-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2019; 9(1): 13-21
doi:10.5923/j.phr.20190901.03

Malaria: Knowledge, Attitudes and Acceptances of Rapid Diagnostic Test amongst Primary Healthcare Workers in Some Selected Local Government Areas, Lagos State, Nigeria
Udeme Asibong1, Aniekan Etokidem2, Ubong Akpan3, Felix Archibong1, Inyang Asibong2, Francisca Funke Adeleye4
1Department of Family Medicine, University of Calabar, Cross River State, Nigeria
2Department of Community Medicine, University of Calabar, Cross River State, Nigeria
3Department of Obstetrics and Gynaecology, University of Calabar, Cross River State, Nigeria
4Department of Community Health and Primary Care, University of Lagos, Lagos State, Nigeria
Correspondence to: Udeme Asibong, Department of Family Medicine, University of Calabar, Cross River State, Nigeria.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction: Malaria still remains a public health challenge in Nigeria and its treatment is expensive due to the introduction of Artemesinin-based Combination Therapy (ACT). This burden can be minimised through confirmation of the diagnosis using Rapid Diagnostic Test (RDT) at the primary care facilities. However one may be concern about the knowledge, acceptance and proper usage of RDTs in the management of malaria at the primary care level. Method: Two hundred and sixty eight primary health workers in Lagos, Nigeria were recruited into this cross-sectional descriptive study using self-administered questionnaire. Epi- info version 3.5.1 statistical software was used for data analysis. Results: Two hundred and one (75%) of the total participants were female and majority (34.3%) were aged 40 years or more. None of the respondents had good knowledge of RDT usage, however about 200(74.6%) had fair knowledge of it. Good acceptance of RDT was 7(2.6%) even though 203(75.7%) participants had used RDT before this study was conducted. Nurse/midwives showed significantly good acceptable level of RDT compared to other cadres of staff (X2 = 41.783; P-VALUE = 0.003). Conclusion: The health workers in PHC have fair knowledge, acceptance and usage of RDT despite the fact that most of them have not been trained on proper usage of RDTs for management of malaria. Therefore there is need for periodic training of the workers on proper use of RDTs.
Keywords: Artemisinin combination therapy, Malaria transmission, Infant morbidity, Rapid diagnostic test, Malaria microscopy
Cite this paper: Udeme Asibong, Aniekan Etokidem, Ubong Akpan, Felix Archibong, Inyang Asibong, Francisca Funke Adeleye, Malaria: Knowledge, Attitudes and Acceptances of Rapid Diagnostic Test amongst Primary Healthcare Workers in Some Selected Local Government Areas, Lagos State, Nigeria, Public Health Research, Vol. 9 No. 1, 2019, pp. 13-21. doi: 10.5923/j.phr.20190901.03.
1. Introduction
- In Nigeria, high malaria transmission is recorded between 154 and 729 cases per 1000 population and malaria accounts for about 30% of all hospital admissions and about 60% of all out- patient attendance. [1] About 50% of Nigerian population have at least one episode of malaria each year. [1] It is one of the leading causes of under-five morbidity and mortality contributing 30% of under five and 25% infant mortality. [1] It is also responsible for an annual loss of 132 billion naira in cost of treatment of malaria. [1] This can be reduced through proper diagnosis of Malaria by using Rapid Diagnostic Tests (RDT) in Health facilities.Diagnosis of malaria can be done clinically using symptoms and signs, biologically using Giemsa stained blood smear or fluorescent staining, and by using molecular methods such as DNA probes and polymerase chain reaction. [2] Signs and symptoms of malaria are non-specific and may mimic other febrile illnesses endemic in the tropics. Microscopic examination of Giemsa-stained blood smears has subsequently become the gold standard of malaria diagnosis because it is inexpensive to perform, able to differentiate malaria species, and quantify parasites. [1, 2] However, microscopy requires well-trained, competent microbiologists and rigorous maintenance of functional infrastructures plus effective quality control and quality assurance. These requirements led to development of Rapid Diagnostic Device which is simple to perform, and easy to interpret for the diagnosis of malaria.Universal access to parasite-based diagnosis of malaria-like febrile illness is the current global policy recommendation due to the use of Artemisinin - based Combination Therapy (ACT), as the first line anti- malaria treatment for Plasmodium falciparum infection in most endemic Countries. [3] However ACT is expensive and relies on an insecure supply of raw materials. Therefore, RDT is important in the diagnosis of malaria by differentiating malarial cases from non-malarial cases to ensure that ACTs are used for malaria cases only. Factors reported to have reduced the appeal of RDTs included the cost of the test and the extra time required to be tested. [4] Studies have also shown that utilisation of RDT is high and its introduction has led to judicious use of antimalarial drugs, including ACTs. [5, 6] However, some other previous studies reported under-utilisation of RDT. [7, 8]Rapid Diagnostic Tests which is expected to reduce the overuse of antimalarial drugs, especially the expensive ACTs, by ensuring that treatment is targeted to patients suffering from malaria as opposed to treating all patients with fever, which was the case when chloroquine was the first-line drug. [5, 8] This is a strategy for improving management and curtailing costs, since the argument has been that, if the result of a test is not going to influence management, then doing the test is a waste of money. [9] Therefore, there is a need for the government to engage in supportive supervision of health workers and to constantly remind them that the cost of treating all individuals regardless of the test results is enormous, both for the patient and to the health services.This study seeks to find out knowledge gaps if any, relating to malaria and acceptance of RDTs by PHC workers in some selected Local Government Areas in Lagos State, thereby providing adequate information for future development of PHC workers which could be included in their training curriculum.
2. Methods
- This study was a descriptive cross sectional survey sampling 299 Primary Healthcare workers in Government PHC facilities in Lagos state. These include; Doctors, Midwives, Nurses, Community Health Officers (CHOs), Community Health Extension Workers (CHEWs), Environmental Health Officers, Health attendants.Multi stage sampling technique was used to recruit participants. The respondents were given self-administered questionnaires and focus group discussion was carried out to obtain more data not easily obtained by quantitative method.Data was cleaned and analysed using Epi- info version 3.5.1 statistical software, as well as Microsoft Excel 2007. The analysed data was presented as frequency tables. Inferential statistic was used to test for associations between variables of interest.
3. Results
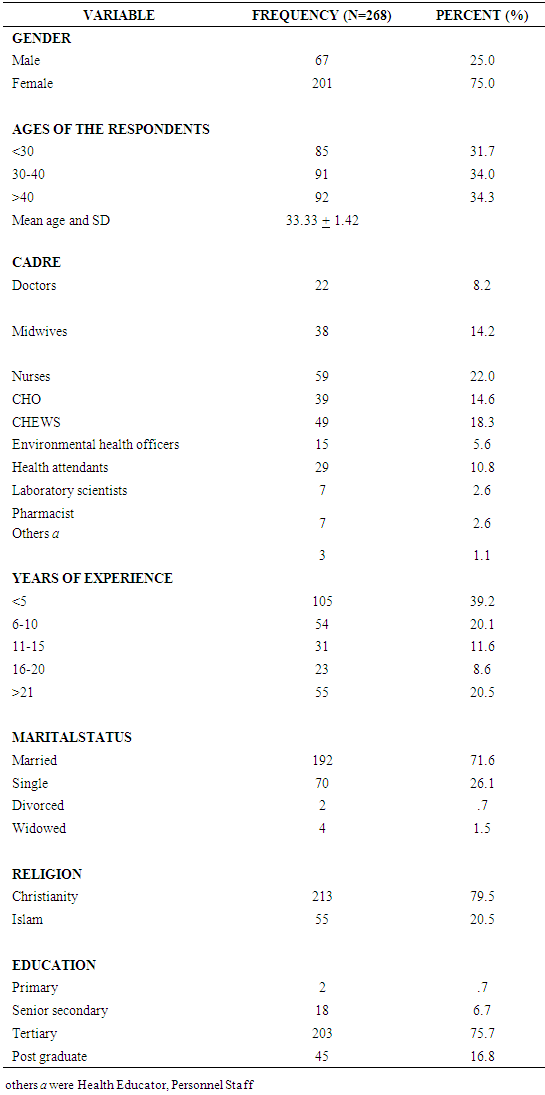
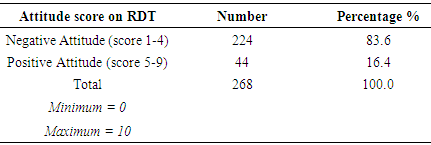
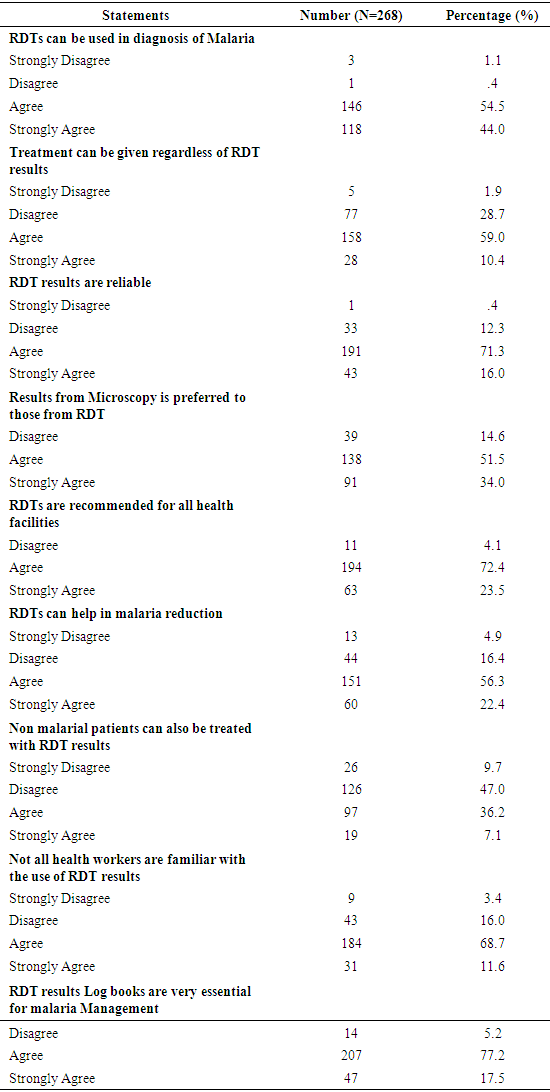
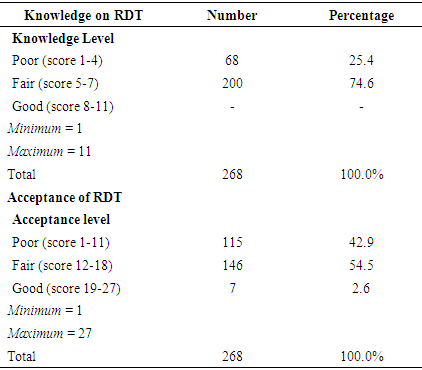
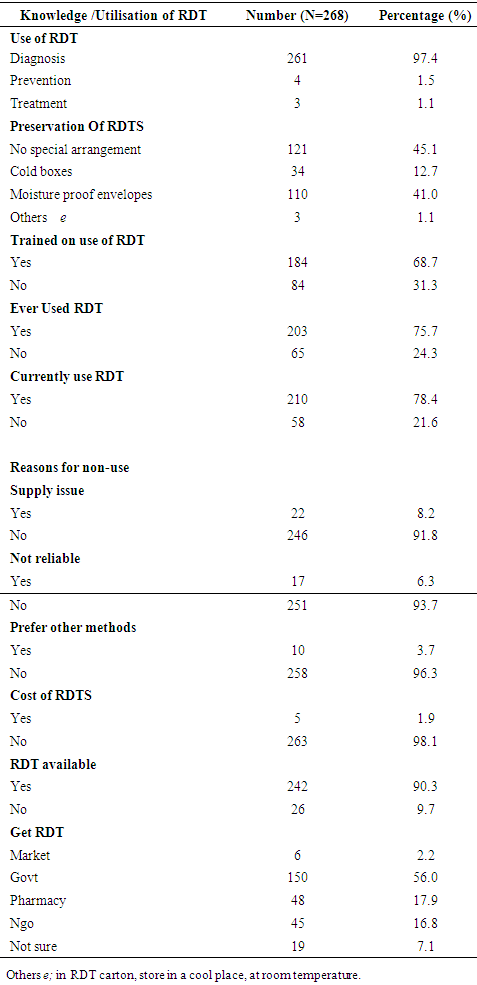
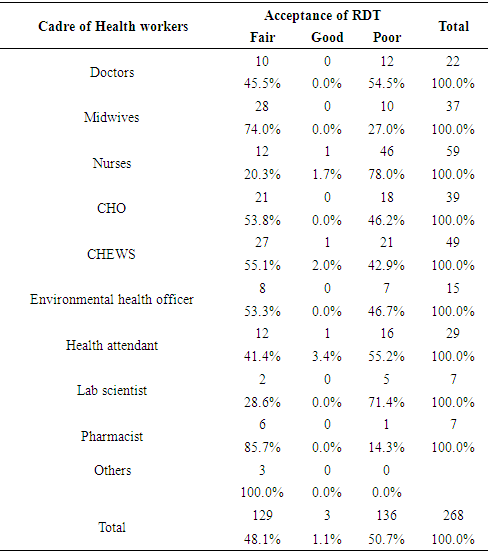
- The study was carried out on a total of 299 health workers but 268 of the respondents (about 90%) completed the questionnaire with female being more than male by 134 (50%). The age range of the respondents was 24 to 58 years with a mean of 33.33 ± 1.42 years and majority 176(65.8%) were 40 years and below. The duration of employment ranged from 1 to 30 years and majority 159(59.3) of the participants were employed 10 years or less prior to this study. About 93% had post-secondary education.Less than 20% of the respondents had positive attitude to RDT. Two hundred and sixty four (98.5%) of participants agreed to the fact that RDTs can be used for diagnosis of malaria while 44(12.7%) said RDT for diagnosis of malaria was not reliable. Blood smear microscopy diagnosis of malaria was preferred to RDTs by 229(85.5%) 0f respondents. One hundred and sixteen (43.3%) agreed that patients with negative RDT result should be treated for malaria.The respondents that had not been trained on the use of RDTs were about 85(31.7%). Participants that had fair knowledge of RDT were 200(74.6%) and none had good knowledge of RDT. Majority of them said there was no special arrangement needed for preservation of RDTs. Only 7(2.6%) had good acceptance level of RDT and 203(75.7%) had used RDTs.The RDTs used in the health facilities (56%) were supplied by government and only 2.2% were gotten from the open market. From the questionnaire a participant was said to have good knowledge of RTD if he scored 8 out of 11. From this study no respondent had good knowledge of RTD. Fair knowledge of RTD was 5 – 7 while poor knowledge was 1 -4 and the difference between these was 132(49.2%). Acceptance of RTD means readiness to use the test. Good acceptance of RTD was the respondent that scored between 19 and 27 on the questionnaire while fair acceptance scored 12 - 18. The difference between participants with good and fair acceptance was 139(51.9%).Comparing Cadre of Health Workers and Acceptance of RDT using the Chi-Square test indicated that there was statistically significant association between Cadre and acceptance of RDT (Chi-square =41.783, DF =20, P-value = 0.003) Majority of the Midwives had a fair acceptance of RDT when compared to other Cadres of Health workers 28 (74.0%) as shown in Table 6.
|
|
|
|
|
|
4. Discussion
- The study revealed that the lowest age of the participants was 24 years and the highest was 58years (mean age of 33.33 ± 1.42 years). The respondents that were married were 192(71.6%) and the males were 67(25.0%) while females were 201(75.0%). Most of the Health workers were Nurses 59(22.0%). This demography was in contrast to a previous study carried out in Ibadan, where there were more males 39(63.9%), than females 22(36.1%), and CHEWS 34(55.7%) made up the most health workers in the study. [10]The prescription of ACTs increased after the introduction of RDTs. This was similar to a previous study that has been carried out. [4] This may likely implies extensive over use of antimalarial drugs. [5, 7] In this research, health centre workers gave ACTs to patients with negative RDT results and this proportion was quite high. Studies in other settings have also confirmed this trend in which clinicians were reluctant to refrain from treating malaria even after a negative RDT test. [2, 11] Similarly, some studies also revealed that even when the tests results are available, health workers do not apply treatment according to the result of malaria tests. [12, 13] In a study carried out in Burkina Faso, 80 to 85% of RDT-negative febrile patients were treated for malaria, [14] while in contrast, another study reported a level as low as 16% of RDT- negative febrile patients were treated for malaria. [4]In contrast to our results, high adherence to RDT results by health workers was reported in Dar es Salaam, Kenya, Tanzania and Zanzibar. [15-18] However, a study in Enugu also showed that adherence to RDT results by health workers was low. [19] In a study done in Cameroon, health workers reported that they gave positive results to please the patient so that they feel they have not wasted their money on a test, as well as safeguard their reputation as a negative result would mean the health worker is incompetent. [20]Also utilisation of RDT in the PHCs was high, 210(78.4%), which was similar to other studies. [2, 4] However some other previous studies reported underutilisation of testing facilities. [7, 8] This affects the use of RDT which is expected to reduce the overuse of antimalarial drugs, such as ACTs, by ensuring that treatment is carried out only on confirmed cases of malaria. This is a strategy would improve patients’ management, curtailing costs and may prevent drug resistant malaria. [5, 12, 15]The results of this study indicate that health workers perceived RDT to be more effective for malaria diagnosis than microscopy and clinical diagnosis, and that it has a lot of benefits. This is in contrast to a study done in Enugu, Nigeria, [21] where the use of laboratory diagnosis (RDTs and microscopy) was low in the study. The low usage of microscopy at 39.2% for diagnosis in this study was similar to the findings of a previous study in South East, Nigeria. [22] Despite the fact that microscopy is regarded as the gold standard for malaria diagnosis; this is a positive development, as this shows the acceptability of RDTs among the health workers. In addition, some of the health workers said they read the test results too soon. This problem has been noted elsewhere, and it has been suggested that the reason for this might be that the package instructions give insufficient emphasis to the importance of waiting time. [12] Hence, the RDT manufacturer might do well to lay emphasis on the waiting time. This is similar to the findings in Tanzania which stated that several factors in the manufacturing process as well as environmental conditions may affect performance. [12]The level of awareness of RDTs by all the providers was not high enough for such an item of enormous utility as RDTs. This calls for creating awareness about RDTs among health workers. If people do not know about a new product and the likely benefits that could accrue from its use, they are not likely to use it and this may lead to market failure. Addressing these barriers to uptake and correct usage requires comprehensive and on-going education campaigns for both health care providers and members of the communities, which in turn necessitate a reliable and consistent RDT supply.Furthermore, in assessing the level of acceptability of RDT using the acceptability score, only 2.6% of them had good level. Another study carried out in Tanzania also stated that most staff felt RDTs placed additional strain on normal operations and believed that more staff were needed to conduct the tests. [17] Most of the respondents said RDTs were ever available at their facility of work, and the rate of use is high, however, some health workers said the RDTs were unreliable. This is similar to the suggestion in a study in Enugu, Nigeria which stated they do not trust the results despite the fact that RDTs have been found to have a sensitivity of 90.6% and a specificity of 95.9% in Nigeria. [21]In another study conducted in the Eastern part of Nigeria, Health Providers and community members both recognised malaria RDTs as an important step to correct treatment, however, it was also reported that there were concerns as to the reliability of test results with symptoms being deemed more important than test results. [23] It has been noted that health workers still treat for malaria even when RDT result is negative, due to reasons such as lack of finances to conduct microscopy by patients, this is similar to a study carried out in Zanzibar. [24] In one trial in Uganda, 13/1,602 (0.8%) blood smear–negative patients who were not given antimalarial drugs developed clinical malaria over 7 days of follow-up and all 13 were detected by the health service and treated. [25] Similar findings were seen in Tanzania (3/603 [0.5%] of RDT-negative patients developed malaria within 7 days). [17]These studies indicate that withholding antimalarial therapy in febrile children with negative test results is likely to be safe and results in a considerable reduction in antimalarial drug consumption. However, most of the health workers who are still using RDTs tend to be satisfied with the results they get. This is similar to another study in Uganda where 92% of Health workers believed positive RDT confirmed malaria, whereas only 49% believed that negative RDT result excluded malaria infection. It is possible that poor technique or even poor preservation of the RDT kits could give rise to negative results which made some health workers to say that RDTs were unreliable. The source of information on RDTs was never through formal training sessions promoted by government, as it should be this was noted by Health workers who said these trainings were less frequent than should be.
5. Conclusions
- Knowledge of malaria amongst Primary healthcare workers was poor after calculating the overall knowledge score during the survey. Acceptance of RDTs amongst Primary healthcare workers was fair, this reflected in the overall knowledge score of RDTs which was also fair. There is need for regular training and retraining of health workers at the PHC level. Also Government agencies and Donors should ensure the continuous availability of ITNs, RDTs and ACTs in Public Health facilities.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML