-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2020; 10(4): 111-118
doi:10.5923/j.phr.20201004.01
Received: July 3, 2020; Accepted: July 29, 2020; Published: August 15, 2020

Does Access to Health Care Guarantee Quality of Care: An Enquiry into the Trend of Facility Deliveries and Maternal Mortality Following the Implementation of Free Maternity Care in Kenya
Njuguna K. David 1, Janette Karimi 2, Samuel Cheburet 3
1Health Economist, Ministry of Health, Nairobi, Kenya
2Reproductive Health M&E Specialist, Ministry of Health, Nairobi, Kenya
3Health Information Expert, Ministry of Health, Nairobi, Kenya
Correspondence to: Njuguna K. David , Health Economist, Ministry of Health, Nairobi, Kenya.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: The reduction and elimination of maternal mortality remain a challenge in most low income countries. Kenya joined other African countries in the abolishment of delivery fees in all public health facilities through a presidential directive signed into effect on June 1, 2013. Unfortunately, this does not guarantee its use and optimal outcomes. This study aimed to demonstrate the trends in facility-based deliveries and maternal mortalities in Kenya from the year 2012 to 2019, and programmatic efforts for increasing quality, coverage, and utilization of BEmONC services as well as critical support systems at all referral levels. Setting: Health facilities in the 47 counties in Kenya. Methods: Data was extracted from the Kenya Health Information System (KHIS). Descriptive analysis of 8 years trend (2012-2019) was adopted complemented with univariate and bivariate analysis with figures. Outcome: Overall, evidence on the implementation of the free maternity policy showed increased utilization of health facilities but did not have a significant effect on maternal mortality. The facility deliveries and maternal mortality across the 8 years followed the same trend, and the difference across years statistically remained the same. Increased mortality with increased utilization points to a crucial gap in quality of care. Conclusions: Increasing facility birth does not translate into reduced mortality unless quality of care is assured. There is need to strengthen the capacity of the supply side through sustainable financing, strengthen institutional capacity for delivery of quality RMNCAH services, build strong leadership and a coherent institutional response, leverage changes in public policy and build a knowledge base and monitoring progress.
Keywords: Maternal mortality, Health facility deliveries, Utilization, Quality, Free maternity
Cite this paper: Njuguna K. David , Janette Karimi , Samuel Cheburet , Does Access to Health Care Guarantee Quality of Care: An Enquiry into the Trend of Facility Deliveries and Maternal Mortality Following the Implementation of Free Maternity Care in Kenya, Public Health Research, Vol. 10 No. 4, 2020, pp. 111-118. doi: 10.5923/j.phr.20201004.01.
Article Outline
1. Introduction
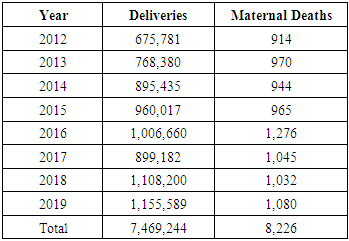
- Adult and maternal mortality rates are key indicators of the health status of a population [1]. A maternal mortality is defined by the 9th and 10th revisions of the International Classification of Diseases as the death of a woman while pregnant or within 42 days of the termination of pregnancy, irrespective of the duration or site of the pregnancy and which results from any cause related to or aggravated by pregnancy or its management [2]. Reducing maternal mortality has been on top of the global health agenda and plays a crucial role in the overarching health goals of the Sustainable Development Goals (SDGs) 2030 [3]. In February 2015, the World Health Organization published “Strategies toward ending preventable maternal mortality (EPMM)” (EPMM Strategies) [4]. This report outlines global targets and strategies for reducing maternal mortality under the SDGs. The EPMM Strategies are grounded in a human rights approach to maternal and newborn health and focus on eliminating the inequities that lead to disparities in access, quality and outcomes of health care within and among countries [5]. There has been significant progress globally in reducing maternal mortality since 2000. The UN inter-agency estimated a 38% decline in the global maternal mortality ratio from 342 deaths to 211 deaths per 100,000 live births between 2000 and 2017. Sub-Saharan Africa achieved a substantial reduction of 39 per cent of maternal mortality during this period [6]. The maternal mortality estimate from the KDHS 2014 was 362 compared to the previous KDHS (2008-09) estimate of 520 maternal deaths per 100,000 live births [1]. The government of Kenya made significant and purposeful efforts geared toward improving the lives of women in June of 2013 by declaring maternity services free of charge in all public health institutions across the country [7]. There is no formal policy document on the Free Maternity Services Policy; however, the national government has issued circulars to county governments and healthcare facilities outlining central aspects of the policy. This move makes access to quality maternal health care possible for all women in the country.Access is the ability of a person or community to receive health care services. It defines the capacity, and factors influencing entry into, or use of the health care system [8]. Furthermore, it implies that health care services are unrestricted by geographic, economic, social, cultural, organizational, or linguistic barriers [9]. It has five dimensions including, availability, accessibility, affordability, adequacy and appropriateness [8]. Availability indicates how well the defined health services meet the needs of the clients/target population [10]. Accessibility implies the location of the supply of services concerning the location of the clients. Geographical access is determined by the distribution of facilities, public transport, referral systems, sufficient community health services and degree of collaborations with other services providers [11]. The WHO recommends an average distance of five kilometers to reach the nearest health facility. It is measured by modes of transportation, distance, travel time, and any other physical barriers that could keep the client from receiving care [12]. Appropriateness denotes the fit between services and clients need, its timeliness, the amount of care spent in assessing health problems and determining the correct treatment and the technical and interpersonal quality of the services provided [8]. Adequacy is concerned with how well the organization of health care meets the expectations of the clients [13]. Affordability refers to how well the price of services fits the clients’ income, and ability to pay. Economic barriers to access include user fees, low household income, low prioritization of health at the household level and inadequate allocation of resources by the state to the health sector [14]. The Abuja declaration recommends governments to allocate 15% of the expenditure budget to health [15]. Kenya participated in and committed to the 2001 Abuja Declaration, pledging to commit at least 15% of the national budget to health care. However, the level of spending in public health remains below the Abuja Declaration threshold of 15% of the total national expenditure [16]. Moreover, Kenya signed the Maputo Protocol on the Rights of Women of 2003, which recognizes reproductive rights and commits state parties to establishing and strengthening existing pre-natal, delivery, and post-natal health and nutritional services for women [17]. As a member of the African Union, Kenya launched the Campaign on Accelerated Reduction of Maternal Mortality in Africa (CARMMA) in November 2010, reiterating the Campaign’s slogan that “no women should die while giving life” [18].The WHO definition of quality of care is “the extent to which health care services provided to individuals and patient populations improve desired health outcomes. In order to achieve this, health care must be safe, effective, timely, efficient, equitable and people-centered” [19]. It comprises the dimensions of input, process and outcome of care. Each aspect requires equal emphasis for holistic improvement in QoC [20]. The WHO developed a framework with eight overarching standards for improving the quality of maternal and newborn care. These standards describe the requirements for high-quality care around the time of childbirth and include 31 quality statements which are then organized into 352 quality measures according to the three categories of input, process, and outcomes [21]. See figure 1 below
 | Figure 1. WHO framework for the quality of maternal and newborn health care [22] |
2. Methods
- The study analyzed data on maternal death and facility-based deliveries. Data was extracted from the Kenya Health Information System (KHIS) accessible at https://hiskenya.org/. KHIS is an online health information system (HIS) powered by DHIS2. DHIS2 is an open-source, web-based software platform for data collection, management, and analysis. All the Kenyan districts and selected health facilities involved are connected to DHIS2 national server using Mobile Internet on computers. DHIS2 improves the Kenyan national health system's data analysis capabilities through an extensive facility survey conducted using the WHO SARA tool and customized through the DHIS2 Tracker. We looked at data for 8 years (2012 to 2019), for the 47 counties. Descriptive analysis was adopted complemented with univariate and bivariate analysis. Tables and figures. were used to present our findings.
3. Findings
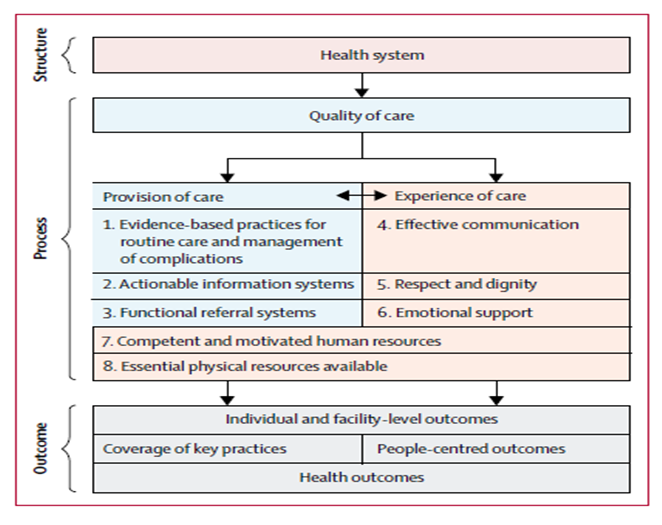
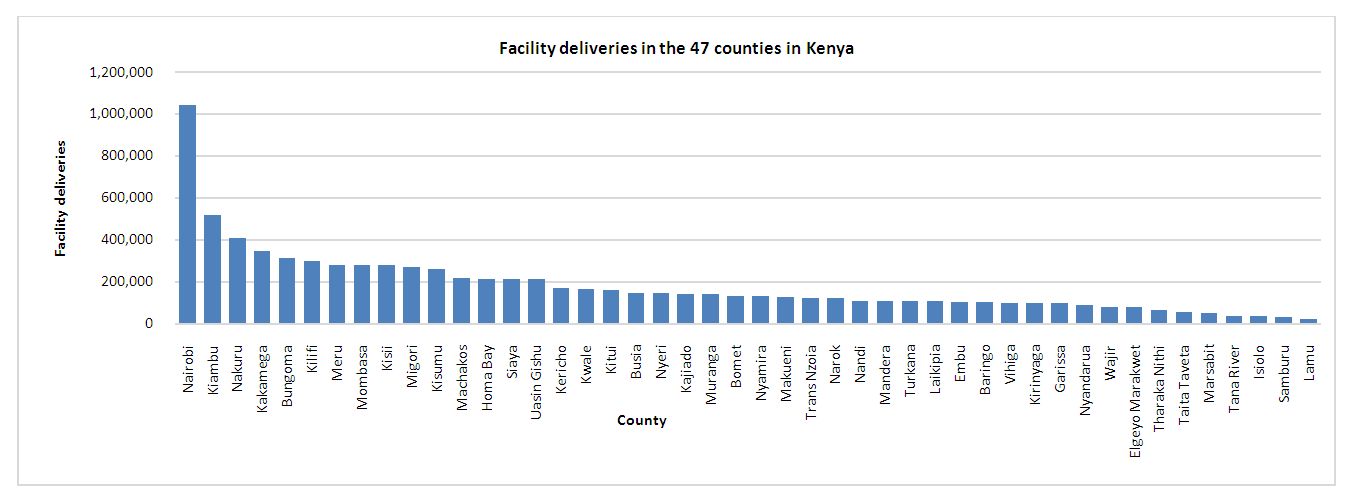
3.1. Comparison of Health Facility Deliveries and Maternal Mortalities
- The results of this study show increased access to facility-based maternity services, measured by the increased number of facility deliveries over the review period. Maternal mortality is still high, despite the increases in facility deliveries. Moreover, the facility deliveries and maternal mortality across the 8 years follow the same trend since increased mortality follows increased facility deliveries and vice versa. The extent to which facility delivery translates into mortality decline crucially depends on the quality of care provided. These findings suggest low provider skills and limited facility capability of providing good-quality routine and emergency care at birth point thus minimizing the opportunity for health gains for mothers. Furthermore, these findings suggest adverse selection that may lead to confounding. Women with complications in pregnancy or during childbirth are more likely to seek care at health facilities, and also more likely to die. See Table 1 below.
|
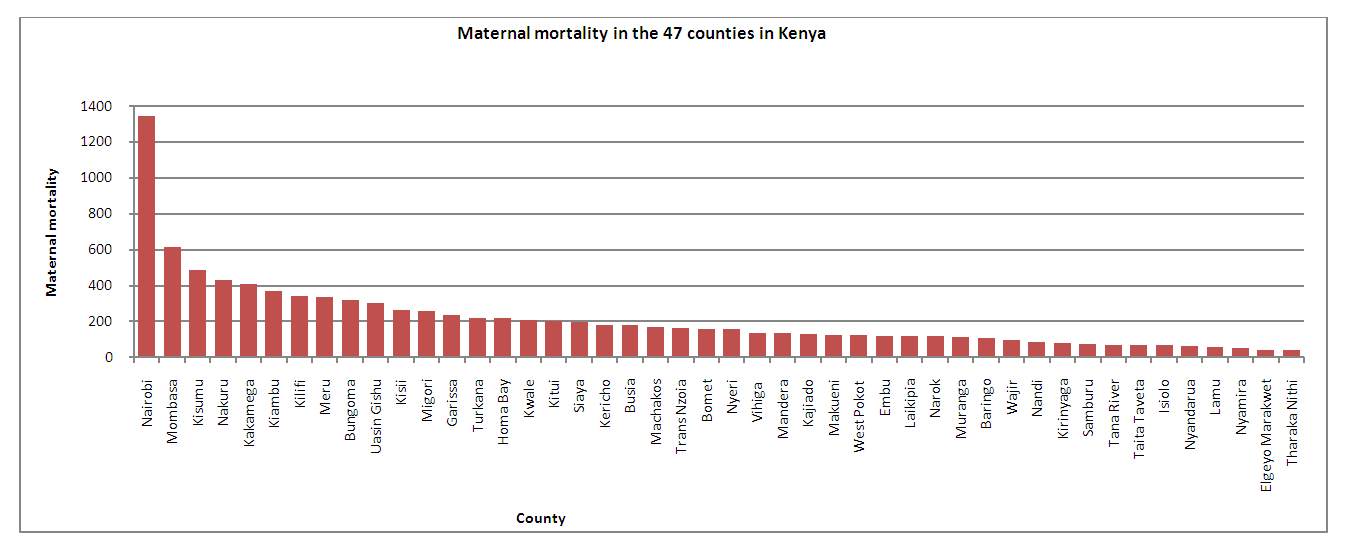 | Figure 2. Maternal mortality in the 47 counties in Kenya |
 | Figure 3. Facility deliveries in the 47 counties in Kenya |
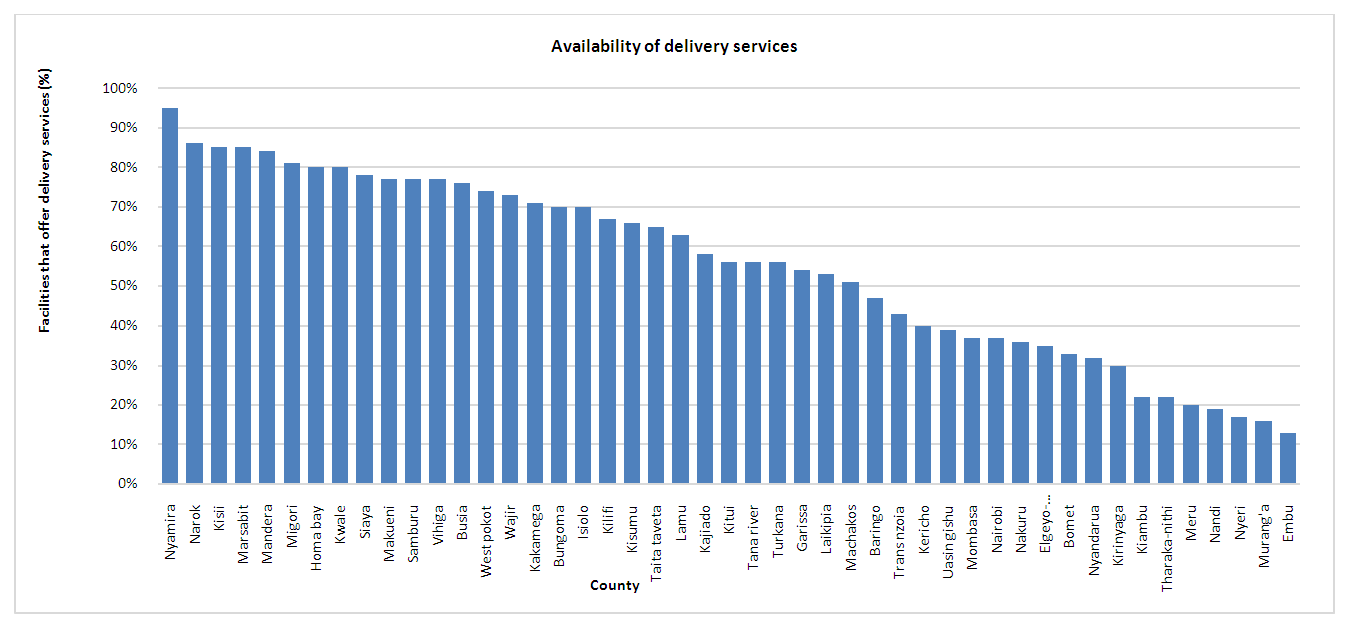 | Figure 4. Availability of delivery services |
3.2. Trend of Maternal Mortality by Age in Kenya
- There is a variation in maternal mortality among adolescents (7.33%) and women older than 20 years (92.67%). This difference could potentially be caused by data limitations since we only report findings for the adolescents during 2016 to 2019 review period. This difference also suggests a reduction in adolescent pregnancies. However, these findings should not divert focus away from efforts to reduce adolescent pregnancy, which are central to the promotion of women's educational, social, and economic development. See figure 5 below.
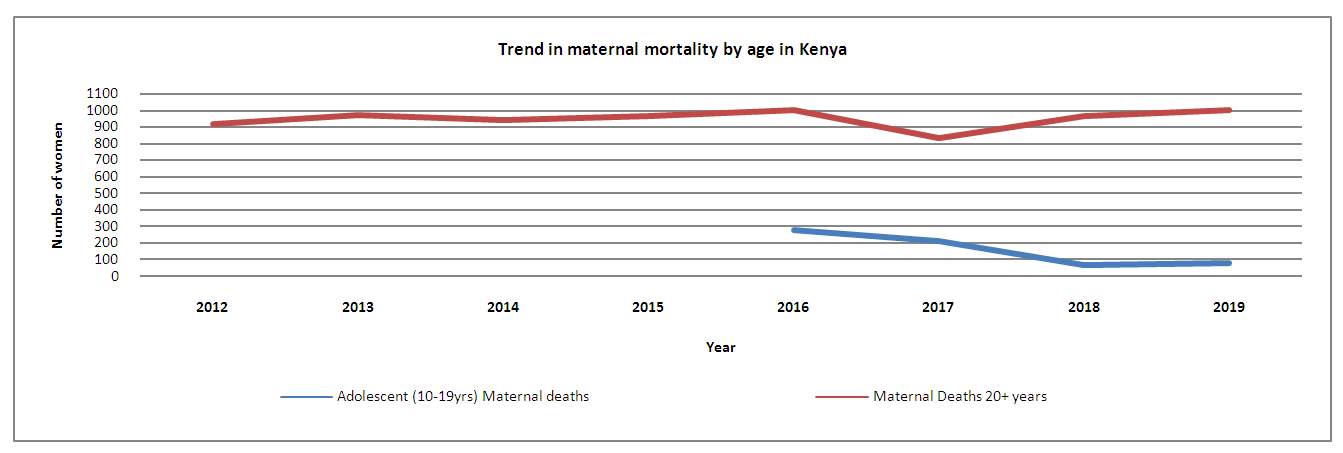 | Figure 5. 8 year trend of maternal mortalities in Kenya |
3.3. Quality of Maternity Services
- Among the 47 counties, only seven counties were ready to provide the complete range of BMONC service while 40 counties did not have adequate capacity to offer the BMONC services. See figure 6 below. The wide variation observed in performance across counties suggests the need for individualized approaches to improving care based on identified gaps. This also points to the need for advocacy for a complete BMONC system by availing all the essential equipment, drugs and supplies and replenishing it with frequent inductions, training or seminars to sustain knowledge and competencies.
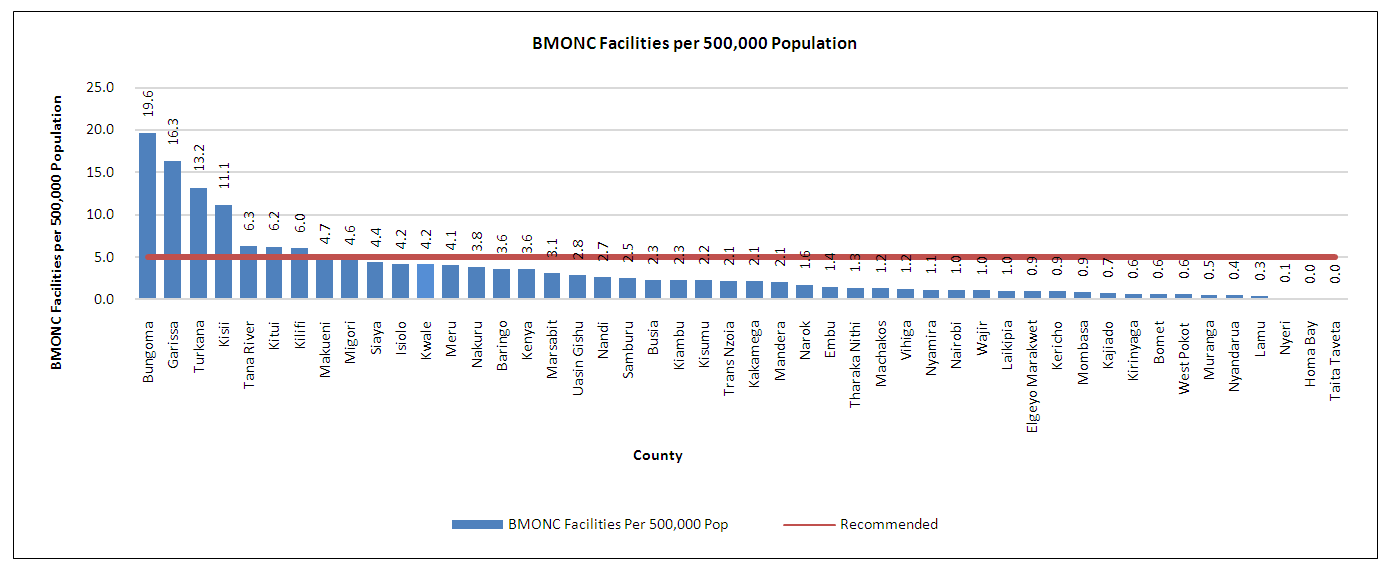 | Figure 6. BMONC Facilities per 500,000 population |
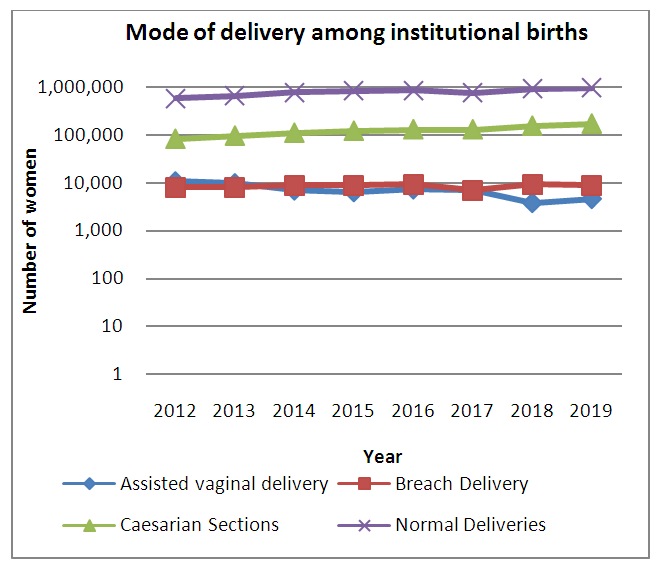 | Figure 7. Mode of delivery among institutional births |
4. Discussion
- The findings of this study show a mismatch between high coverage of facility deliveries and maternal mortality in the 47 counties. Although access to institutional care has increased, it is still poor for a substantial proportion of women and many avoidable deaths occur within health-care institutions or despite the presence of a skilled birth attendant. These findings are consistent with the findings of a mixed methods process evaluation of the free maternity policy in Kenya which showed that the rapid increase in facility deliveries was not matched by an increase in health facility capacity and hence compromised quality of care [26]. WHO/UNICEF/UNFPA/AMDD (2009) recommendation is to have at least five basic emergency obstetric care facilities (including one comprehensive facility) for every 500,000 population. In the present study, the level of provision for the signal functions was below the UN-recommended acceptable level [23] in 40 counties and is consistent with the finding of the following studies [27,28,29]. This can be attributed to increased demand due to the free maternity policy that created supply side constraints, which exposed health facilities in Kenya to financial constraints, and compromised service provision. While the policy also intended to address supply side factors like expansion of infrastructure, availability of qualified and skilled human resource for health and provision of essential commodities, it initially implemented the user fee removal due to political pressure to have the policy rolled out as soon as possible. The supply side capacity challenges were to be addressed later [26]. As such, it is not clear which investments have been made at the county level to close the supply side gaps. With most deliveries taking place in public primary hospitals, the need to ensure continued availability of BEmONC and CEmONC services will go a long way to improving maternal and new born outcomes. More investments in interventions that increase the number of available BEmONC and CEmONC facilities in the counties are required. There is need to further interrogate why there has been no significant reduction in maternal mortality across the 8 year review period, despite the availability and utilization of free maternity services in the counties. On the contrary, the cesarean delivery rate (13%), which is a strong indicator of the accessibility and utilization of EmNOC services, and for identifying gaps in obstetric care was above the UN-recommended minimum of 5% [23]. This finding is comparable with data available from the District Health Information Software (DHIS) which shows that the Kenya national cesarean delivery rate was 14.4% [30].Despite data limitations, the maternal mortality was consistently low among adolescents compared to women older than 20 years. This is can be linked to the finding of a recent study in Kenya which showed that Maternal Health Service utilization rates amongst Kenyan adolescent mothers were 93%, 65%, 92% for ante-natal care, skilled birth attendance and post natal care respectively [31]. This suggests increased access to adolescent friendly reproductive health services. Reproductive health care, including family planning services, can help women including adolescents, to prevent unintended pregnancy, complications during pregnancy and delivery, and unsafe abortion [32]. However, a recent analysis by WHO in 29 countries, showed that adolescent mothers aged 10–19 years had higher risks than mothers aged 20–24 years of eclampsia, puerperal endometritis, systemic infections, low birth weight, preterm delivery, and severe neonatal conditions [33]. Context varies therefore improved understanding of the causes of adolescent maternal death is essential to conceptualize targeted strategies for reducing adolescent mortality rates in Kenya.Finally, the greatest challenge to reducing maternal deaths in Kenya lies within the counties. The present study highlights variations in utilization and maternal mortality across the 47 counties. There is a need to collect county-specific data since the lack of quality data on maternal health undermine planning and response to maternal health issues. Context-specific analysis is critical in coming up with targeted interventions to increased utilization and reduce maternal mortality. This must be resolved in light of the increasing devolution of health services to the county level. Moreover, improvement in the collection and analysis of vital registration data is required to provide accurate estimates of data on maternal deaths and monitor health trends.
5. Conclusions
- This study shows that increasing facility deliveries does not translate into reduced mortality unless the quality of care is assured. It also highlights variations across counties on readiness to provide quality services that are likely to reduce maternal mortality. The need to improve local priority setting and decision making to improve quality, and reduce maternal mortality is strongly recommended.
6. Study Limitations
- The findings of this study do not differentiate the specific contributions of the public, private and NGOs sectors. This makes it difficult to assess quality of care for the different sectors, identify sector specific gaps and come up with creative and targeted intervention to improve utilization and reduce maternal mortality.
7. Recommendations
- While Kenya has made great strides in improving utilization of maternity services, there is need to strengthen the capacity of the supply side through sustainable financing, strengthen institutional capacity for delivery of quality RMNCAH services, build strong leadership and a coherent institutional response, leverage changes in public policy and build a knowledge base and monitoring progress.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML