-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2019; 9(4): 65-76
doi:10.5923/j.phr.20190904.01

Factors Associated with Non-Adherence to Antiretroviral Therapy among Adult Clients in a Comprehensive Care Center at a Health Center; Kiambu County, Kenya
Sammy Kithinji Kamaingi1, Lucy Wankuru Meng’anyi2
1School of Nursing, Mount Kenya University, Thika, and Ng’enda Health Center, Gatundu, Kenya
2Department of Medical Surgical Nursing, School of Nursing, Mount Kenya University, Thika, Kenya
Correspondence to: Lucy Wankuru Meng’anyi, Department of Medical Surgical Nursing, School of Nursing, Mount Kenya University, Thika, Kenya.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Non-adherence which is the leading cause of active Antiretroviral Therapy (ART) resistance among clients is basically the failure to use antiretroviral drugs as prescribed for Human Immunodeficiency Virus (HIV) by clients. Internal and external factors contribute to this. Objective: The aim of the study was to determine factors associated with Non-adherence to ART among adult HIV clients in Ng’enda Health Center, Kiambu County, Kenya. Methods: A descriptive cross-sectional study design was used. Target population was adult HIV clients seeking ART services at Ng’enda Health Center Comprehensive Care Clinic (CCC). Simple Random sampling was used and a sample size of 141 (98.6%) was achieved. A structured interview schedule was used to collect quantitative data. Data was analysed using Statistical Package for Social Science (SPSS) version 22.0 and findings presented in frequency tables, bar graphs and pie charts. Results: Fifty four percent (54.6%) of the respondents were female and 45.4% males, 36.2% had attained secondary education and 31.9% college education. Forty five percent (45.4%) had been on ART for 1 to 5 years, 70.9% had adequate knowledge on ART adherence, however 63.4% had ever failed to adhere and 51.1% had not adhered in a month prior to the study. Main reasons for non-adherence were forgetfulness (43.9%); busy work schedule (18.4%), distance/fare to the clinic (21%), long queue (25.5%), lack of family support (14.8%), and long waiting time (41.1%). Forty two percent (42.6%) of clients lacked treatment supporters and 16.3% had not disclosed their status. Only 37.6% did not receive family support. Forty percent (40.4%) experienced stigma at family level while 87.9% reported stigma existed at community level. Fifty seven percent (57.7%) of the respondents associated spiritual healing with non-adherence. Conclusion: Personal and facility factors contributing to ART non-adherence among clients were identified. The facility management team therefore needs to identify interventional programs to improve ART adherence among HIV clients. This requires collaborative efforts of all stakeholders involved in HIV prevention and control in the CCC.
Keywords: Adherence, Antiretroviral therapy, Comprehensive care center
Cite this paper: Sammy Kithinji Kamaingi, Lucy Wankuru Meng’anyi, Factors Associated with Non-Adherence to Antiretroviral Therapy among Adult Clients in a Comprehensive Care Center at a Health Center; Kiambu County, Kenya, Public Health Research, Vol. 9 No. 4, 2019, pp. 65-76. doi: 10.5923/j.phr.20190904.01.
Article Outline
1. Introduction
- Kenya AIDS Indicator Survey (KAIS) of 2012 indicated that the HIV prevalence is at 5.6% (1.4 million) among adults aged 15 to 64 years. The prevalence nevertheless has a regional variance with the highest prevalence recorded in Nyanza and the lowest prevalence recorded in North Eastern region. The report further indicated that viral suppression among Persons living with HIV/AIDs (PLWHAS) was only at 40%. Viral load suppression among those adhering to ART (75.4%) was higher i.e. ≤1,000 copies/ml than those who reported that they had missed taking their ARVs (57.9%) in the 30 days prior to the survey. In suppressing the viral load, several types of Antiretroviral (ARVs) drugs are used to manage HIV/AIDS. These ARVs act against the HIV by decreasing the viral replication and viral load in the blood. Adherent use of ARVs usually results to viral levels that are no longer detectable in usual viral load essays test. However, non-adherence to antiretroviral therapy (ART) leads to compromised immune system among PLWHAS. This usually results in increased opportunistic infections among the PLWHAS [1]. The government of Kenya for the last 10 years has been committed to improve the access to lifesaving ART services to PLWHAS by up scaling ART programs in the country. This has contributed to an increase in the number of persons on the ART program from 6,000 in 2003 to about 656,000 in 2013. However, recruitment to ART program does not guarantee client adherence to the ART which is a lifelong program for persons with HIV. Available data shows that, there is need to integrate active measures to reduce loss to follow up and non-adherence among PLWHAS for sustained viral suppression which is a critical component of ART services [2]. According to the Joint United Nations Programme on HIV and AIDS (UNAIDs), individual and public health benefits of ART are adherence dependent. Non-adherence to ART results to poor viral load suppression among HIV infected persons. Non-adherence to ART may end up in development of ARV drug-resistance thus negating the critical role played by ART in reducing HIV incidence and transmission as well as improving the health status of PLWHAS. As developing countries become more committed to improving the access to ART today, adherence is particularly important since regular viral load monitoring is not always possible among PLWHIV [3].According to World Health Organization (WHO) and Management Science for Health (MSH), 2011, a survey on ART adherence and defaulting behaviour involving 6,500 ART clients, conducted in five East African countries (Kenya, Uganda, Tanzania, Ethiopia and Rwanda) indicated a strong evidence of achieving adherence targets in these resource poor countries. However, some of the countries had a low adherence value especially for dispensing based adherence and patient attendance. The healthcare providers should therefore always investigate the factors influencing adherence in their facilities and work to achieve high level ART adherence through regular performance monitoring of ART services [4].The Ministry of Health (MoH), 2016 AIDS response report indicated a steady increase in the PLWHAS client accessing ART services in Kenya, contributing to reduced HIV/AIDS related mortality. However the ART program has a regional performance variation ranging from 2% to 99% in the country. The report therefore recognized the need for improved retention and adherence of clients on ART for maintenance of viral load suppression among PLWHAS [5].At Ng’enda Health Centre CCC, the number of the patients advancing to non-adherence to antiretroviral therapy is rising every day. Adherent records at CCC at Ng’enda Health Center showed that, 132 clients were recorded to be non-adherent in the year 2015. This number significantly increased to 196 clients in the year 2016. These clients had missed doses which were recorded through the pill count with the refill against the number of days. Some of these clients had missed the clinic appointment for the refill of the ARV treatment. Some viral loads done to non –adherence clients indicated detectable viral load of above 10,000 copies while still on ART. By the end of 2015 there were 12 clients with detectable viral load while still on ART. The number rose to 19 patients in 2016 [6].According to Byakika et al, 2011, an investigation carried out to assess non-adherence and factors associated with it in Nairobi, Kenya indicated that patients who accessed therapy in clinics within a walking distance from their homes were likely to adhere better than clients who refilled in faraway clinics. Probably this could be because they could not afford transport cost to CCC. Difficulties in accessing ART in a CCC within walking distance from home makes the clients to become non-adherence to medication because some unspecified patients may not be able to travel for long distance to access the clinic [7]. A study conducted in Zambia in 2006 revealed that, HIV positive persons showed good adherence when a client has a long standing and trusting relationship with a sole health care provider but those who had mistrusted association were non-adherent. A trusting relationship between healthcare providers and ART clients helps to make adherence among the clients better than those who do not have such relationships [8]. Some ARVs require specific food and fluid restrictions, for instance there are those that should be taken one hour before or 2 hours after meals with at least 1.5 litres of fluids to prevent formation of gallstones. This makes the clients to stop taking their ARVs or pass over some doses when they lack food either supplied by CCC or their relatives or guardians [9]. As per CCC instructions it is prudent that clients feed prior to taking ARVs. In regards to this it has been noted that clients hesitate or decline to take their medications because they develop fear of taking the medications prior to feeding [10]. HIV infections cause increased energy requirements, lowered appetite and mal- absorption. A Cross sectional investigation carried out in CCCs at Kenyatta National Hospital (KNH), Kenya Medical Research Institute (KeMRI) and Riruta Health Center on “predictors of non- adherence” indicated that clients who spent more than half a day in the clinic to refill were likely to become non-adherent to HAART than the clients who took less time in the clinic [10].Adverse side effects usually occur from virtually all antiretroviral drugs. This may result in distressing symptoms to ART clients subjecting them to non-adherence more than those without adverse side effects from ART. Prior to commencing therapy most of these clients are asymptomatic hence may stop the medications to avert the adverse effects which can be life threatening such as Stephens- Johnson Syndrome [11].Antiretroviral Therapy clients often fail to remember the right time to take their ARV drugs as scheduled. Some may even omit their drugs or take them against their prescribed time. Wakibi et al, (2011) indicated that, there are varied reasons why ART clients become non-adherent. Some say they forget their ART drugs due to busy work schedules and daily chores. Clients who are actively involved in duties of their lives are unable to keep time in taking their drugs as they are too busy attending other duties [10]. Social stigma is among the major factors that may prevent persons living with HIV from revealing their status to others and acts as a hindrance to ART adherence. Highly stigmatized HIV clients are three times more likely to non-adhere to their ART regimen than those without stigma. Katz L. et al, 2013 further argues that, the impact of HIV related stigma compromises clients’ ability to successfully adhere to ART. Therefore, there is great need to incorporate stigma reduction interventions at the community level in order to attain optimum effectiveness on ART adherence. Secondly, social and family stigmatization and fear of the consequences of revealing HIV sero-status to intimate partners are closely associated to poor family support system and non-adherence to ART among clients. The acceptance of the client’s HIV status in the family is associated with better adherence than clients who are rejected or stigmatized [12].Clients who receive support from family and friends on the use of drugs adhere more than those who do not receive any support from their families and loved ones. This support includes; transport to the CCC for drug refill, food to take with ARV therapy, and reminding them to take drugs on time. Clients whose families’ provide none or irregular support have difficulties in adhering to their therapy schedules. Support plays an important part as it is an encouragement to the client to take antiretroviral drugs as indicated. Clients who can confidently discuss their HIV status with the family adhere better than those who do not [13].
2. Methods
- A quantitative descriptive cross sectional study was conducted in the month of March 2018 where 143 respondents aged between 18-65 years who sought ART services at Ng’enda Health Center for the last six months prior to the study were recruited for study. Consent was sought from the respondents before recruitment. The sample size was calculated using the Blair E & Blair J (2015) formula. The respondents were further sampled randomly from the CCC register where pieces of papers bearing numbers corresponding with CCC client numbers as per their return dates were generated folded and shuffled in a carton. Then a casual worker in the CCC was requested to pick pieces equivalent to the sample size (143 pieces). The CCC client corresponding with the picked number was sampled to participate in the study. In the event the sampled client did not turn up or declined to participate in the study, the succeeding client in the register was sampled. Approval to conduct the study was sort from Mount Kenya University Ethics and Research Committee, the Sub County Medical Officer of Health (MOH) Gatundu, and from the Officer in-charge of Ng’enda Health Center. An interview schedule with both open and closed ended questions was used to collect quantitative data from the sampled clients. The researcher conducted face-to-face interviews with sampled CCC clients during the data collection period. A pre-test was conducted in Gatundu Level 5 hospital where 15 (10% of total sample size - 143) interview schedules were filled. Any difficulties in understanding the questions, language barrier, ambiguity, anomalies and/or gaps noted in the interview schedule were appropriately amended. The researcher was keen to ensure completeness and consistency during the interview sessions. Completed interview schedules were numbered and packed in envelopes marked with dates of the data collection day. The quantitative data was coded, entered in a computer, cleaned and analysed using Statistical Package for Social Science (SPSS) computer software Version 22.0. Descriptive analysis was done and analysed data was presented in frequency tables, bar graphs and pie charts.
3. Results
3.1. Response Rate
- The study achieved a response rate of 98.6% whereby 141 interviews were successfully conducted.
3.2. Social Demographic Characteristics of the Respondents
3.2.1. Gender of the Respondents
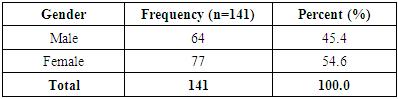
- Over half (54.6%) of the respondents were female while the rest of the respondents were male (Table 1).
|
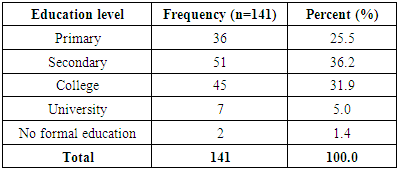
3.2.2. Level of Education
- The findings of the study showed over a third (36.2%) of the respondents had attained secondary education, while a quarter (25.5%) had a primary level of education. A small percent (1.4%) had no formal education (Table 2). This shows that majority of the people attending the health center have minimum education which is important when providing health education.
|
3.2.3. Religion of the Respondents
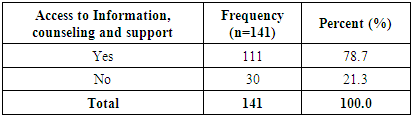
- A larger proportion (46.8%) of the respondents was Catholic believers followed by the Protestants (45.4%). A small proportion (1.4%) comprised of Muslims, while 3.5% of the respondent gave no response (Figure 1). Religion plays a big role when it comes to health seeking behaviour. People who are very cultural tend to seek care from herbalists and traditional healers. The main stream churches believe in people seeking conventional medicine. With the large proportion of this community being religious it therefore means they can readily seek medical help from the hospital.
 | Figure 1. Religion of the respondents |
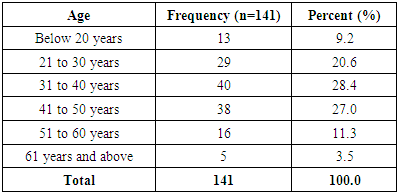
3.2.4. Age of the Respondents
- Most (28.4%) of the respondents were aged between 31 to 40 years followed by those between 41 to 50 years. Nine percent (9.2%) were below the age of 20 years while 3.5% were over 61 years. The youngest respondent was 18 years while the oldest was 64 years. The mean age (±SD) of the respondents was 36.0 (±12.08) (Table 3).
|
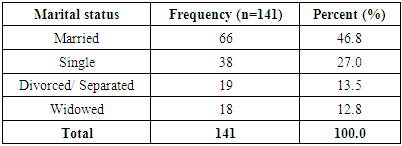
3.2.5. Marital Status
- Most (46.8%) of the respondents were married, more than a quarter (27.0%) were single while 12.8% were widowed (Table 4). A significant number of the respondents were single or widowed and it has been shown that a partner to remind the other or a family member to remind a client on when to take drugs is important in adherence to ART.
|
3.2.6. Occupation of the Respondents
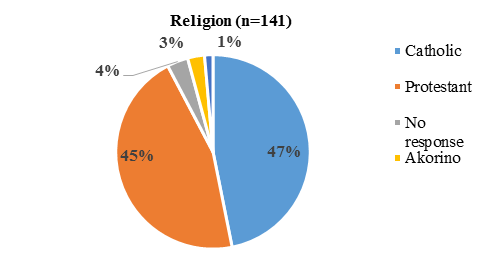
- More than a third (35.5%) of the respondents were farmers while slightly less than a quarter (24.8%) were self-employed. Almost 10.0% of the respondents were students.
 | Figure 2. Occupation if the respondents |
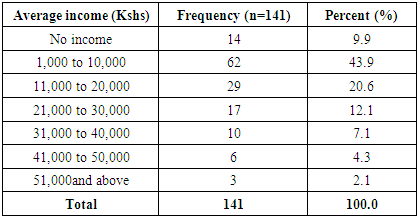
3.2.7. Average Income of the Respondents
- In this study forty three percent (43.9%) of the respondents earned between Ksh 1,000 to 10,000 shillings, while 20.6% earned between Ksh 21,000 to 30,000 shillings a month. A small proportion (2.1%) earned more than Ksh 51,000 shillings in a month (Table 5). Majority of the respondents were low income earners and a small proportion had no source of income, hence can lead to the conclusion that most of the time they cannot afford a balanced diet which is key in management of HIV.
|
4. Client Related Factors
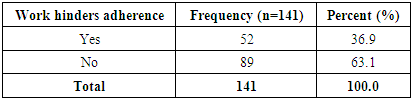
4.1. Hindrance to ART Adherence Due to Work Schedule
- Most (63.1%) of the respondents reported that their work does not hinder adherence while the rest (36.9%) said their work hindered them from adherence to ART (Table 6). This is alarming because if they do not adhere because of work then they might not be around or might not be strong enough to work in the near future. Employers should encourage their employees to disclose their status so that they can release them to go and refill drugs when over.
|
4.2. Duration on ART
- Slightly over a quarter (45.4%) of the respondents had been on ART for 1 to 5 years while 22.7% had been on ART for 5 to 10 years. A small proportion (3.5%) had been on ART for more than 15 years (Figure 3).
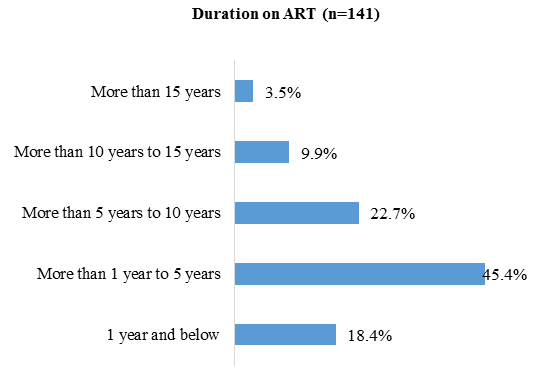 | Figure 3. Duration on ART |
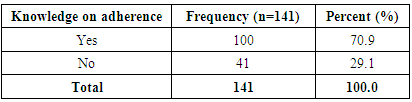
4.3. Adequate Knowledge on Adherence to ART
- Majority (70.9%) of the respondents reported they had adequate knowledge on adherence while 29.1% of them which is a notable number said they did not have adequate information (Table 7).
|
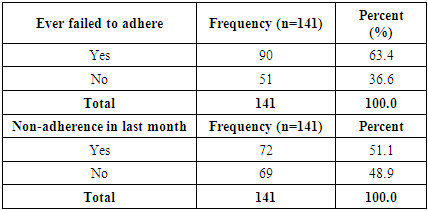
4.4. Non-adherence to ART
- Most (63.4%) of the respondents reported that they had ever failed to adhere to ART while 36.6% reported they had never failed to adhere to ART therapy. Slightly over half (51.1%) of the respondents had failed to adhere for the last one month prior to the study while the rest had not failed (Table 8). A significant number failed to adhere and it is alarming as the key to reducing the viral load is adherence.
|
4.5. Reasons Given by Respondents for Non-Adherence
- Forgetfulness was reported by most (43.9%) of the respondents as the main reason for non-adherence to ART. Busy work schedule and side effects were reported by 18.4% and 9.2% respectively. Five percent (5%) reported stigma while 4.1% reported stress as the reasons for ART non-adherence (Figure 4). This is an indication that several factors play a role in the hindrance of clients who visit this health center from adhering to ART.
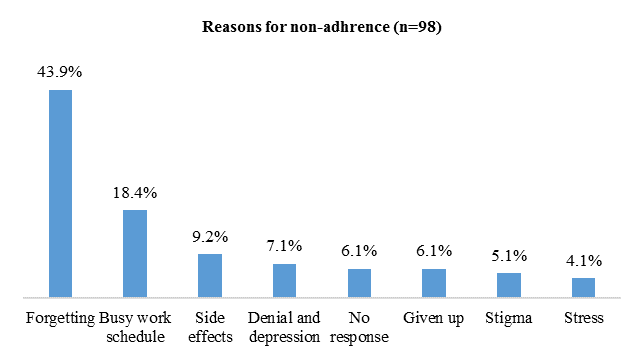 | Figure 4. Reason for non-adherence |
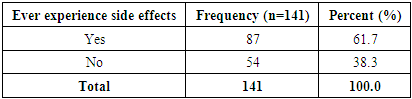
4.6. Responses on Whether the Respondents Had Ever Experienced ART Side Effects
- Most (61.7%) of the respondents reported that they had ever experienced side effects of ART (Table 9). Side effects to ARVs have been cited as one of the factors that lead to non-adherence. With most of the respondents reporting to have experienced side effects a significant number might be non-adherent as per the findings on non-adherence due to treatment.
|
4.7. Side Effects Experienced by Respondents
- Over a third (35.6%) of the respondents reported that they had experienced drowsiness, nausea, vomiting and hallucinations while 12.6% had experienced rashes and lack of appetite as a result of ART. Ten percent (10%) fatigue, hallucination and lack of appetite, while 9.2% experienced fatigue, vomiting, headache and shivering. A small proportion (3.4%) experienced swollen breast tissues, numbness of the limbs and headache (Figure 5). Most of the clients in this study reported that they earn between 1000-10,000 Kshs hence low income earners. Consequently with a significant number of these respondents reporting drowsiness, nausea, vomiting and hallucinations as side effects, it can be postulated that they might experience challenges at work.
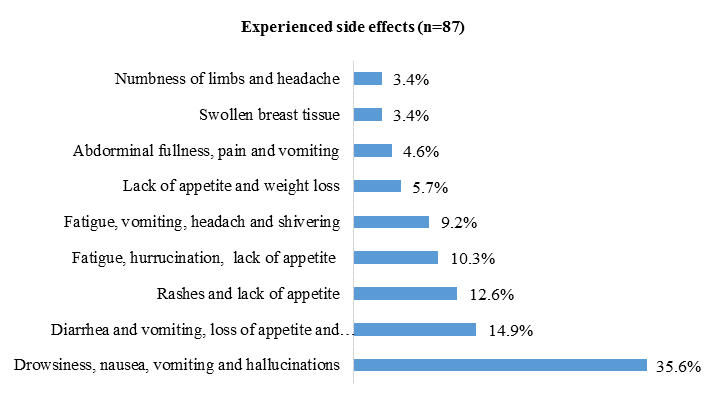 | Figure 5. Experienced side effects |
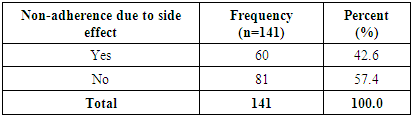
4.8. Non-Adherence due to Side Effects
- Less than a half (42.6%) of the respondents reported that they had failed to adhere to ART in the last one month prior to the study due to side effects (Table 10).
|
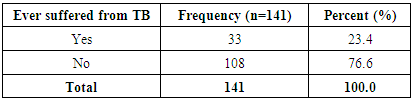
4.9. Respondents’ Responses on Whether They had ever Suffered from Tuberculosis (TB)
- Less than a quarter (23.4%) of the respondents had ever suffered from Tuberculosis while the rest had not (Table 11). Findings from studies have shown that HIV weakens the immune system hence predisposing a person to tuberculosis.
|
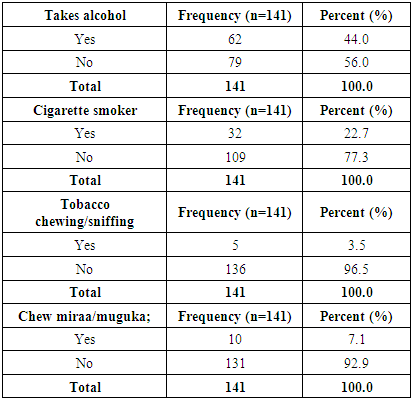
4.10. Drug and Other Substances Use
- Less than a half (44.0%) of the respondents reported taking alcohol, 22.7% smoked cigarette and 7.1% chewed miraa/ muguka (Table 12). Alcohol intake has been associated with risky behaviour when it comes to HIV. The clients can easily get drunk and forget to wear a condom during sexual intercourse hence infect others or get infected with another strain of HIV. High cases of non-adherence to ART have also been noted in clients who take alcohol in some studies.
|
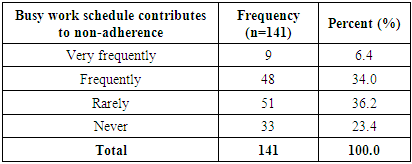
4.11. Extent of non-adherence due to Work
- Over a third (36.2%) of the respondents reported that a busy work schedule rarely contributed to ART non-adherence while 23.4% reported it never contributed to non-adherence. However, a small proportion (6.4%) reported that a busy work schedule very frequently contributed to their ART non-adherence and 34% reported it frequently contributed to non-adherence (Table 13). This is an indication that the extent of work schedule being a hindrance to ART adherence is significant as per the findings on non-adherence due to work schedule.
|
4.12. Respondents’ Social Factors
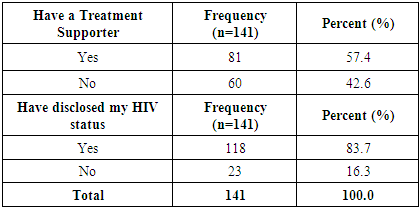
4.12.1. Treatment Supporter and HIV Status Disclosure
- Over half (57.4%) of the respondents had a treatment supporter while the rest (42.6%) did not have a treatment supporter. Majority (83.7%) of the respondents had disclosed their HIV status (Table 14).
|
4.12.2. Respondents Responses on who They have Disclosed HIV Status to
- Half (50.0%) of the respondents had disclosed their status to their wives or husbands while 31.6% had disclosed to members of their nuclear family, and 16.7% had disclosed to extended family members. Only 5.3% of the CCC clients had gone public about their HIV status. This is a positive finding as when a client doesn’t have to hide their HIV status it means that they can take the drugs freely and are not likely to infect non suspecting individuals.
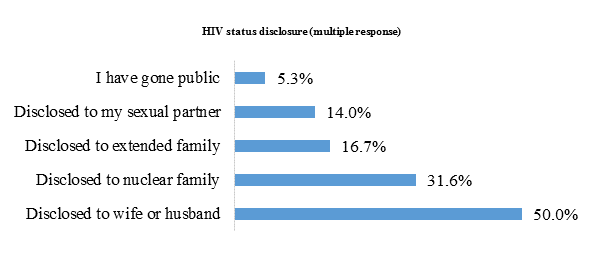 | Figure 6. Disclosure of HIV status |
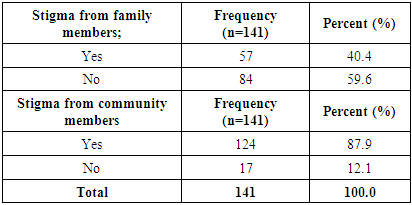
4.12.3. HIV Stigma
- Forty percent (40.4%) of the respondents reported that they were stigmatized by members of their families while the rest (59.6%) were not stigmatized. However, majority (87.9%) of the respondents reported they were stigmatized by members of the community (Table 15). Stigma plays a big role in non-adherence hence with a significant number of the respondents having been stigmatized their adherence is questionable.
|
4.12.4. Form of Stigma from Community Members
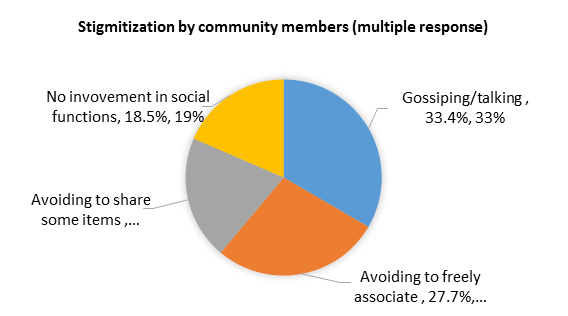 | Figure 7. Stigma by Community Members |
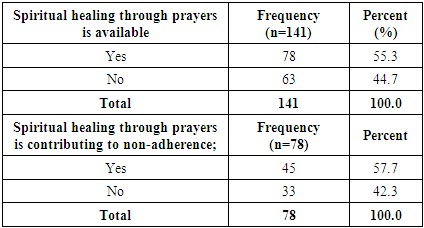
4.12.5. Availability of Spiritual Healing through Prayers
- Over half (55.3%) of the respondents reported that spiritual healing for HIV infected clients is available in the community while the rest (44.7%) reported that it did not exist. Most (57.7%) of the respondents reported spiritual healing through prayers was contributing to non-adherence among the CCC clients (Table 16).
|
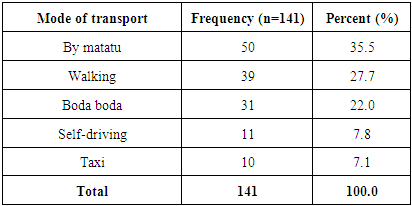
4.12.6. Mode of Transport to the Health Center
- Over a third (35.5%) of the respondents used matatu to the CCC while 27.7% walked to the CCC. A small proportion (7.1%) took a taxi to the CCC (Table 17). Walking to the CCC can contribute to non-adherence as clients can be too tired or feel lazy to do so although in this case the respondents who used matatu as a mode of transport were the majority.
|
4.12.7. Cost of Transport
- Most (47.1%) of the respondents used less than Ksh 100 while 29.4% used between Ksh 101 and 200 shillings for transport to the CCC. Almost 10% used more than Ksh 301 (Figure 6). The findings on income earned by respondents revealed that majority of them earned 1000 to 10,000 Kshs per month. If these clients are to use 101 to 301kshs for transport to the facility, there might be significant cases of non-adherence in relation to transport.
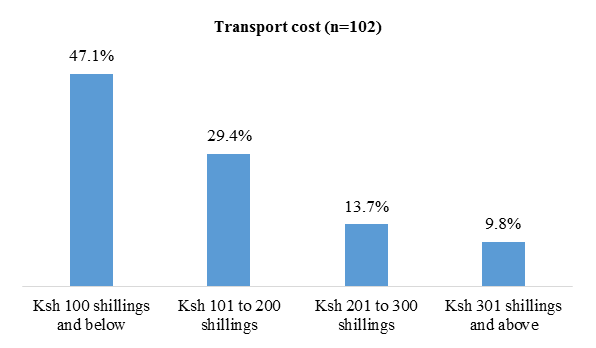 | Figure 8. Cost of transport |
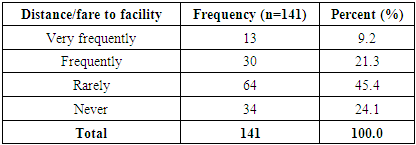
4.12.8. Extent of non-adherence due to Distance to Health Facility
- On distance or cost to the CCC, 45.4% reported it rarely contributed to ART non-adherence but 21.3% of the respondents reported distance or cost to the CCC frequently contributed to ART non-adherence (Table 18).
|
5. Institutional Related Factors
5.1. Non-adherence due to Long Queue and Lack of Family Support
- A quarter (25.5%) of the respondents reported long queuing time frequently contributed to ART non-adherence, while 14.8% reported lack of family support frequently contributed to their ART non-adherence. A relatively small proportion of 2.9% and 5.7% reported long queue and lack of family support very frequently contributed to ART non-adherence respectively (Figure 9). This shows that the health center management needs to come up with modalities to reduce the queues like the queueing theory and appointment system. The staff to client ratio can also be looked into.
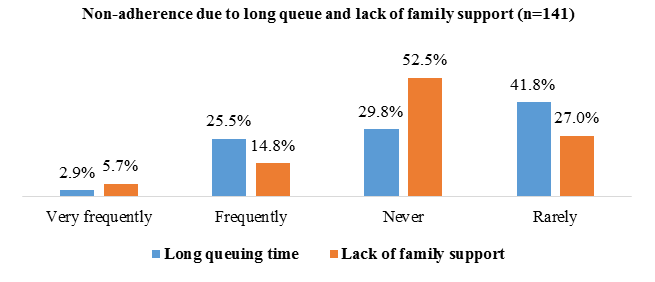 | Figure 9. Non-adherence due to long queue and lack of family support |
5.2. Waiting Time
- Over a third (35.5%) of the respondents reported waiting for up to 30 minutes while 41.1% reported they waited for 31 to 1 hour before being served at the CCC (Figure 10).
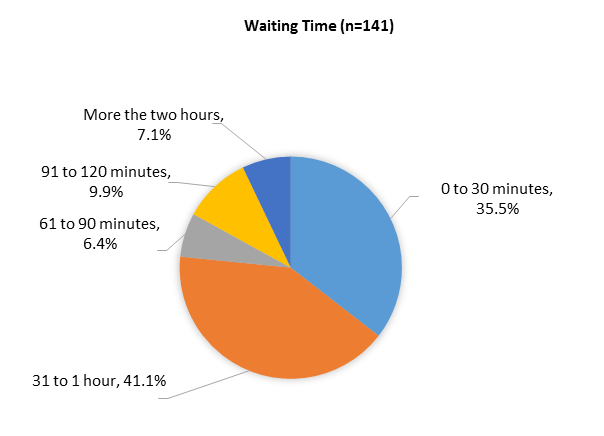 | Figure 10. Waiting time |
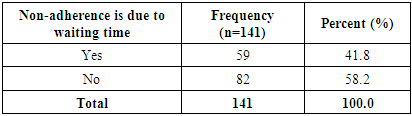
5.3. Non-adherence due to Waiting Time
- Forty one (41.8%) of the respondents reported that long waiting time contributed to their non-adherence to ART (Table 19).
|
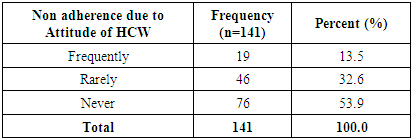
5.4. Non Adherence due to Attitude of Health Care Workers (HCWs)
- Over a half (53.9%) of the respondents reported they never failed to adhere to their ART due to the attitude of the healthcare workers. However, 13.5% of the respondents reported frequent non-adherence due to the attitude of the healthcare workers (Table 20). With majority of the respondents reporting that they do no fail to adhere due to attitude of health workers, it can be assumed that the attitude of health workers in the institution is fairly good.
|
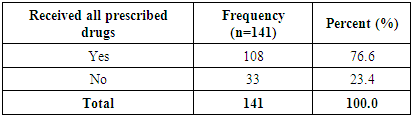
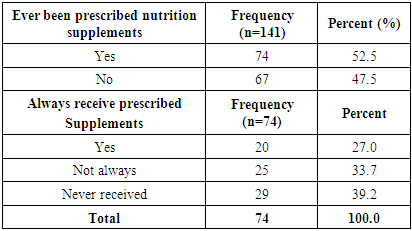
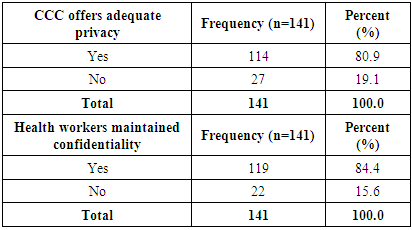
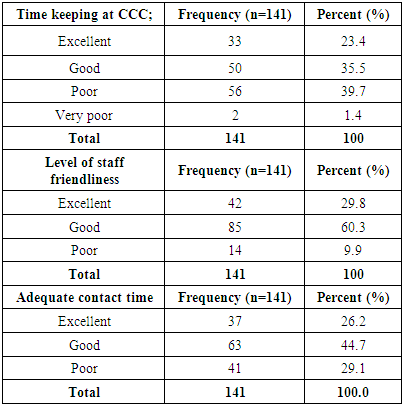
5.5. Respondents’ Responses on whether They Receive all Prescribed Drugs
- Majority (76.6%) of the respondents reported they receive all the prescribed drugs from the CCC while the rest (23.4%) reported that they do not always get the prescribed drugs (Table 21). These findings indicate that despite the waiting time being long, majority of the CCC clients are able to receive drugs as prescribed which is important in the fight against HIV.
|
5.6. Respondents’ Responses on whether They have ever been Prescribed Nutrition Supplements
- More than half (52.4%) of the respondents reported that they had ever been prescribed nutritional supplements, while 27.0% reported they had always received the prescribed supplements. The rest 39.2% reported to have never received the prescribed supplements from the CCC (Table 22). Nutrition is imperative in management of HIV. If a significant number of respondents do not receive nutrition supplements, it is alarming and considering the fact that most of the clients are low income earners.
|
5.7. Adequacy of Privacy in the CCC Clinic
- Majority (80.9%) of the respondents reported the CCC offers adequate privacy while 84.4% reported health workers maintained confidentiality (Table 23). Privacy and confidentiality are vital in the management of HIV. The nurses at Ngenda health center have been able to achieve this although they can still work to achieve 95 or 98%.
|
5.8. Time Keeping, Level of Staff Friendliness, and Contact time with Staff by CCC Staff to Clients
- Over a third (39.7%) of the respondents reported time keeping at the CCC was poor while 35.5% of the respondents reported it was good. Most (60.3%) of the respondents reported good level of staff friendliness at Ngenda CCC while 9.9% reported the level of friendliness was poor (Table 24). With a significant number or respondents pointing out that time keeping and staff friendliness as an issue, there is need for improvement.
|
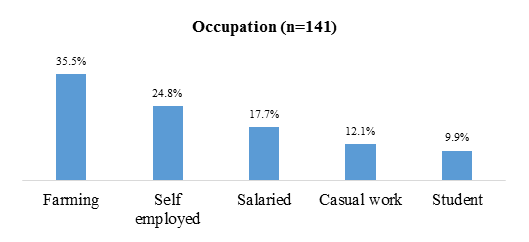
5.9. Access to Information, Counselling and Support
- Majority (78.7%) of the respondents reported that they have access to information, counselling and support at the CCC while the rest (21.3%) reported that they did not (Table 25). The management of the health center should work towards improving on clients’ access to information, counselling and support as a small number of the respondents reported these as lacking.
|
6. Discussion
- The findings of the study point out that most of the CCC clients were in the economically productive age cohort (31 to 40 years) which was also found to be the biggest group which did not adhere to ART. This contradicts findings from several studies that were analyzed by Heestermans et,. al. 2016 [14], which led to the conclusion that clients above the age of 35 years are the most non-adherent as compared to clients between 30 to 40 years who adhere well to treatment. The findings of a meta-analysis by Soomro et., al. 2018 on the other hand led to the conclusion that ART adherence levels in Africa among younger and older adults are comparable [15].Most of the clients in this study had been on ART for 1 to 5 years, were married and a large group were farmers and earned between Ksh. 1,000 and 10,000. A relative big proportion of the CCC clients reported that, their work hinders adherent to ART. A majority of the clients in the study were female, married and had attained secondary level of education. These factors are critical when addressing ART non-adherence since married persons and those who had attained the secondary level of education were found to be the most non-adherent. These findings still concur with the systematic review by Heestermans et, .al. 2016, which indicates the mentioned factors as determinants of adherence to ART [14].The results from this study also indicate that most of the CCC clients had adequate knowledge on adherence and had reported to have adequate information on ART. However, a large proportion of the study population had failed to adhere to their ART for various reasons. Study findings by Raberahona et. al, 2019 on the other hand led to the authors conclusion that the association between good knowledge of ART and high education was independent. Forgetfulness and busy work schedule were other major reasons given by those who failed to adhere to their ART. These findings are in line with a study by Wakibi et al. 2011 which indicated that, the same factors (forgetting and work schedule) were strongly contributing to non-adherence [10].A half of the clients in this study had failed to adhere to ART in the last one month prior to the study and a relatively large proportion of the clients reported having experienced ART side effects. Clients have been known to become non-adherent as a result of adverse or side effects of the antiretroviral drugs. The findings of this study concur with NASCOP 2011, 2013 reports which indicate that, adverse or side effects usually occur on virtually all antiretroviral therapy clients resulting in distressing symptoms that encourage them to be non-adherent [9,11].A proportion of the ART clients in this study were on other drugs and substances. Though this did not show significant relationship to non-adherence, it could result in poor ART uptake and drug interaction among the clients. Kalichman et al, .2019 in a study conducted in South Africa found that 24% of people who per took alcohol stopped taking their ART and 25% who used alcohol believe that those who drink alcohol should desist from taking ART [16]. The findings of the study also revealed that some clients lacked access to information, counseling and support which is a critical component of adherence. Lack of information and counseling services can negatively impact on ART adherence just as confirmed by Heestermans et al. 2016 whose systematic review revealed that patients with higher risk of non-adherence were those patients with poor knowledge of basic HIV concepts due to no or low quality of counseling [14]. A relatively high non-adherence rate was reported from the study findings since almost two thirds of the clients had ever defaulted from ART. The highest number of those who were non-adherent was found to be the users of public service vehicles (matatu). Those who walked to the facility were found to be better in adherence than those who used other means of transport to the health facility. This finding concurs with Byakika et al 2013 study which investigated factors associated with ART non-adherence in Nairobi, which found out that, those clients who accessed ART services within walking distance from their homes were likely to adhere better than clients who sought the CCC services in faraway clinics [7]. This is a crucial fact since difficulties in accessing ART services due to distance from home will often contribute to non-adherence among the clients. Institute of tropical medication and infectious disease 2011 report also indicated that clients accessing ART services within walking distance adhered well than those traveling long distance to the clinics due to transport difficulties. Uzochukwu et al, 2009 study further revealed health facilities located faraway from clients contributed to non-adherent to ART services [17].The study also showed that most of the clients used between 10 and 100 shilling for transport to the health facility. A relatively large proportion of this group was also found to be non-adherent to their ART. The study further revealed most of the client wait for between half and one hour at the CCC. A proportion of the clients failed to adhere as a result of long waiting time. These finding concurs with Wakibi et al 2010 study which indicated that long waiting time in the facility made clients to become more non-adherence to ART than clients who took less time in the clinic [10]. The findings of this study indicate that most clients received all the prescribed drugs. However for those who were prescribed nutritional supplements, some never received the supplements while others did not always receive the supplements. NASCOP 2013 report recommends that nutritional support and supplements are a critical component of ART to deserving clients as ARVs are known to lower appetite and may even lead to mal absorption. Nutritional support is therefore needed to promote adherence as the clients are given food which has easy palatability and consequently increases their energy and promotes recovery [11]. The clients who visited the CCC felt that there was an existence of lack of adequate privacy and lack of confidentiality by the healthcare providers. Poor time keeping, low level of friendliness among staff, inadequate contact time, negative HCWs attitude, and poor adherence was also experienced by the clients. Some clients reported non adherence as a result of negative attitude from the healthcare providers. These factors are documented in Sonjobo 2008 report, as contributing to non-adherence and that ART clients showed good adherence when they have a long standing and trusting relationship with healthcare providers [18]. This further concurs with Aspeling et al, 2008 study which revealed that, a poor healthcare provider and client relationship leads to non-adherence among ART clients [19]. Wroth et al., 2006 report also indicated that, clients who are gladly and comfortably received by healthcare providers are more likely to collect their drugs and adhere to the treatments than those who are poorly received in the CCC. The study also revealed existence of poor healthcare provides support to adherence [20]. Some clients in the study lacked treatment supporters, and others had never disclosed their status. Support is an important factor in adherence to ART thus needs to be encouraged and improved among the clients. The study further revealed that the clients who had disclosed received moral, financial and spiritual support which is important in ensuring ART adherence. However, from the study the researchers found out that, having a treatment support did not guarantee adherence since there was even a higher rate of non-adherence among clients with support than those without. This is a contradiction to Hardon et al 2006 report which indicated that, clients receiving support from family and friends on the use of drugs adhere more than those who do not receive any support from their families and loved ones. Adequate support plays an important role in encouraging the clients to continue with their ART as required [13].An existence of stigma was revealed both at the family and community levels from the findings of this study. Stigma level was noted to be highest at the community level and lesser at family level. This concurs with Katz et al 2013 report which strongly indicated that, social stigma is one of the major factors that prevent ART clients from both revealing their status and adhering to ART [12]. Stigmatized clients are three times more likely to non-adhere to their ART than clients who are not stigmatized. The study identified lack of involvement in social functions, fear of sharing, gossiping and avoiding associating with the clients as the forms of community stigma experienced by the clients. A study conducted in Nigeria by Okoronkwo et al., 2013 also indicated that, stigma hinders employed persons from adherence since they do not want to be seen carrying their drugs to their work places while those who carry them hide when taking them or even fail to take the drugs when at work thus omitting some doses [21]. A study conducted in South Africa by Kalichman et al., 2019 on the other hand also led the authors to the conclusion that behavioral effects of stigma directly hamper ART adherence [22]. Some clients in this study reported to defaulting as result of spiritual healing intervention through prayers. Parsons et al. 2006 concluded that it is important to remember to address a patient’s religious beliefs as part of medical care. This is so because in Parsons et al. 2006 study certain religious practices were found to be positively associated with adherence and others negatively related to adherence [23].
7. Conclusions
- The achievement and maintenance of high adherence level in all ART clients is critical to ensure viral load suppression which is one of the 90-90-90 strategy requirements in HIV prevention and control strategy. There is therefore need to generally assess the various factors contributing to non-adherence to ART in the county, and initiate result oriented programs that will contribute to high level ART adherence in the County. Ng’enda Health Facility Management Team therefore needs to identify specific interventions as per the study recommendations in order to improve and maintain high adherence level among the ART clients seeking CCC services in the facility.
8. Recommendations
- The Ng’enda CCC and the Health facility Management Team (HMT) need to collaborate with all the different stakeholders in HIV/AIDS prevention and control program in order to identify and implement a community sensitization and awareness programs on drug adherence. The team should also involve the church to take part since the largest proportion of the ART clients are Christians.The facility HMT should also initiate community sensitization programs where the community members will be sensitized and empowered to strengthen family support systems and hence be aware of the benefit it has to both chronically ill patients in general, including ART clients, to the immediate family and the community at large. The HMT also needs to design stigma reduction intervention both at individual and community level since it plays a key role in non-adherence. This needs a multidisciplinary approach as stigma is multifaceted and may take many different forms and occurs at different settings both at the concerned institutions and community levels. The healthcare providers in the CCC need to counsel and encourage the clients on the benefits accrued from HIV status disclosure. They should also initiate a support system for the client treatment supporters to assist them to offer holistic and quality support to their ART clients.The healthcare workers need also to improve their relationship and support adherence support systems. They should also have a positive attitude towards ART clients as they serve in the CCC.The County Government of Kiambu through the County HMT needs to plan and conduct a large scale adherence survey in order to identify critical factors contributing to non-adherence and roll out a countywide adherence improvement program across the health facilities offering CCC services in the County.
ACKNOWLEDGEMENTS
- The authors give special thanks to the management of Ng’enda Health center and the clients who participated in this study. The authors also appreciate Mt. Kenya University Research Department for the support provided.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML