-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2019; 9(2): 23-29
doi:10.5923/j.phr.20190902.01

Socio-economic, Demographic and Environmental Factors Effects on Under-Five Mortality in Empowered Action Group States of India: An Evidence from NFHS-4
1Ph.D. Scholar, USMPMHS, GGSIP University, New Delhi, India
2Scientist ‘F’, National Institute of Medical Statistics, ICMR, New Delhi, India
Correspondence to: Sarvesh Kumar, Ph.D. Scholar, USMPMHS, GGSIP University, New Delhi, India.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

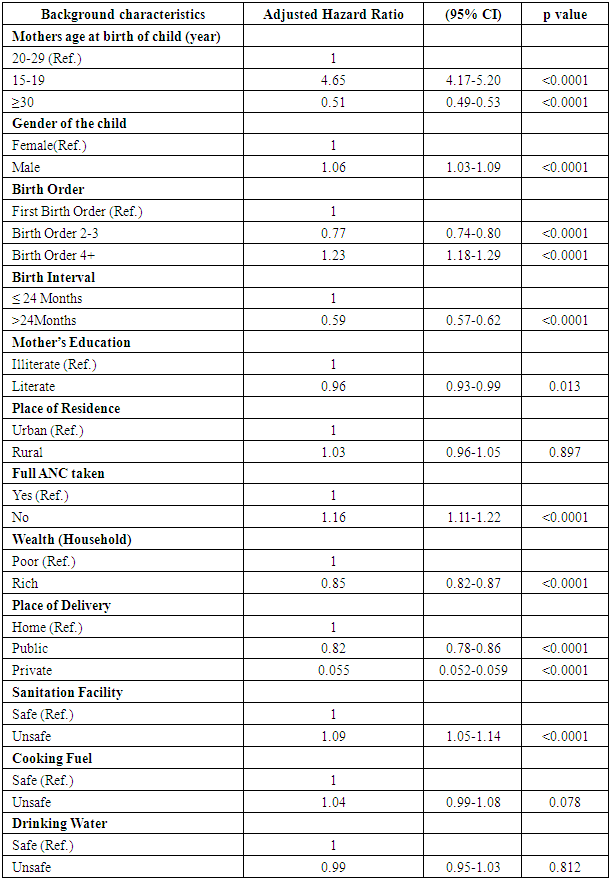
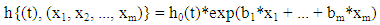
Background: Globally, in both under developed and developing countries including India have experience substantial decline under-five mortality rate i.e., infant and child mortality rates due to reproductive and child health programme intervention during past two decades. In India, overall U5MR has been declined from 74 per thousand live births in 2005-06 to 50 per thousand live births in 2015-16. The Empowered Action Group (EAG) of states has very high under-five mortality as compared to Non-EAG states. The aim of the study was to identify the socio-economic, demographic and environmental factors effect on U5MR in EAG States of India. Data and Methods: The 9 EAG States NFHS-4 data had been analyzed and used for this study. The National Family Health Survey is a cross-sectional household survey conducted in year 2015-16. The survival analysis i.e., Kaplan-Meier with log-rank test and Cox-proportional hazard regression model was used to assess the effects of socio-economic, demographic and environmental factors on risk of under-five mortality. Total information of 322396 children born during past ten years preceding survey and their mother's characteristics were analyzed. Results: The result showed that under-five mortality was significantly associated with mother's age at the time of birth, sex of the child, previous birth interval, birth order, household wealth, toilet facility and cooking fuel. Children of young mother < 20 years are 4-5 times more likely to die as compared to children of mother's age 20-29 years (HR = 4.67, 95% CI: 4.17-5.20) after controlling for other factors. The risk of dying was higher among children whose mother' illiterate and poor household compared to children whose mothers were literate and belong to rich household. Conclusion: To achieve the sustainable development goal 3 targets on under-five mortality by 2030, the EAG states clearly need to reduce U5MR [1].
Keywords: NFHS, MDG, SDG, EAG, Under-five mortality
Cite this paper: Sarvesh Kumar, Damodar Sahu, Socio-economic, Demographic and Environmental Factors Effects on Under-Five Mortality in Empowered Action Group States of India: An Evidence from NFHS-4, Public Health Research, Vol. 9 No. 2, 2019, pp. 23-29. doi: 10.5923/j.phr.20190902.01.
1. Introduction
- In global scenario, India has the maximum share of mortality among the Under-five deaths. The Millennium Development Goals (MDG), in the year 2000, world leaders agreed to set of 8 goals and 48 indicators; one of them was to reduce the under-five mortality and infant mortality rate by two-third at the end of 2015. During this era of MDG, the major progress has been made in reducing the child mortality throughout the world [2]. In various round of National Family Health Survey data the Under-five deaths has been decline more than half in the last 20 years i.e. 109deaths (per 1000 live births) in NFHS-1 (1992-93) to 50 deaths (per 1000 live births) in NFHS-4 (2015-16) [3]. In 2016 world leaders adopted 17 Sustainable Development Goals (SDG) and 169 indicators to achieve by 2030 with an agenda of sustainable development. The third goal of Sustainable Development Goals focuses to ensure healthy lives and promote wellbeing at all ages. As per SDG 3.2 target by 2030 to end preventable deaths of new borns and children under-five years of age, with all countries aiming to reduce neonatal mortality to at least as low as 12 per 1000 live births and under-five mortality to at least to as low as 25 per 1000 live births. For the Under-five mortality, the national level estimate has the huge diversity across the states and their districts. Social and economic development of a nation is often reflected by the existing infant and child mortality rates. India has the world’s highest percentage (21%) of under-five deaths, estimated at 1726000 in 2009 [4]. The north-south variation in child mortality in India is reflected in various literatures [5, 6] where some of the north Indian states such as Rajasthan, Uttar Pradesh, Bihar, Orissa, Chhattisgarh and Madhya Pradesh persistently performed poorly in health care [7]. The Ministry of Health and Family Welfare, India established Empowered Action Group (EAG) in 2001 to have special focus by monitoring and facilitating the attainment of national health goals on some of these states which are demographically lagging behind. In India, studies on child mortality have mainly addressed the role of maternal, socioeconomic and health-related determinants [8-10]. On account of the unacceptably high fertility and mortality indicators, the eight Empowered Action Group (EAG) states (Bihar, Chhattisgarh, Jharkhand, Madhya Pradesh, Orissa, Rajasthan, Uttarakhand, Uttar Pradesh and Assam), which accounts for about 48% of India’s population, are designated as ‘‘High Focus States’’ by the Government of India.As a part of the Millennium Development Goals, India seeks to substantially reduce its burden of childhood mortality. Six states, namely, Kerala, Tamil Nadu, West Bengal, Maharashtra, Punjab and Himachal Pradesh are likely to achieve the goal. Studies conducted globally and in India suggest associations of sex of the child, mother’s exposure to mass media, use of clean cooking fuel, access to a toilet facility, improved/safe drinking water facility, mother’s religion and ethnicity, income of the household, birth order, mother’s age at birth, birth intervals, availability of professional antenatal and delivery care, full immunization of children, mother’s education, and urban-rural residence with infant and child mortality [9, 11]. A number of studies attempted to demonstrate the indirect causes of childhood illnesses or mortality, but none of them proved as influential in formulating public policy. So, the aim of the study was to identify the socioeconomic and demographic factors effect on under-five mortality in Empowered Action Group (EAG) states of India.
2. Materials & Methods
- Data and sampling frame: We have primarily used the fourth round of Demographic and Health Survey (DHS) for India, known as National Family Health Survey (NFHS-4) conducted in the year of 2015-16 under the leadership of Ministry of Health and family Welfare (MoHFW), Government of India. For the first time in NFHS-4 survey in India all 640 districts level information were collected. NFHS-4 was based on 1,315,617 children born of 699,686 women in 601,509 households with a response rate of 98%. The survey included 425,563 households from rural areas and 175,946 households from urban areas. Multistage stratified sampling methods were used to create a sample representing individuals from all 29 states of India. This study is based on only Empowered Action Group (EAG) states in India which are Uttar Pradesh, Madhya Pradesh, Bihar, Rajasthan, Orissa, Chhattisgarh, Jharkhand and Uttarakhand and Assam. NFHS provides state and national level information on Fertility, family planning, infant and child morbidity and Mortality, maternal and reproductive health, nutritional Status of women and children, and the quality of health Services. In NFHS, all eligible women aged 15-49 years were asked to provide information on complete birth history, which included gender, month and year of birth, and survival status for each live birth. The information on age at death was recorded in days for children who had died in the first month of life; in months for children who had died after the first month but before completion of their second birthday, and in years for children who had died at later ages. For children who had died after their second birthday, age at death in months was computed.Dependent variable is under five child mortality which is defined as probability of dying children before the fifth birthday.Independent variables were taken mother’s age at the time of child birth (15-19, 20-29, 30+ yr), gender of the child (female/male), birth order (1, 2-3, 4+), Birth interval (≤24 months, >24 months); mother’s Education (illiterate, literate); mother’s work status (Yes/No); Place of Residence (Urban/Rural);Wealth (poor/rich); full antenatal care (ANC) (no/yes); sanitation facility (unsafe/Safe); cooking fuel (unsafe/safe); drinking water (unsafe/safe).Wealth: NFHS did not collect information on income. The level of economic status of a woman was assessed computing a composite index of household wealth Indicating possession of wealth or assets by the Household to which they belonged. We have categorized into categories as belonging to poor and rich.Full ANC: We have categorized full ANC into Yes and No. Yes is considered as those women’s taken more than 4 ANC visits during her pregnancy.Sanitation facility: Household having either flush, or a pour flush which is connected to a sewer system, septic tank or pit latrine, a ventilated improved pit (VIP), a bio gas latrine, a pit latrine with slab and twin pit, and composting toilet regarded as ‘safe’ sanitation as opposed to those without any facility taken as a (unsafe).Cooking fuel: The households using liquefied Petroleum gas, electricity, kerosene and biogas were considered as (safe) fuels. Those were using dung cake; firewood and coal were regarded as users of high polluting fuels (unsafe).Safe drinking water: Households with access to source of drinking water piped into dwelling/ yard /plot, water available from public tap or stand pipe or a tube well or borehole or a protected well or spring considered as a ‘safe’.Cox Proportional Hazard Model: The Cox model is based on a modeling approach to the analysis of survival data. The purpose of the model is to simultaneously explore the effects of several variables on survival. Cox’s method is similar to multiple regression analysis, except that the dependent variable is the hazard function at a given time. If we have several explanatory (x) variables of interest (for example, age, sex and treatment groups), then we can express the hazard or risk of dying at time t as:
 Linearizing the model by dividing both sides of the equation by h0(t) and then taking the natural logarithm of both sides:
Linearizing the model by dividing both sides of the equation by h0(t) and then taking the natural logarithm of both sides: Where h(t,...) denotes the resultant hazard, given the values of the m covariates for the respective case (x1, x2, ..., xm) and the respective survival time (t).The term h0 (t) is called the baseline hazard; it is the hazard for the respective individual when all independent variable values are equal to zero.
Where h(t,...) denotes the resultant hazard, given the values of the m covariates for the respective case (x1, x2, ..., xm) and the respective survival time (t).The term h0 (t) is called the baseline hazard; it is the hazard for the respective individual when all independent variable values are equal to zero. An important feature of this formula, which concerns the proportional hazards (PH) assumption, is that the baseline hazard is a function of t, but does not involve the X’s. In contrast, the exponential expression shown here, involves the X’s, but does not involve t. The X’s here are called time-independent X’s.Statistical analysis: To assess the effects of socio-economic, demographic and environmental factors on risk of under-five mortality cox proportional hazard model was used. Firstly we have used Univariate analysis for the association of the dependent and independent variables. After that for the modeling we have used multivariate analysis using cox proportional hazard model. We defined dependent variable as Time (age of the child) and survival status of child (0 if event has occurred i.e. child died and 1 if child is Alive) during period (0-4 Yrs). Results of the multivariate Analyses are presented as hazard ratios (risk of dying). If hazard ratio is > 1 for a predictor variable, it means that the hazard is higher, i.e. increased risk of death and if hazard ratio is < 1, it implies a decreased risk of death. All statistical analysis has been done on SPSS 22.0 software. A p value is < 0.05 is taken to be statistical significant.
An important feature of this formula, which concerns the proportional hazards (PH) assumption, is that the baseline hazard is a function of t, but does not involve the X’s. In contrast, the exponential expression shown here, involves the X’s, but does not involve t. The X’s here are called time-independent X’s.Statistical analysis: To assess the effects of socio-economic, demographic and environmental factors on risk of under-five mortality cox proportional hazard model was used. Firstly we have used Univariate analysis for the association of the dependent and independent variables. After that for the modeling we have used multivariate analysis using cox proportional hazard model. We defined dependent variable as Time (age of the child) and survival status of child (0 if event has occurred i.e. child died and 1 if child is Alive) during period (0-4 Yrs). Results of the multivariate Analyses are presented as hazard ratios (risk of dying). If hazard ratio is > 1 for a predictor variable, it means that the hazard is higher, i.e. increased risk of death and if hazard ratio is < 1, it implies a decreased risk of death. All statistical analysis has been done on SPSS 22.0 software. A p value is < 0.05 is taken to be statistical significant.3. Results
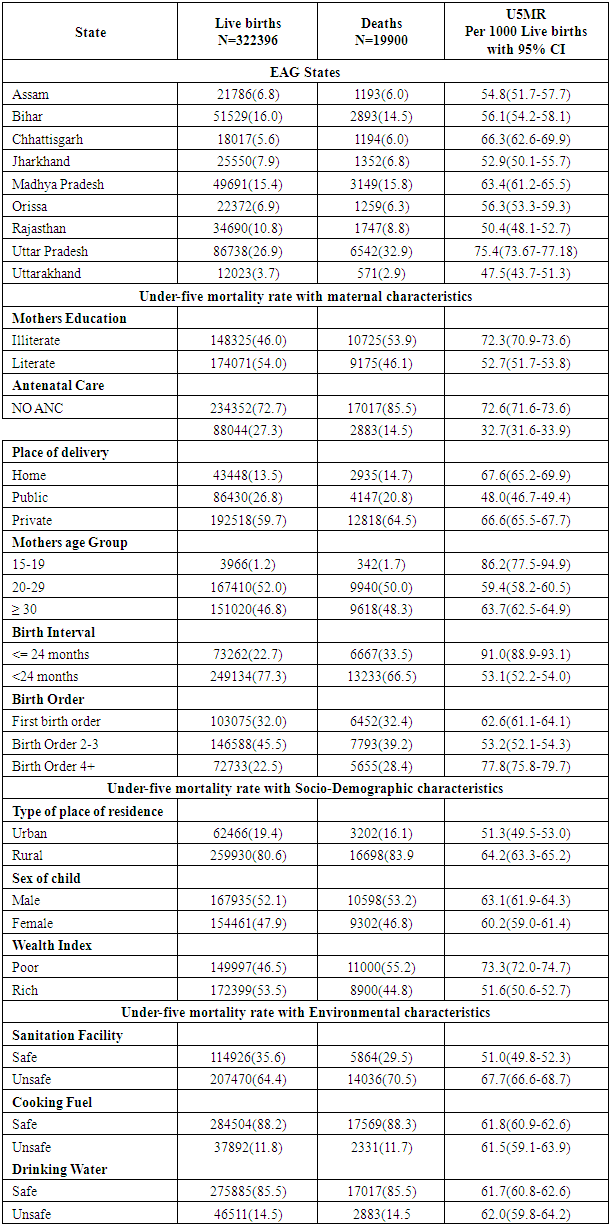
- Total 322396 female respondents of age 15-49 years were interviewed from all 9 EAG states of India. Out of total 19900 under- five deaths was reported in EAG states. Kaplan Meier plot showed the survival probability and censored observations of EAG and Non EAG states of India [Fig 1]. It was observed that probability of dying children was decreasing as age of children increasing. It also shows that the probability of dying children is higher in EAG states as compare to Non EAG states of India.
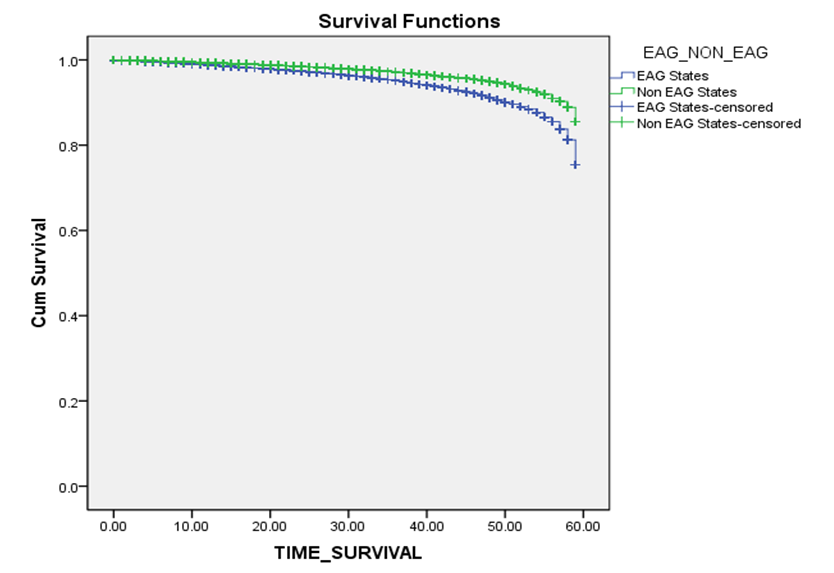 | Figure 1. Kaplan Meir Survival Curve of Under-five mortality in EAG states and Non EAG States of India |
|
|
4. Discussion
- This study showed that in EAG states high mortality due to poor socioeconomic status, demographic stages, low female autonomy, likewise the poor health system performance and lower utilization of maternal and child health services [12]. The study also found the determinants that were significantly associated under-five child mortality among EAG states of India during 2015-16. These determinants were mother’s age at child birth, gender of the child, birth order, birth interval, household wealth status, and place of residence. Some studies also found the similar observations in population [13-15]. Increasing effect of low age of mother at birth on mortality could be due to wide gap in utilization of the mother and child health (MCH) care services between younger and older mothers. There is a need for programs to concentrate on delaying the age at first birth for younger women in EAG state of India. These kind of efforts would not bring down the under-five child mortality but also help in reducing the morbidity conditions such as pneumonia and diarrhea in children under five [13, 16, 17]. Birth order and preceding birth interval of the child were found significantly associated with under-five mortality [18]. We can say that under-five child mortality tends to increase with the birth order. The risk of child mortality was higher in first order births. However, a study on utilization of maternal health services suggested that higher mortality risk among first order birth could be linked with the early childbearing trends and lower utilization of maternity services in developing countries like India [19]. This study finds out a higher risk of under-five mortality among males as compared to females in EAG states of India. Similar findings have been observed in general population and are consistent with other studies [20, 21]. Biologically a male child is at higher risk of mortality as reflected by the under-five mortality rates, however, the socio-behavioral causes such as gender based discrimination may in part attribute for the higher mortality of a female child. However, since literature suggests gender equitable relationships in the population [22]. Our findings showed a positive association of education with child survival. The children of educated mothers have a greater chance of survival, in part because educated women seek out higher quality services and have a greater ability to use healthcare inputs [23, 24]. A considerable poor-rich gap in mortality has come out from this study. Several studies have ingeminate the case of economic inequality and health care access leading threat to the newborns at early age [25].
5. Conclusions
- After this study analysis we can conclude that the factors associated with under-five mortality more or less are same. The running national programs for the decreasing under-five mortality have been focusing on educating women on increasing age at marriage, age at first birth, and increasing the birth interval between two births. The originality of the study lies in its ability to identify factors affecting on under-five mortality to meet the SDG-3 target. In this study our analysis describes the huge variation cross the Indian states in U5MR [26]. While only few states and UTs have already achieved the SDG-3 target for U5MR and many states may not achieve the SDG-3 target even in 2030.This study has a state level comparative analysis to show that the majority of high risk states for U5MR belong to the EAG states. The huge variations in U5MR in EAG states are due to wide disparities in the level of socio-economic development [27]. The findings of this study have substantial for policy makers, health professionals, program managers and administrative authorities. India needs more in-depth programs, particularly in certain regions not just in the most populous and demographically backward regions, but especially in EAG states.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML