-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2018; 8(4): 94-100
doi:10.5923/j.phr.20180804.03

Factors Associated with Birth Location among Reproductive Age Women in Ghana: A Cross-Sectional Survey
Emmanuel Amangbey1, Joshua A. Akuu2, Charles Lwanga Moandiyiem Tabase3
1Upper East Regional Office, National Health Insurance Authority, Bolga, Ghana
2Kwapong Nursing Training College, Kwapong, Kwapong-Kukuom, Brong Ahafo Region, Ghana
3Zuarungu Nursing Training College, Bolga, Upper East Region, Ghana
Correspondence to: Emmanuel Amangbey, Upper East Regional Office, National Health Insurance Authority, Bolga, Ghana.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Maternal mortality remains a major public health challenge in Ghana and among African countries, despite several policy measures adopted by the international community and national governments. While the location of delivery plays a key role in contributing to maternal deaths, several factors influence the decision to either deliver at home or in a health facility. This study examined factors associated with the choice of site of delivery in the Asunafo South District of the Brong Ahafo Region, Ghana. A cross-sectional survey of 138 women aged 18 years and or above were interviewed using a structured questionnaire. Association between predictors and the place of delivery was analysed using chi-square test (𝜒2) at 95% confidence interval. Factors with 𝑃 value < 0.05 were considered statistically significant. The results indicate that 52.2% of the women interviewed delivered at home as against 47.8% who gave birth at a health facility. Maternal age (p<0.003), marital status (p<0.001), level of education (p<0.004) and occupation (p<0.001) were found to be statistically significant to influence place of delivery. Other associated factors with birth location include traditional belief systems, convenience, cost and access to health services. The paper concludes that there should be extensive health education by all stakeholders including the Ghana Health Service, Ministry of Health regarding the benefits skilled birth attendants’ services bring to maternal health outcomes.
Keywords: Home delivery, Cross-sectional, Place of delivery, Facility delivery, Associated factors
Cite this paper: Emmanuel Amangbey, Joshua A. Akuu, Charles Lwanga Moandiyiem Tabase, Factors Associated with Birth Location among Reproductive Age Women in Ghana: A Cross-Sectional Survey, Public Health Research, Vol. 8 No. 4, 2018, pp. 94-100. doi: 10.5923/j.phr.20180804.03.
Article Outline
1. Introduction
- Maternal mortality remains a major public health challenge globally, despite several policy measures employed by the international community and the states to combat it (Tsegay, 2017). Globally, the trend of maternal mortality has been on the decline progressively (World Health Organisation, 2014). According to the WHO (2014), the total number of maternal deaths decreased by 4 percent, that is from 523, 000 in 1991 to 289,000 in 2013. Similarly, maternal mortality ratio also declined by 4 percent from 380 maternal deaths per 100, 000 live births in 1990 to 210 in 2013 representing 2.6 percent (WHO, 2014). Although, these statistics depict some progress gained in addressing the challenge of maternal mortality globally, the pace has been markedly slow and requires some extra efforts, especially in less developed countries in sub-Sahara African where little gains have been recorded compared to other countries in Asia, South America and Eastern Europe (WHO, 2014). The Ghanaian situation is considerably higher than the SDG global target of a MMR of 70 per 100, 000 live births by 2030 (United Nations, 2015). The WHO (2015) maintains that no country should have an MMR greater than 140 per 100, 000 live births by 2030, though it has already been projected that sub-Saharan Africa is likely to lag behind with respect to both the national and global targets (Nicolai et al., 2016). A major factor associated with maternal mortality is the location of delivery. Sialubanje et al. (2014) suggested that the place of delivery chosen by women is very important with health facility being the most ideal. Despite the health facility being advocated as the ideal place for delivery, many women still prefer to deliver at home. The home environment as a place of delivery in developing countries is shown to be unsafe and may have adverse neonatal and maternal outcomes (WHO, 2007). Many of the deaths that occur would be fundamentally prevented with health facility delivery assisted by skilled birth attendants (SBAs) (Kongnyuy et. al., 2009; Bhutta et. al., 2010). Several policy interventions in Ghana have been implemented to increase health facility delivery. Such policy interventions include cost exemption from the National Health Insurance Scheme and free maternity care. The free delivery in health facilities for pregnant women have contributed to uptake in health facility delivery (Penfold, 2007; Mensah, 2010). The percentage of deliveries occurring in a health facility has increased from 42 percent in 1988 to 73 percent in 2014; the percentage of births attended by a skilled provider has increased from 40 percent to 74 percent over the same period (Ghana Statistical Service, 2014). Similarly, the Ghana Statistical Service (2014) report that 90.2% of women in urban Ghana delivered in a health facility, with just 9.4% doing so at home and the rest 0.4% at “other” places outside a health facility. In rural Ghana however, 59% of women delivered in health facilities while 40.6% did so at home and 0.4% at “other” places. Previous studies have identified numerous factors which have influenced the location of delivery of women (Adadow and Mustapha, 2014; Cofie et al., 2015; Gultie et al., 2016). These studies found that reasons for health facility delivery include accessibility, good perceptions about the safety of health facility, positive attitudes towards health providers and quality of care received for facility births (Brighton et al., 2013; Shiferaw et al., 2013; Cham et al., 2005). Moyer and Mustafa (2013) identified several conditions that drive facility deliveries in Sub-Saharan Africa, including maternal, social, facility and macro-level factors. Their study highlights that maternal factors such as maternal education, parity/birth order, awareness of pregnancy risk factors, religion and cultural orientation were the most commonly studied drivers (Moyer and Mustafa, 2013). On the contrary, several factors have been noted to drive homebirths, these include cost-effectiveness, convenience, immediate family support during labour and maintaining traditional childbirth and postpartum practices (Shiferaw et al., 2013; Pfeiffer et al., 2013). Social pressure from family members, social norms, and past experiences of using traditional birth attendants (TBAs) were also contributing to homebirths among pregnant women (Magoma, 2010; Amooti-Kaguna, 2000). This paper sought to examine factors associated with the location of delivery amongst reproductive age women in the Asunafo South District of the Brong Ahafo Region of Ghana. The results of this study are relevant as understanding why women decide to choose a particular site of delivery is important for program and policy planning. The formulation of appropriate health promotion and community-based strategies to aid birth preparedness, and further improve maternal and new-born survival could be facilitated by the findings of this study. The rest of the paper is organised as follows: the methodology is presented in section two, followed by the results, discussion and implication for health policy intervention. The paper ends with the conclusion.
2. Materials and Methods
2.1. Study Setting
- This paper employed a cross-sectional quantitative technique to obtain information from selected women aged 18 years and or above, who had given birth within the last one year. The study employed this type of design because it is best suited to studies aimed at finding out the prevalence of a phenomenon, by taking a cross-section of the population (Babbie 1989). Cross-sectional surveys are useful in obtaining the overall “picture “as it stands at the time of the study. The study was conducted in the Asunafo South District of the Brong Ahafo Region of Ghana. The population of Asunafo South District, according to the 2010 Population and Housing Census, is 95,580 representing 4.1 percent of the region’s total population (GSS, 2014). The Asunafo South District is located at the southern part of the Brong-Ahafo Region and shares boundaries with the Ashanti and Western Regions (GSS, 2014). The district shares common boarders with the Asunafo North Municipality to the north and the Juabeso District to the South-West. Other adjoining districts are the Sefwi-Wiaso District in the Western Region to the South-East, and Atwima Mponua District in the Ashanti Region to the East (GSS, 2014).
2.2. Study Population and Sampling
- The study population consists of reproductive women who were aged 18 years old and or above, and should have had a live or stillbirth within the past one year prior to this study and be resident in the study area at the time of the study. Women who had abortions and miscarriages were excluded from the study. Multistage sampling technique was used to select respondents for the study. The researchers purposively selected the Asunafo South District out of the twenty-seven administrative districts in the Brong-Ahafo Region of Ghana due to proximity and the researcher’s prior research experience of the study area. Using simple random sampling technique, four communities were selected for the study. These included Kukuom, Kwapong, Kokooso and Noberka. Systematic random sampling technique was used to select houses from which households and respondents were randomly drawn. The sample interval or the skip depended upon the number of houses.
2.3. Sample Size
- A cross-section of 138 women was determined at confidence level of 95% as the sample size using a mathematical formula suggested by Cochran (1977). The sample size was calculated as, n= t2x p(1-p)/m2, where n= required sample size, t= the z score associated with the confidence level required (confidence level at 95% has a standard value as 1.96), p= the population prevalence of the attribute being studied. Thus, the occurrence rate of the attribute within the study population, m= margin of error, t=1.96, p, (90/100 x 100) = 0.90= 90%, and m=5%.
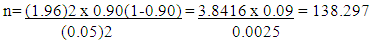 Therefore, the sample size for the study was 138 respondents. The study response rate was 100% because the researchers administered the questionnaire personally.
Therefore, the sample size for the study was 138 respondents. The study response rate was 100% because the researchers administered the questionnaire personally.2.4. Data Collection Instruments
- The study employed a structured questionnaire in collecting the data. Twumasi (2001) advocates that the questionnaire as a data collection instrument is an efficient way to collect statistically quantifiable information. The questionnaire was structured to elicit information on participants’ socio-demographics, place of delivery, reason(s) for choice of place of delivery. The questionnaire was pre-tested to check for internal consistency and absence of ambiguity and later edited. The questionnaire was administered through face-to-face interviews.
2.5. Data Analysis
- Data from the study was entered into Statistical Package for Social Scientists (SPSS). The results of the study were displayed by frequency distribution tables. Association between predictors and the location of delivery was analysed using chi-square test
 at 95% confidence interval (CI). Factors with p value <0.05 were considered statistically significant. Factors analysed included maternal age and education, marital status and occupation.
at 95% confidence interval (CI). Factors with p value <0.05 were considered statistically significant. Factors analysed included maternal age and education, marital status and occupation. 2.6. Ethical Consideration
- Ethical clearance for the study was obtained from the Asunafo District Health Directorate. Oral consent was also obtained from the study participants after thorough explanation of the rationale of the study. Participants were interviewed in private, and all the information collected from the respondents was kept confidential. The participants are not directly identified in the study.
3. Results
3.1. Participants Demographic Characteristics
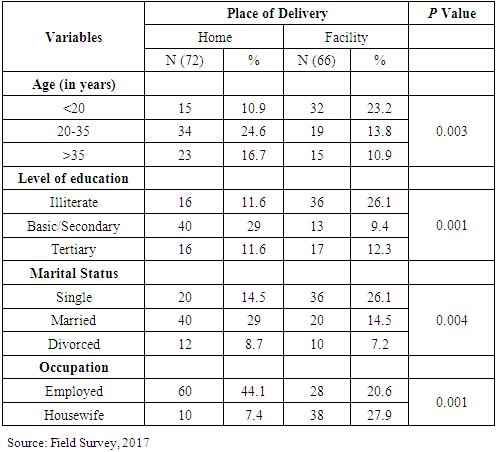
- The study involved a total of 138 participants, with 43.5% married and the remaining 36.2% were either single or divorced. Participants with age below 20 years constituted 34.1% of the total sample, whereas participants with ages above 35 years represented 65.9% of the sample respondents. A significant proportion (37.7%) of the study participants have no formal education, while 38.4% of the participants have basic or secondary education, only 23.9% were educated up to tertiary level. While 34.8% of the respondents were housewives, 63.8% of them were engaged in some form of economic activity. The table below provide detail information of the participants’ demographic characteristics.
|
3.2. Relationship between Antenatal Care Attendance and Place of Delivery
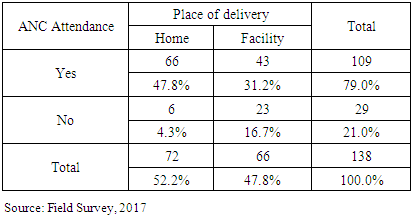
- The results in table 2 shows that majority (79%) of the respondents at least had visited a health facility for antenatal care, whereas 21% never attended health facility. However, antenatal visit did not necessarily guarantee facility delivery as 52.2% of the respondents delivered at home.
|
3.3. Decision Making during Delivery
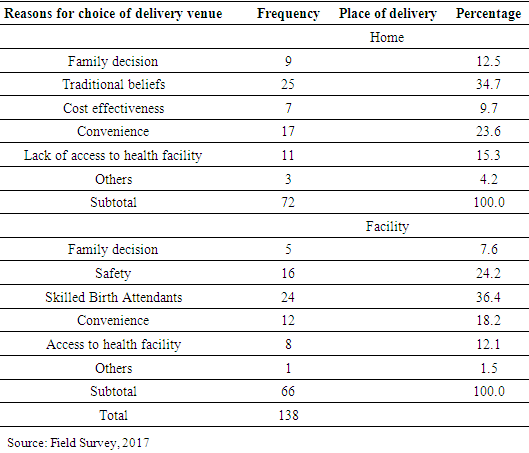
- The preference for a particular venue for delivery is influenced by multifaceted factors, 34.7% of the respondents’ preferred home delivery as a site of delivery due to traditional beliefs. Factors such as family decision (12.5%), cost-effectiveness (9.7%), convenience (23.6%), and lack of access to health services (15.3%) influenced the choice of home delivery by the study participants.With regards to health facility delivery, skilled birth attendants (36.4%) was a key determinant in deciding the health facility as a site for child birth. The role of the family (7.6%), safety issues (24.2%), convenience (18.2%), and accessibility to health services (12.1%) were cited as the choice of health facility delivery.
|
4. Discussion and Policy Implications on Maternal Health
- This paper identified factors associated with women’s choice of child birth at a health facility or home in the Asunafo South District of the Brong Ahafo Region of Ghana. The study shows that 52.2% of women during their recent child birth delivered at home. This finding supports the study of Adadow and Mustapha (2014) who report that 52.6% of women delivered at home in the Nanumba North District of the Northern region of Ghana. Factors such as traditional belief system, cost and lack of access to health services, family decisions were identified as contributors to the high rate of home deliveries. This figure is still high given the significant policy interventions by government and civil society organisations to encourage health facility delivery as it is the most ideal place of delivery. The high rate of home deliveries among reproductive women in the area has several implications on government policy intervention in eliminating maternal deaths in Ghana. Sialubanje et al. (2014) suggest that the place of delivery chosen by women is very important with health facility being the most ideal. The study further shows that majority (79%) of the respondents attended antenatal care. However, the results suggest that antenatal attendance had no influence on the choice of venue of delivery. Majority of women accessing antenatal care services could provide opportunities for health professionals to educate women on the relevance of facility delivery and provide information about the dangers of home delivery. The results are in tandem with Akazili et al. (2011) who reported that despite the increase in antenatal visits over the years, deliveries at health facilities have not increased significantly. The study provide evidence to suggest that interventions should focus on encouraging men to support their wives such as attending antenatal care (ANC) visits. The use of incentives such as preferential treatment to pregnant women who attend ANC with their husbands could increase male involvement in ANC and offer opportunities for promoting facility delivery by health professionals (Kululanga et al., 2011).Maternal age, level of education, marital status and occupation of the participants had a positive relationship with the site of delivery. Previous studies conducted in developing countries have linked marital status with home delivery (Katung, 2001; Yanagisawa et al., 2006). The age of the participants during pregnancy influenced the birth location as younger women were more likely to deliver at a health facility. Mpembeni (2007) argue that the utilization of skilled attendants at birth, showed that the proportion of women who were attended to by a skilled attendant decreased significantly with increasing age of a woman from 57.5% among women below 20 years of age to only 48.8% among women 35 years or more. It thus implies that maternal health policy interventions should be tailored in a manner that will address the specific needs of the various age categories (Mpembeni, 2007). Even though a significant proportion of the respondents are literate, the evidence depict that it is not a good predictor of location of delivery. This situation might be out of fear of traditional sanctions despite the fact that they may hold contrary opinions. Irrespective of the educational level of members of the community, as long as they reside in that vicinity, they are more likely to abide by the norms therein. Women who are literates are more likely to deliver at a health facility than those who are illiterates. This can be attributed to the fact that educated women have better awareness regarding health-related issues than their uneducated counterparts (Gultie et al., 2016). Increased decision-making power, self-confidence and familiarity with modern healthcare are attributes of educated women that could contribute to facility delivery (Gultie et al., 2016). Educated women are more likely to be aware of difficulties during pregnancy and as a result, they are more likely to use maternal health care services (Bhatia, 1995). There is therefore the urgent need for public health promotion programmes to be focused on rural, uneducated reproductive age women regarding pregnancy related complications and ultimately the need to deliver at a health facility (Kumar et al., 2013). Participants who were engaged in economic activities are more likely to choose the health facility as a delivery point since they owe resources and autonomy with regards to decision making. Women who are solely housewives lack resources and will ultimately be dependent on their partners and other family members with respect to issues relating to health (Simkhada et al., 2010).The evidence suggests that traditional belief systems have played a major role in the decision to deliver at home. Women perceive home delivery to be a social norm or practice that must be preserved (Sialubanje et al., 2015). Women entrenched with traditional belief systems and orientation perceive that since time of antiquity, their peers had delivered at home and should remain so. The decision to deliver at a health facility is therefore seen as a cover up for sins committed during the time of the pregnancy or a sign of weakness as a woman. Successful delivery at home therefore raises the moral status of a woman (Bazzano et al., 2008). The evidence further suggests that some women seem to be aware of the potential risks associated with home delivery, yet they are of the conviction that complications arising could be handled by traditional birth attendants who are perceived to be experienced compared to well-trained health professionals. Speizer (2014) highlight that perceived susceptibility has shown to be an important factor influencing health behaviour change. Government maternal health policy interventions should be tailored towards women groups that perceived susceptibility as an important determinant of their health behaviour change as these could help in improving maternal health and obstetrics outcomes (Sialubanje et al., 2015).In addition, cost and access to health services were identified as factors that contributed to the choice of site of delivery. Access to health facility for delivery care is more challenging and thus requires pregnant women and their families to plan in advance as they seek for health care (Cofie et al., 2015). Women who delivered at home noted that, it was cost effective as expenses usually incurred during delivery at a health facility were non-existent. The economic ability and access to health care is a daunting task for most women making home delivery convenient for families not economically active (Yakong, 2008). Primarily, cost generally associated with transportation to a health facility will not be needed when one delivers at home. These practices are likely to undermine maternal health policy interventions or strategies aimed at fighting maternal mortality. There is therefore the need for government policy interventions to consider rural communities and women who have no access to facility based delivery services to ensure they are supervised by skilled birth attendants (Sialubanje et al., 2015). Maternal health strategies should also take into consideration costs associated with facility delivery such as transportation fees to and from the health facility after delivery. Costs to be incurred on the day of delivery including facility delivery kits have been identified as disincentives to health facility delivery. Decision-making during delivery does not solely lie within the powers of women. The study revealed that the family, including husbands and in-laws have a significant role to play with regards to the choice of place for delivery. The evidence suggests that, Ghanaian communities are largely patriarchal in nature and as such, requires the approval of the man regarding the choice of site for delivery. To some extent, in-laws equally have roles to play as where women deliver. Men are decision makers in families, thus decisions about where, when and even if, a woman should go to a health facility for delivery mostly fall to men and in-laws (Adadow and Mustapha, 2014; Speizer, 2014). These findings emphasised the critical role decision-making and autonomy of women and others play in the use of a health facility for delivery (Adadow and Mustapha, 2014; Speizer, 2014). Women who had more autonomy were most likely to use a health facility as a delivery site. Giving women decision-making power in partnership with their spouses could raise the rate of delivery at healthcare facilities (Danforth et al., 2009). The relevance of women empowerment with regards to some family decision-making may deal with obstacles surrounding the choice of health facility delivery. Family members such as husbands and parents should also be key targets when developing maternal health policy interventions. Women who delivered at a health facility were essentially influenced by the knowledge and skills of trained medical professionals and their ability to handle delivery complications should they arise. The determinants of facility delivery in sub-Saharan African countries, linked facility births with factors such as concerns about pregnancy related complications, previous experiences of facility births, and desire for a skilled birth attendant in case of birth complications. Facility delivery was therefore perceived to be safe (Moyer and Mustafa 2013).
5. Conclusions
- This paper identified factors associated with women’s choice of child birth at a health facility or home. The study also found that maternal age, level of education, marital status and the occupation of participants had a positive relationship with the site of delivery. Factors associated with the choice of location of birth identified by this study included traditional belief system and convenience. Cost and access to health services were also unraveled as factors associated with place of delivery. The paper concludes that there should be extensive health education by all stakeholders including the Ghana Health Service, Ministry of Health regarding the benefits skilled birth attendants’ services bring to maternal health outcomes.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML