-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2020; 10(2): 64-70
doi:10.5923/j.phr.20201002.04

Assessment of Naso-Gastric Feeding Able to Prevent Aspiration in Pneumonia
Md. Shahariar Khan 1, Tania Hussain 1, Basir Uddin 1, Syed Moosa M. A. Quaium 2, Yahyia Tanjil 3, Md. Rahimullah Miah 4
1Assistant Professor, Department of Paediatrics, Northeast Medical College & Hospital, Sylhet, Bangladesh
2Professor, Department of Paediatrics, Northeast Medical College & Hospital, Sylhet, Bangladesh
3Intern Doctor, Northeast Medical College & Hospital, Sylhet, Bangladesh
4Head, Department of Information Technology in Health, Northeast Medical College & Hospital Pvt. Ltd, Sylhet, Bangladesh
Correspondence to: Md. Shahariar Khan , Assistant Professor, Department of Paediatrics, Northeast Medical College & Hospital, Sylhet, Bangladesh.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: In case of patient with Pneumonia with respiratory distress, it is better to give NG (Nasogastric) feeding to prevent aspiration. But if NG feeding is not given there will be more chance to develop aspiration. So, the objective of this study is to evaluate the outcome of NG feeding to prevent aspiration in pneumonia with respiratory distress admitted in hospital. Methodology: This was a prospective observational study conducted in the department of Paediatrics in Medical College hospital over a period of six months. Hundred cases of Pneumonia with respiratory distress were included and data were collected in respect to history, examinations and diagnosis. Results: Out of the 70 cases on feeding by NG tube, about 85% of patients were rapidly improved within 2 to 4 days, 9% of patients were improved gradually within 4 to 6 days, and about 6% of patients were deteriorated within 1 to 3 days due to oral feeding in spite of having NG tube due to aspiration. Among the rest of the 30 cases, which were not given by NG tube feeding due to party refusal, out of them 20% of patients were died within few days, 26 % of patients were referred to Paediatric intensive care unit within 3 days and 34% patients were delayed improved within 5 to 7 days due to aspiration. The remaining 20% of patients were improved as usually within 3 to 5 days. Conclusion: In case of pneumonia with respiratory distress, starting NG (Nasogastric) feeding is better to avoid aspiration and give good outcome. The study explored for future research trajectories for improvement of physical condition in children with pneumonia within very few days.
Keywords: Pneumonia, Respiratory distress, Aspiration, NG feeding
Cite this paper: Md. Shahariar Khan , Tania Hussain , Basir Uddin , Syed Moosa M. A. Quaium , Yahyia Tanjil , Md. Rahimullah Miah , Assessment of Naso-Gastric Feeding Able to Prevent Aspiration in Pneumonia, Public Health Research, Vol. 10 No. 2, 2020, pp. 64-70. doi: 10.5923/j.phr.20201002.04.
Article Outline
1. Introduction
- Pneumonia is an acute inflammation in lung parenchyma [1], which is the leading infectious causes of death among children of under-five years’ old [1;2].About the 16% of deaths of children under this age occurred in pneumonia. Out of deaths, most of them were under two years old [2]. Annual child deaths from pneumonia decreased by 47% from 2000 to 2015, from 1.7 million to 922,000 million globally [2]. Tremendous improvement in child survival has been made over the past 20 years [17]. In Bangladesh, between 1990 and 2011, under 5 mortality decreased from 151 to 53 per 1000 live births (LBs). The infant mortality rate fell less rapidly from 87/1000 to 43/1000 LBs over the last 18 years. Mortality declines are associated with improved coverage of effective interventions to prevent or treat the most important causes of child mortality and with improvements in socioeconomic conditions. Pneumonia is responsible for around 28% of the deaths of children under five years of age, which are around about 50,000 each year. An estimated 80,000 children under five years are admitted to hospital with virus-associated acute respiratory illness each year; the total number of infections is likely to be much higher [2]. It can be caused by a wide range of bacteria, viruses and also seldom fungal and parasite infections [2]. The most common bacterial causes of pneumonia include Streptococcus pneumoniae Louis, Haemophilus influenzae Richard and Staphylococcus aureus Ogston [2]. Major symptoms include fever, cough and dyspnea [3]. Mainly cough is productive in older children and dry in infants and young children [3]. Moreover, dyspnea may vary from mild to severe fever from low to high grade in nature [3]. Pneumonia may manifest as upper abdominal pain when lower lobe infection irritates the diaphragm [3]. Gastro-Intestinal symptoms like nausea, vomiting, and diarrhea are also common [3]. Symptoms become variable at the extremes of age [3]. Infection in infants may manifest as nonspecific irritability and restlessness [3]. Signs include fever, tachypnea, tachycardia, crackles, bronchial breath sounds [3]. In Bangladesh, co-morbidity of pneumonia and malnutrition is prevalent and frequently associated with death. This disease accounts for approximately 15% of 1,19,000 deaths among Bangladeshi children aged less than five years [4]. In Bangladesh, 36% of children aged less than five years are malnourished and 12% of them have severe acute malnutrition [4]. The Two-thirds of the malnourished children admitted to hospital are diagnosed with pneumonia [4]. which is crucial to target malnourished children with pneumonia with the highest risk of death to have a significant impact on global child mortality through proper pneumonia case management [4].The most common viral causes of pneumonia include influenza viruses, respiratory syncytial virus (RSV) and para-influenza viruses; viral infections are particularly common in children [4]. Sometimes the types and severity of illness are influenced by several factors including age, season of the year, immune status of the host and environmental factor such as overcrowding [4]. It can occur recurrently or may be persisted more than 1 month [4]. Antibiotics are not necessary in treatment of viral pneumonia and most of the cases require supportive and symptomatic treatment [4]. Bacterial Pneumonia caused by common bacteria can be prevented by vaccination and also by exclusive breast feeding and proper weaning it can be reduced [4]. The World Health Organizations recommended low-cost alternative treatment for severe pneumonia - low-flow oxygen - still results in one in seven children death. The International Centre for Diarrhoeal Disease Research, Bangladesh (ICDDRB), and started work on a simpler, cheaper bubble CPAP device like discarded shampoo bottle [5].The new innovative method conducted by ICDDRB arranging or modifying the outdoor facility or primary healthcare facility with small investment in pediatric beds, tools for measuring the vital signs of severe pneumonia, suction of nasopharyngeal aspirates, blood oxygen saturation measurement, oxygen cylinders, antibiotics, feeding the patient and twice-a-day follow-up by nurses or other health care providers [6]. Careful monitoring of patients and on call service should also be in place [6]. Aspiration pneumonia is a type of lung infection that is due to a relatively large amount of material from the stomach or mouth entering the lungs [7]. Signs and symptoms often include fever and cough of relatively rapid onset [8]. Complications may include lung abscess [8].Aspiration implies to inflow of materials from oral cavity or upper gastrointestinal tract into the lungs via larynx [25]. Moreover, aspiration pneumonia is an important cause of morbidity and mortality in children. It occurs mainly due to oral feeding in case of pneumonia with respiratory distress. Some include chemical induced inflammation of the lungs as a subtype, which occurs from acidic but non-infectious stomach contents entering the lungs [8]. Aspiration pneumonia preferentially affects children with medical complexity and, as such, accounts for longer and more costly hospitalizations and higher rates of ICU admission and readmission rates [9]. Treatment is typically with antibiotics such as clindamycin, meropenem, ampicillin/sulbactam, or moxifloxacin [8].Nasogastric feeding is a fine feeding tube, which is set up through the nose to the stomach [26]. It is indicated to put liquid foods, fluids and medications accomplish with nutrients into stomach directly, who are not able to eat or drink sufficient amounts orally due to swallowing problems, poor appetite etc. [24]. It is a safe procedure.The study assessed the collected quality data for diagnostic accuracy, missing data, naso-gastric feeding and feasible causes of death [16]. The aim of this study is to evaluate the prevention of aspiration in case of pneumonia and respiratory distress by giving NG (Nasogastric) feeding in children.
2. Methodology
- This was a prospective observational study conducted in the department of Paediatrics in Northeast Medical College Hospital (NEMCH), Sylhet between the months of March to August, 2019 over a period of six months. Sample size was hundred (100) in number.Data CollectionPrimary data collected from the NEMCH in Bangladesh pertaining on pneumonia in children from the existing ward. Meanwhile secondary data were collected from diverse sources like ICDDRB, NEMCH central library, Journals, daily news, books, different web pages and relevant update sources.Informal Discussion Informal discussion is integrated with the patient’s guardian like father, mother, grandmother, aunt, uncle etc. at Northeast Medical College Hospital. Some hospital data were collected through informal counseling with them to observe patient’s complication/ major problems. This discussion method was also used to be aware with them to recover from the pneumonia and aspiration.Selection CriteriaInclusion criteriaAge group range between 2 months to 2 years, pneumonia, respiratory distress, cough and cold, chest in drawing, fever, cyanosis, wheeze, lethargy, unable to feed or vomits everything, SpO2 (percentage of oxygen carrying hemoglobin in blood) < 90% without 02.Exclusion criteriaPneumonia and congenital heart disease, urinary tract infection, meningitis, severe acute malnutrition, febrile convulsion, recurrent wheeze, congenital anomalies. Total 100 patients were selected and careful history, thorough physical examinations, and diagnosis were performed. Among 100 patients NG feeding was given in 70 patients and rest 30 patients were not given by NG (Nasogastric) feeding. Data CompilationAll general information regarding pneumonia, after aspiration, its history, clinical examination, investigation, diagnosis, management and follow up data were compiled according to research objective. Data Analysis and InterpretationCompiled data were integrated for analysis and interpretation as findings using standard data analysis software like SPSS version 26, MS Excel 2016 and R programming version 3.5.
3. Results
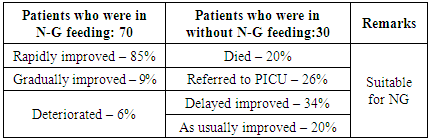
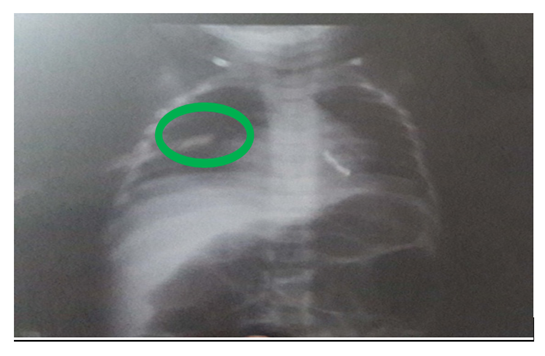
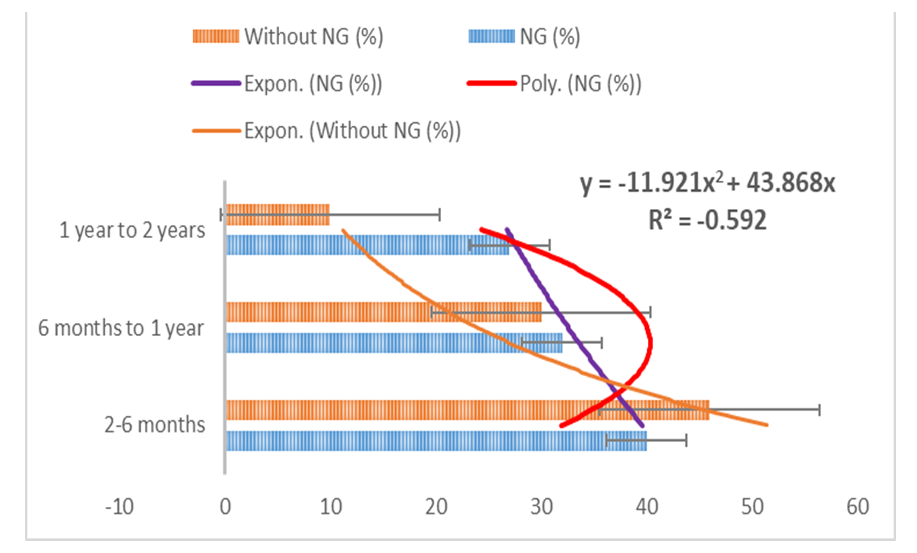
- During this study, hundred patients were included at Northeast Medical College Hospital. Cases were noted in respect to history, clinical examinations & investigations. The results were analyzed as follows:Among them 70 cases who were given feeding by NG tube, out of them 85% of patients were rapidly improved within 2 to 4 days, 9% of patients were improved gradually within 4 to 6 days, 6% of patients were deteriorated within 1 to 3 days due to oral feeding in spite of having NG tube due to aspiration. Among rest 30 cases, which were not given by NG tube feeding due to party refusal, out of them 20% of patients were died within 3 days & 26% of patients were referred to Pediatric intensive care unit within 3 days & 34 percent patients were delayed improved within 5 to 7 days due to aspiration. The rest 20% of patients were improved as usually within 3 to 5 days, which are shown in Figure 1 to Figure 4.
 | Figure 1. A case of pneumonia before aspiration, patchy opacity in middle part of right lung |
 | Figure 2. Same of above case of after aspiration, radio opaque shadow in upper part of right lung |
 | Figure 3. Distribution of patients in different age and sex group |
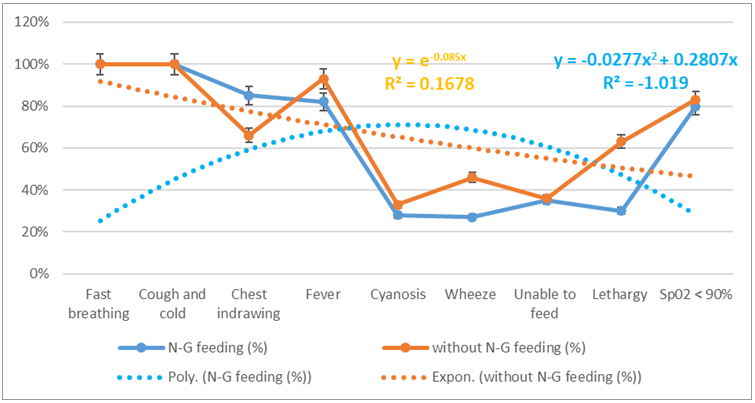 | Figure 4. Distribution of patients in different clinical presentation |
|
4. Discussion
- The study illustrated on aspiration in pneumonia with respiratory distress towards 2 months to 2 years’ children. Among them 85% of patients were rapidly improved for suitable NG feeding from our study. As a result, the study enhanced significantly reduction on child mortality and morbidity [7]. The study also observed the disease may spread via touching, sneezing, coughing and also even breathing. The occurrence happened more in the age of 2 months to 2 years. Mainly fast breathing and cough-cold are usual common manifestations in this disease. The hospital authorities arranged for isolation and quarantine of all patients and suspected cases and giving treatment accordingly. Out of hospital admitted patients, the most common case is pneumonia [22]. The common clinical presentation is fever, breathing difficulties and invasive lesions in lungs on chest x-ray [18]. Most of cases treated accordingly to take weeks to recover completely. Aspiration may arise from a case of pneumonia with breathing difficulties [7]. These difficult conditions are very much significant due to great mortality and illness. The risk factors of aspiration in pneumonia is yet unidentified [15]. The grading of aspiration depends on the type and nature of aspirated material, the frequency and the host factor of predisposition towards patients for response [14]. In addition, sometimes it may remain asymptomatic or silent [11]. Aspiration in pneumonia is a part of pneumonia field carrying same character in microbiology, pathophysiology and management [21]. Now a day’s microbiologist revealed that the lung is not germ-free, and quarantines in case of aspiration in pneumonia with aerobes and diverse culture [21]. For treatment purpose, aspiration in pneumonia should include broad spectrum coverage of antibiotic are necessary to subside the condition and manage quickly to prevent further complications. Moreover, the aiming of prevention enhanced on aspiration in pneumonia and reducing mortality and morbidity are reasonable. This depends on number and type of the aspirated materials, rate of aspiration and host responsible for events [12]. According to ALA (2020) several risks factors can increase individuals’ probabilities to getting sick and having a more severe illness, particularly aspiration in pneumonia [19]. Life-threatening problems can happen if the patient is severely compromised immune or has gone for long time without treatment. It is possible to death of children due to aspiration in pneumonia so doctors will propose the condition earlier [12;27]. The research mentioned that mortality can be reduced with the effective coverage, treatment and prevention of severe causes of child mortality according to progress in social status [20]. In Bangladesh, child mortality rate reduces within successive year, for example in 2010 the value was 49.1 but the value reduces 30.2 in 2018 [23]. According to the polynomial and exponential equations represent to downward direction gradually, which indicates to lack of awareness regarding NG or without NG feeding. If we give NG tube feeding, we can prevent aspiration as well as morbidity & mortality. The study is advised to have naso-gastric feeding with technological and psychological supports associated with effective awareness for maintenance of the nutrition, treatment and follow up in case of pneumonia to prevent aspiration. Alternatively, there are also substitute options with counselling and to prevent recurrence for setting up milestone. In some cases, those are identified difficult for NG feeding, there are few extra techniques to maintain nutrition through (i) Radiologically inserted gastrostomy tube, (ii) Percutaneous endoscopic gastrostomy. Furthermore, these methods may not be suitable in these cases, the doctor or nutritionist will assess this case and offer the most suitable method according to the required condition. The NG feeding tube should be flushed regularly before and after feed to prevent blockage [28]. NG feeding needs to supervise for advancement cautiously to ensure that the child is tolerating the feed. Before the feeding is started, remain correct placement and check the tube. A dietitian should include for adequate feeding and maintenance of proper nutrition of the child. Administration of humidified oxygen and nebulization with bronchodilator can be given. The children have to be kept in propped up position. We can prevent furthermore aspiration by inserting NG tube and gastric decomposition through suction or gravity drainage. In spite of proper treatment, aspiration in pneumonia show high mortality and morbidity. We can reduce this by limiting the risk factors and colonization of pathogenic organisms. Control Model is effective on the priority of condition or situation in connection with NG feeding. From Figure 5, the study has shown that following parameters enhance with NG feeding, such as techno-psychological supports with awareness, maintenance with nutritional support, associated with vigorous treatment and follow up counselling. On the other hand, without NG feeding, knowledge, mind set-up, motivation, doctor’s advice about follow up conditions and nutritional supports. Over all, with NG feeding is suitable for milestone-setting in case of children.
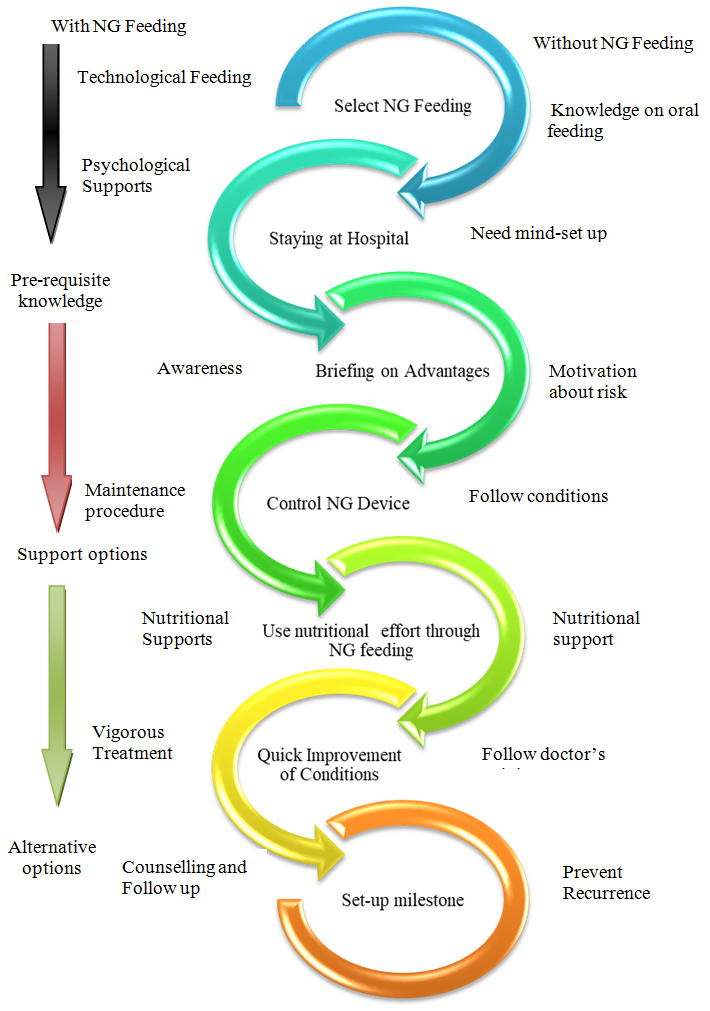 | Figure 5. A Control Model for Recovery on Aspiration in Pneumonia |
5. Conclusions
- In case of pneumonia with respiratory distress if we start NG (Nasogartric) feeding in spite of oral feeding as early as possible, we can prevent aspiration in maximum and could get better outcome. But in many cases, aspiration occurs due to refusal to give NG feeding by their guardians. So, parents counseling is very important to understand the benefits of NG feeding in that critical condition. That wise we can prevent the infant and childhood mortality in our country and correlate the existing national policy in connection with Sustainable Development Goals 2030 [29]. For this purpose, the research/ study recommends for future research trajectory.
6. Disclosure
- Data AvailabilityThe data are being used to support the findings of this research work are available from the corresponding author upon request. Competing InterestsThe authors declare no potential conflict of interests in this research work.
ACKNOWLEDGEMENTS
- The authors acknowledged the authority of NEMCH, Sylhet, Bangladesh for kind support.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML