-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2020; 10(1): 1-11
doi:10.5923/j.phr.20201001.01

The Cost-Implications of Reaching Universal Coverage of Maternity Health Services in Siaya County, Western Kenya
Oluoch Felix 1, Ayodo George 1, Owino Fredrick 2, Okuto Erick 3
1Department of Public and Community Health, School of Health Sciences, Jaramogi Oginga Odinga University of Science and Technology, Bondo, Kenya
2Department of Spatial Planning, School of Spatial Planning and Natural Resource Management, Jaramogi Oginga Odinga University of Science and Technology, Bondo, Kenya
3Department of Applied Statistics, School of Mathematics and Applied Statistics, Jaramogi Oginga Odinga University of Science and Technology, Bondo, Kenya
Correspondence to: Oluoch Felix , Department of Public and Community Health, School of Health Sciences, Jaramogi Oginga Odinga University of Science and Technology, Bondo, Kenya.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In Kenya, no studies have attempted to model alternative scenarios of the cost-implications of reaching universal coverage (i.e. 95% population coverage) of the existing maternity health services network at the ward administrative level. A cross-sectional study design used publicly available geospatial data in combination with routine data from the web-based district health information software (DHIS2) platform. AccessMod (version 5) was used for scaling up analysis. ArcGIS (version 10.5) sufficed for the preparation of geospatial input and the mapping of AccessMod results, respectively. The geographic coverage of three alternative scenarios to scale up the existing maternity health services network was tested and compared to the status quo. The findings in Siaya County confirm that even if the existing maternity health services network had unlimited capacity, almost 30% of pregnant women would still not be covered. Moreover, targeting the upgrade of hospital facility types currently working beyond their capacity would offer the best value for every additional resource allocated as compared to targeting either health centers or dispensaries, otherwise reaching universal coverage will require the construction of 32 second-tier facilities in Siaya County, as it is the most equitable approach in terms of physical accessibility to maternity health services. Future research should also consider the Lives Saved Tool (LiST) to model the effect of scaling up the geographic coverage of maternal health interventions on maternal mortality in Siaya County.
Keywords: DHIS2, Geographic information systems, Maternity services, Scaling up analysis, Travelling time, Universal coverage
Cite this paper: Oluoch Felix , Ayodo George , Owino Fredrick , Okuto Erick , The Cost-Implications of Reaching Universal Coverage of Maternity Health Services in Siaya County, Western Kenya, Public Health Research, Vol. 10 No. 1, 2020, pp. 1-11. doi: 10.5923/j.phr.20201001.01.
Article Outline
1. Introduction
- Kenya is among the countries with the highest burden of maternal deaths in the world (Keats et al., 2018). Maternal deaths in Kenya also vary markedly among its geographic regions, with the highest maternal mortality per 100,000 live births reported in North Eastern and Nyanza regions (KDHS, 2014; MoH, 2016; UNFPA, 2014). Siaya is the worst of the six counties in Nyanza region in terms of obstetric risk ratio, with an unacceptably high MMR of 691 maternal deaths per 100,000 live births, despite receiving the best ranking in terms of its overall readiness to provide maternity health services around the same period (Gok, 2014; UNFPA, 2014). According to routine health facility data from the web-based DHIS2, Siaya County also reported an estimated 66% deliveries in a health facility, despite pregnant women’s preference for health centres and hospitals as compared to dispensaries.Moreover, maternity health services in Siaya County might indeed be available but inconveniently located, therefore hindering physical access to pregnant women who will never utilize health services or do so infrequently in the predominantly rural county. Moreover, it is currently unknown whether individual facility capacities, different transportation modes (walking versus motorized) and the limited road networks, poor road quality, and diverse terrain affect the supply and demand-side barriers to universal coverage of maternity health care in this region. More importantly, global health policy experts like the World Health Organization (WHO) support the local use of existing geographic information system (GIS) tools like AccessMod (version 5.0) that incorporate the target population, availability coverage and accessibility coverage to expose hidden gaps in maternity health services provision targeting rural and marginalized populations (Ebener et al., 2015; Ebener & Stenberg, 2016a, 2016b; Munoz & Källestål, 2012; Schmitz et al., 2019). However, to date, no studies have attempted to use publicly available geospatial data in combination with routine health facility data, to design alternative scenarios able to model an increase in population coverage that would occur from specific investments aimed at increasing the number and/or capacity of maternity health services across all the 30 administrative wards in rural Siaya County. Therefore, based on current GIS best practices from literature (Ebener & Stenberg, 2016b; Ebener et al., 2019; Makanga, Schuurman, von Dadelszen, & Firoz, 2016; Schmitz et al., 2019), in combination with data on the actual capacities of existing maternity services from DHIS2, the current study was able to take into consideration the inherent inadequacies and travelling times to existing dispensaries, health centres and hospitals to model alternative, yet policy-relevant scenarios, towards a more realistic representation of the cost-implications of scaling-up maternity health services in rural Siaya County.
2. Materials and Methods
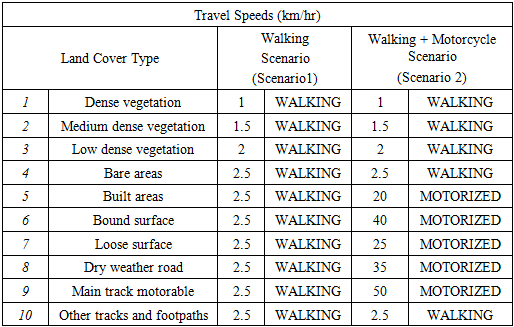
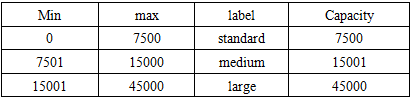
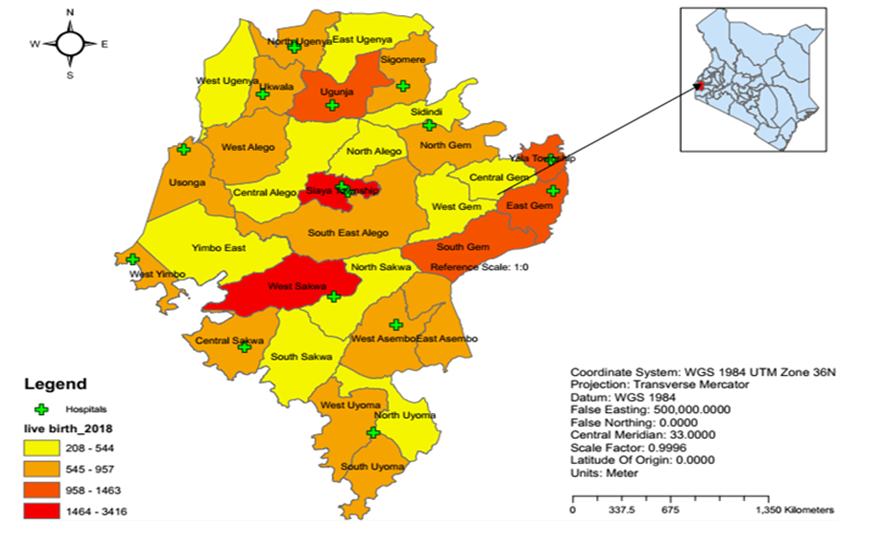
- Study AreaSiaya is one of six counties in the Nyanza region of Kenya. It has a land surface area of approximately 2,530 km2 and a water surface area of approximately 1,005 km2. It approximately lies between latitude 0° 26´ South to 0° 18´ North and longitude 33° 58´ and 34° 33´ East. The county consists of six sub-counties and thirty wards. Alego Usonga, Bondo and Gem sub-counties have six wards each; Rarieda, Ugenya and Ugunja sub-counties have five, four and three wards respectively; Alego Usonga is thus the largest sub-county with an approximate area of 605.8 km2, while Ugunja is the smallest with an approximate area of 200.9 km2 (Siaya County, 2018).The female reproductive population was estimated at 222,846, representing 22.7 per cent of the population and was projected to increase to 238,527 and 273,276 persons in 2022 and 2030, respectively. The county’s population density of 318 per square kilometre is further anticipated to increase to 415 and 476 in 2022 and 2030 respectively. In terms of the population distribution by residence, 89 per cent of Siaya County residents currently live in rural areas. As of 2017, the county had 434.2km of standard bitumen roads, 1297.41km of gravel, 532.78 km of earth and a further 1,170 narrow roads. The main development challenges include poor infrastructure, inadequate water supply, erratic electricity supply, high prevalence of HIV/AIDS and high unemployment; as a result, about 47.5% of the total population in the county currently lives below the poverty line (Siaya County, 2018).Moreover, by 2018, the number of health facilities registered in the county were 220, comprising 11 hospitals (level 4), 50 health centres (level 3) and 159 dispensaries (level 3) (S. O. Nyangueso, P. O. Hayombe, & F. O. Owino, 2018). The County’s uptake of Antenatal care and skilled Birth Attendance was higher than the national average, but it is not certain whether all the demand was met within or there was spillover to neighbouring Counties. According to the last demographic and Health Surveys (DHS), percentage of mothers receiving antenatal care from a skilled provider in the county was 98.5% as compared to 95.5% nationally (KDHS, 2014). Similarly, percentage mothers who delivered in a health facility were 66% compared Kenya’s 61.2%, yet the demand for the maternal services in 2018 was 38,972 annually, as depicted in figure 1 below (S. O. Nyangueso, P. Hayombe, & F. Owino, 2018).
 | Figure 1. Study Area |
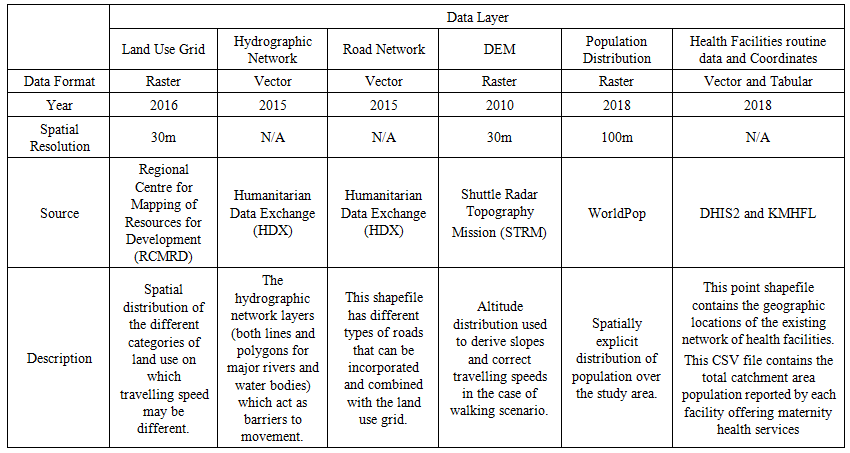 | Table 1. Characteristics of the various Input Geospatial Datasets |
|
|
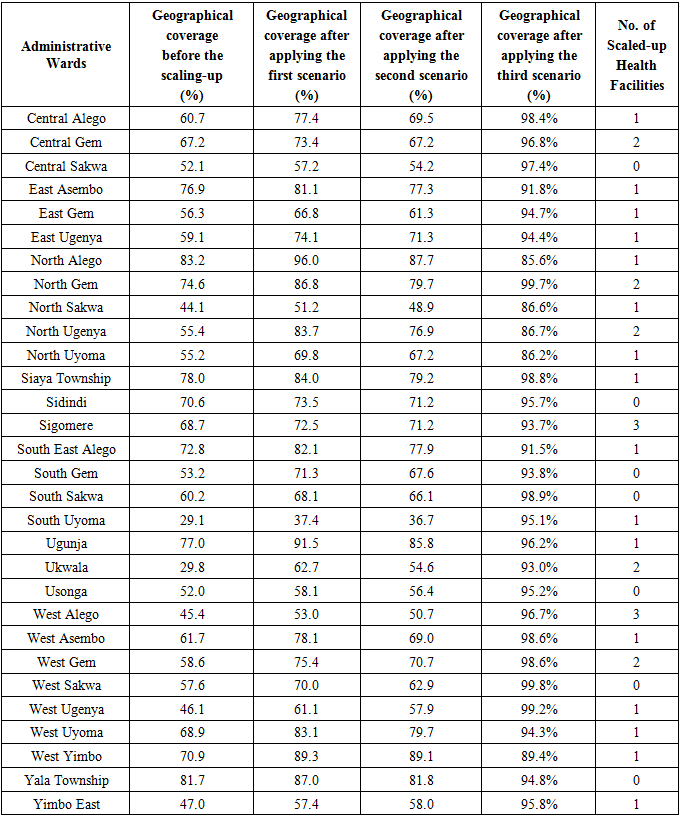
3. Results
- Summary Statistics from DHIS2: Skilled Delivery Capacity UtilizationAccording to data from the web-based DHIS2 platform, the total capacity of all health facilities for skilled deliveries across all administrative wards in Siaya County in 2018 was 39,419, yet only 25,755 (66%) of this capacity was effectively utilized, despite almost half (14/30) of the administrative wards in the county utilizing less than 50% of their estimated capacity for skilled deliveries during the same period.Moreover, in terms of total capacity by health facility type, Dispensaries represented the largest proportion at 41%, and Health Centres followed closely at 34%, despite Hospitals having 22% and Medical Clinics representing the least proportion at only 3% of the estimated skilled delivery capacity in Siaya County. Nevertheless, Hospitals utilized nearly one and a half times (149%) their estimated skilled delivery capacity and Health Centres; on the other hand, utilized 68% of their estimated capacity, despite Dispensaries and Medical Clinic facility types utilizing only 20% and 19% of their estimated capacity respectively, as illustrated in Figures 2 and 3 below.
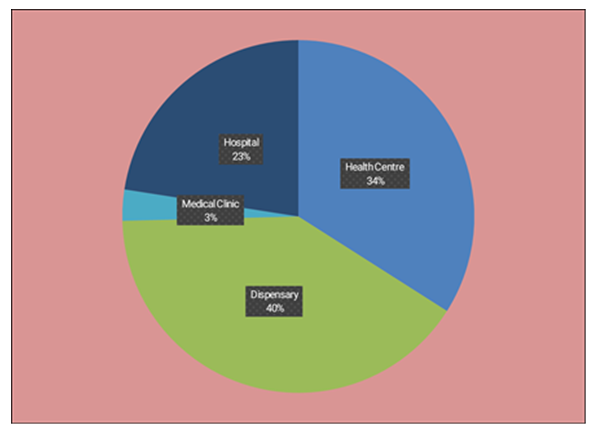 | Figure 2. Showing the estimated skilled deliveries capacity across health facility types in Siaya County |
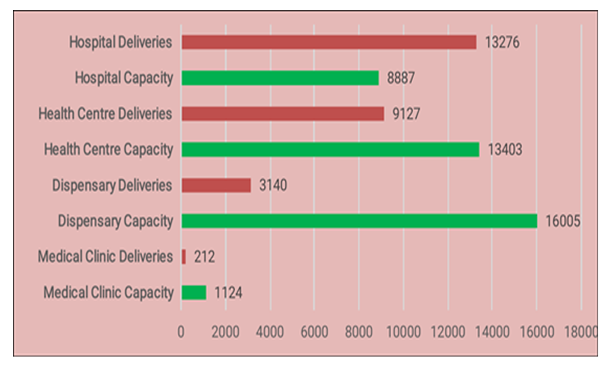 | Figure 3. Showing the total deliveries versus the skilled deliveries capacity across all facility types in Siaya County |
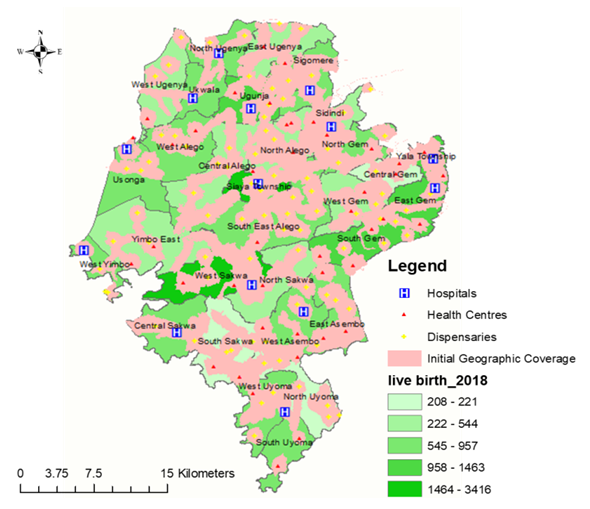 | Figure 4. Showing a map of the initial geographic coverage analysis before scaling up |
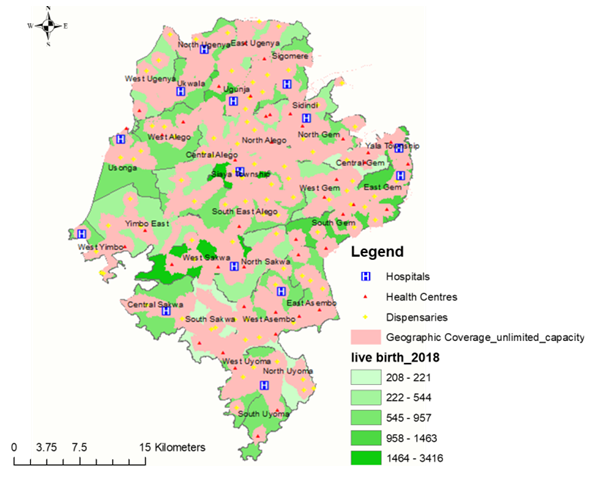 | Figure 5. Showing a map of the first scaling up scenario, when the capacities of health facilities is not a limiting factor |
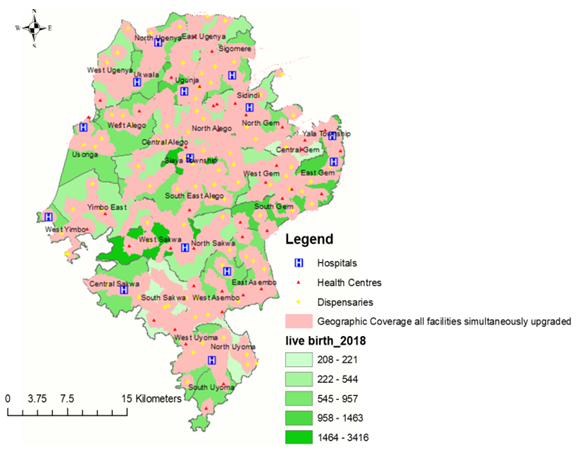 | Figure 6. Showing a map of the second scaling-up scenario when all facilities working above their capacity are simultaneously upgraded |
|
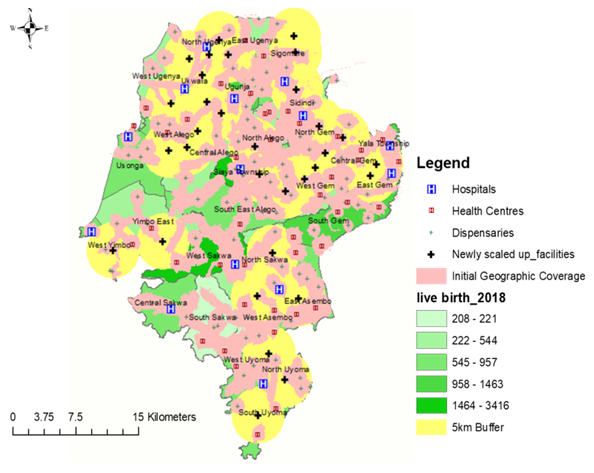 | Figure 7. Showing a map of the third scaling up scenario, with the locations and 5 km catchment buffers of the newly created facilities |
4. Discussion
- The current study succeeded in testing three scenarios designed to scale-up the maternity health services network in Siaya County, Kenya. Moreover, the results from scenario 1 and 2 confirm that neither a blanket nor a targeted upgrading of the entire network of health facilities offering free maternity health services in Siaya County will suffice to reach universal coverage. In particular, scaling up scenario 1 confirms that the major bottleneck is physical accessibility to effective coverage of maternity health services, as most facilities are working below their capacity and the situation would not improve much even if all facilities had unlimited capacity. Besides, the current situation in Siaya County seems to conform to the “inverse care law” that states that “the availability of good medical care tends to vary inversely with the need for it in the population served” (Hart, 1971). The same phenomenon has been observed in many areas of public health, including maternal and child survival strategies (Ahmed, Creanga, Gillespie, & Tsui, 2010; Dalal, Shabnam, Andrews-Chavez, Mårtensson, & Timpka, 2012; Graham, McCaw-Binns, & Munjanja, 2013; Kirkham, Stapleton, Curtis, & Thomas, 2002; Victora, 2008). Hence, in the current era of Sustainable Development Goals (SDG,s) where no one should be left behind, it is imperative to insist on progressive measures directed explicitly at poor, vulnerable or geographically marginalized populations, since alternative retrogressive paths to scaling up the existing maternity health services network may increase overall efficiency but have otherwise been explained to result in widening spatial inequalities in service coverage and associated maternal health outcomes (Ahmed et al., 2010; Choudhury & Räder, 2014; Conning & Kevane, 1999; Dugarova, 2016; Graham et al., 2013; Jaspers & Shoham, 1999; Lawn, Blencowe, Kinney, Bianchi, & Graham, 2016; Ramasundaram, 2002).Nevertheless, results from the second scaling up scenario confirm that the most significant benefit towards universal coverage of the existing maternity health services network would result form the upgrade of 8 hospitals found to be working above their capacity as compared to the 20 health centres or 56 dispensaries which would require more investment, despite resulting in diminishing returns. For example, The Lancet Commission on High-Quality Health Systems in the SDG’s Era suggests that childbirth services should be centralized to hospitals under the premise that larger volumes will result in (1) more efficient delivery care, (2) more skilful maternity providers and (3) more timely emergency care interventions including blood transfusion and caesarean section (Hanson & Schellenberg, 2019). Moreover, in sub-Saharan Africa, about 90% of the population lives within 2 hours of travel to a hospital, the present benchmark, but only 50% within 30 min, yet this number is even lower in Siaya County, Kenya (Juran et al., 2018). Therefore, Hanson et al., concludes that if we are indeed serious about leaving no one behind, significant investments are needed, both to assist poor rural women to overcome the long distance to hospitals and to build more hospitals to reduce travel time (Hanson & Schellenberg, 2019).Furthermore, scaling up scenario three confirms that in order to achieve universal coverage of the existing maternity health services network in Siaya County, more facilities will have to be built. The current decision to build 32 more facilities as compared to expanding nearby ones may seem wasteful or even inefficient at first glance, but equity often comes at a price – as does efficiency. Conventionally, in economics, equity and efficiency are often considered conflicting objectives (Davies, 1993; Jehu-Appiah et al., 2008; Kieny et al., 2017; Lindholm, Rosen, & Emmelin, 1996; Rasanathan & Diaz, 2016; Tangcharoensathien, Mills, & Palu, 2015). For instance, it may be efficient to expand more extensive facilities like hospitals currently offering maternity health services concentrated in a small number of large centres or urban areas, but more equitable in terms of physical accessibility to services to allocate more resources to construct a larger number of dispersed, smaller services like dispensaries or model health centres. In contrast, a previous World Bank sanctioned paper on Improving the Delivery of Health Services further explains that performance improvements at the system level and the facility level may be both imperative, and indeed interdependent (Berman, Pallas, Smith, Curry, & Bradley, 2011). System-level initiatives alone are explained to be too blunt an instrument often to improve service delivery across diverse organizations since they also depend a great deal on the desired response by individual facilities and organizations. The same paper also points out that without interventions directed at performance within individual facilities, broader policy reforms may not achieve their full impact, since interventions at the facility level cannot have a substantial and sustained impact on health outcomes if they are not reinforced by efforts that address the entire mix of delivery organizations (Berman et al., 2011). For example, a previous study on targeting health facility-based programs clarified that areas with low accessibility ratios could signify a need for increasing the number of facilities offering the service of interest. It also pointed out that it is worth upgrading existing health facilities that are not currently offering the service of interest, rather than investing in entirely new facilities (Colston & Burgert, 2014).Hence, in line with recommendations from the Maternal Health Task Force (MHTF), increasing access to and utilization of health care services, Siaya County is not sufficient for improving maternal health outcomes. Five priority actions have since been recommended by the Lancet Maternal Health Series, which focuses on quality of maternal health care around the world: prioritizing quality maternal health services that respond to the local specificities of need, and meet emerging challenges; promoting equity through universal coverage of quality maternal health services, including for the most vulnerable women; increasing the resilience and strength of health systems by optimizing the health workforce, and improve facility capability; guaranteeing sustainable finances for maternal–perinatal health; and accelerating progress through evidence, advocacy, and accountability (Campbell et al., 2016; Koblinsky et al., 2016; Kruk et al., 2016; Shaw et al., 2016).
5. Limitations
- A major caveat for the current analysis, as well as for other studies using least-cost path algorithms, is the assumption of a closed system- where women do not seek services outside the study area, yet in actual sense, pregnant women living near borders likely travelled beyond the current administrative boundaries of Siaya County to seek maternity services. There were also minor limitations in terms of time discrepancies and different resolutions between the publicly available geospatial datasets, despite the omission of the few privately-owned facilities that were not offering free maternity health services. Moreover, the current study did not assess other delays related to the decision to seek care and waiting time before receiving care. Theoretically, the scaling-up analysis itself was also affected by data quality, such as incomplete road networks or inaccurate health facility coordinates, despite boat and car travel not being analysed, as the study area was restricted to mainland Siaya County, and because rural women in such a low resource setting with poor road networks, were less likely to rely on car travel.
6. Conclusions and Recommendations
- The current analysis has confirmed the feasibility of scaling up the existing maternity health services network in Siaya County. The immediate implication is that upgrading Hospital facility types would result in the most significant benefit, despite requiring the least investment as compared to dispensary and health centre facility types. Moreover, indiscriminate decisions to upgrade all facilities currently working beyond their capacity will not be enough to reach universal coverage (i.e. 95% population coverage), as such policymakers need to explore the option of constructing a larger number of dispersed, second-tier health facilities in Siaya County, as it is the most equitable approach in terms of physical accessibility to maternity health services. Future research should also consider leveraging the Lives Saved Tool (LiST) to model the effect of scaling up the geographic coverage of maternal health interventions on maternal mortality in Siaya County.
ACKNOWLEDGMENTS
- I would like to thank the Siaya County Health Department, Division of Reproductive Health and the County Health Management Team for their support.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML