-Saharan Africa's human resources crisis in HIV care [57]. However, there is a need to ensure the quality of care for HIV and NCD integrated services is not compromised by generating high rates of internal quality control failures and long turnaround times. The results highlight a need to strengthen health systems, with an emphasis on staffing, and training.It is also evident that individual models of HIV/NCD integration translated into impressive health outcomes including increased coverage, improved medication adherence, and high rates of retention in care. Janssens et al.2007 showed that at 24 months of care, 87.7% of all HIV/AIDS patients were alive and inactive follow–up. Besides, 90% of all diabetes patients who stayed more than 3 months in the cohort were still in follow-up at 24 months [40]. Daughters et al 2010 examined the integration of combined depression and HIV medication adherence treatment program and reported reduced depression rates, initiation of a HAART regimen, HIV medication adherence across all cases, increased behavioural activation and environmental reward in two out of three cases [45]. Adams et al 2012a also reported high retention and exceptional fidelity of the care manager to the measurement-based care protocol for HIV and depression integration [46]. Husbands et al 2007 assessed a case management approach used to support integrated services for depressed HIV patients. They found that very depressed PLHAs on case management had a 45% improvement in social function compared with 27% deterioration by very depressed PLHAs directing their use of services [47]. However, this requires the case managers to have adequate training in the separate areas of HIV, and mental health, and are well supported, if they are to coordinate care effectively. Winiarski et al 2005 evaluated the effectiveness of an HIV mental health program integrated with primary care and reported a reduction in mental health problems and HIV symptoms, a decrease in alcohol and cocaine use and improved social functioning [49]. Hypertension care integrated into HIV clinic visits prevented redundant visits. Moreover, HIV-infected patients also received extensive counselling about daily medication adherence and retention support leading to increased adherence among HIV-infected patients [50]. Odafe et al 2013, Huchko et al 2011, Moon et al 2012 and Talama et al 2020 reported increased uptake of cervical cancer screening among HIV positive women [52–55]. These findings are consistent with those of Goldie et al (2005) who showed that the most clinically effective and cost-effective strategies for cervical cancer prevention were those that had low rates of attrition between screening and treatment, through either a reduced number of visits or strategies to improve patient follow-up [58]. Stockton et al 2020 achieved viral suppression and depression remission for nearly all participants who remained in care and had a 6-month viral load drawn and PHQ-9 assessment [56]. While service integration and linkages can improve care and reduce missed opportunities, the need for a return visit to obtain fasting blood samples led to a loss to follow up among people living with HIV and diabetes mellitus in Tanzania [41]. This was also experienced by hypertension, diabetes mellitus and HIV patients enrolled on Medication Adherence Clubs (MACs) in Kenya [44]. Kwarisiima et al 2019 also reported problems with linkage to care. Blood pressure was controlled in slightly less than half (46%) of all follow-up visits due to more frequent clinic visits precipitated by drug stock-outs [50]. Despite studies reporting staff satisfaction with the integrated services, increased staff workload [42,43], and shortage of staff [54] were other challenges reported, for individual models of integrated care. This suggests the need for incentivizing staff working within the system and training in new skills while ensuring mentoring and supervision facilitates integration. On the contrary, Lemmon and Shuff 2001 reported that high staff turnover rates had no negative impact on integration, except for within-centre services [51].One unique challenge with the integration of HIV and mental health services is conceptualizing the social and cultural context of the mentally ill PLWHIV. Daughters et al 2010 examined the integration of combined depression and HIV medication adherence treatment program and reported challenges with consistent homework completion due to difficulty with time management in their real-world settings, low motivation, and poor physical health. Also, there were challenges with assuring confidentiality and making clients feel comfortable returning to the residential treatment centre for outpatient follow-ups [45]. Increasing awareness and reducing stigma, especially that associated with HIV and mental illness amongst the wider population, may influence substantially the extent to which integration will be feasible and lead to better health outcomes. This calls for considerations of the social and cultural context in which depressed HIV patients conceptualize their beliefs, understand mental illness and receive treatment. Moreover, support interventions should be tailored to their gender and age, and provide them with skills to improve their livelihoods [59]. Institutional structures and infrastructure including financial resources and medical supplies were challenges experienced with individual models of integrated care. Adams et al 2012a and Kwarisiima et al 2019 reported limited availability of drugs which precipitate loss to follow up [46,50]. Cost concerns also limited access to further care leading to loss to follow up [52]. Huchko et al 2011, Talama et al 2020 and Moon et al 2012 reported infrastructure limitations, manpower shortages, equipment problems, poor paper record systems and a limited ability to follow-up patients as barriers that inhibited the quality of cervical cancer screening services [53–55]. This evidence points to the need to maximize investments and open new grant channels to specifically support these areas.
5. Study Limitations
- The studies reviewed report in depth diabetes and depression integration with HIV compared to other NCDs. More research needs to be conducted to put into perspective challenges and opportunities of integrating HIV with other NCDs such as hypertension, asthma, cardiovascular disease and many more.
6. Conclusions
- All (100%) body of evidence reviewed supports the notion that integrated programs addressing HIV/NCD integration provide stronger impacts on health outcomes. In contrast, 85% of the literature reviewed reported several challenges for HIV/NCD integration. Both population-based and individual-based models of integrated have notable opportunities such as increased coverage and improved health outcomes as demonstrated in the studies reviewed. However, population-based models may be more efficient than individual based models, because they are intended for the same population and make use of the same facilities, transportation, and client contacts. Existing opportunities for leveraging and linking beneficiaries to the available population-based HIV/NCD integrated services need to be embraced since they are high yield and cost effective. While implementing population-based models, more efforts are required to improve male involvement, investing in point of care technologies, reducing the return visit rates and providing streamlined care to reduce the loss to follow up.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML