-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2018; 8(4): 81-87
doi:10.5923/j.phr.20180804.01

Knowledge, Perception and Uptake of Prostate Cancer Screening: A Cross Sectional Study at a Level III Hospital in Kenya
Beth Wanja Wachira1, Lucy Wankuru Meng’anyi2, Mbugua Gathoni Ruth1
1Department of Community Health Nursing, College of Health Sciences, Mount Kenya University, Thika, Kenya
2Department of Medical Surgical Nursing, College of Health Sciences, Mount Kenya University, Thika, Kenya
Correspondence to: Mbugua Gathoni Ruth, Department of Community Health Nursing, College of Health Sciences, Mount Kenya University, Thika, Kenya.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective: The aim of the study was to assess the Knowledge, Perception and Uptake of Prostate Cancer Screening among men attending Mathare North Health Centre. Methods: This was a Descriptive cross-sectional facility based study. The study was conducted at Mathare Health Centre in Nairobi County in Kenya among men aged 30 years and above attending the facility outpatient department. Quantitative data was collected using a structured interview based questionnaire. Data was analysed by use of Statistical Package for Social Scientists (SPSS) version 22. Results: Eighty percent (80%) of the respondents were aware of prostate cancer existence with the mass media being the major source of the information. Knowledge on various domains was low as 87% of the respondents were not aware of the symptoms of prostate cancer, 52% did not know that the disease is preventable while 71% did not know the disease is curable. Sixty four percent (64%) of the respondents were not aware of existence of prostate cancer screening services, 63% of the respondents perceived themselves as not being at risk of developing the disease while 8.8% of the respondents perceived themselves as being susceptible to prostate cancer in the future. The respondents (62.2%) held fatalistic beliefs towards prostate cancer. Only 1.3% of the respondents had undergone screening which was done more than three years preceding the study. Conclusion: The level of awareness of prostate cancer was high while knowledge on the various domains was low. There was low perception of self-vulnerability and existence of fatalistic beliefs. Consistent with the low level of knowledge, low perception of self- vulnerability, the uptake of prostate cancer was extremely low. There is need to Scale up health education to the community regarding prostate cancer to enhance knowledge, eliminate negative beliefs and increase the uptake of screening.
Keywords: Knowledge, Perception, Fatalism, Screening, Prostate cancer
Cite this paper: Beth Wanja Wachira, Lucy Wankuru Meng’anyi, Mbugua Gathoni Ruth, Knowledge, Perception and Uptake of Prostate Cancer Screening: A Cross Sectional Study at a Level III Hospital in Kenya, Public Health Research, Vol. 8 No. 4, 2018, pp. 81-87. doi: 10.5923/j.phr.20180804.01.
Article Outline
1. Introduction
- Cancer persists as the major cause of morbidity and mortality globally, with an estimated 14 million new cases and 8 million deaths in 2012. This number is projected to rise by at least 70% by 2030. World-wide prostate cancer is ranked the fourth most common cancer and the second most common cancer among men. An estimated 1.1 million men worldwide were diagnosed with prostate cancer in 2012 which accounted for 15% of the cancers diagnosed in men and the fifth cause of mortality among men. In addition to the existing burden, cases and mortality are projected to increase rapidly in line with population growth and adoption of behaviours that are likely to increase the risk of cancer mostly in middle and low income countries. [1] Prostate cancer is the number one cancer in both incidences and mortality, in Africa constituting 40,000 (13%) of all male cancer incidences and 28,000 (11.3%) of all male cancer-associated mortalities. In East Africa, prostate cancer ranks third in both incidence and mortality, and leads to an estimated 9000 (9% of all male cancers) cases and 7,300 (8.5% of all male cancer) deaths annually [2]. Prostate Cancer incidences in East Africa increased by 64.5% between 1990 and 2010 [3]. In Kenya, according to the data from the Kenya Medical Research Institute the incidence of prostate cancer rose from 9.4% to 11.4% of all cancers in Nairobi County [4]. Prostate cancer is increasingly becoming an important health burden among men in the world. In the developed world the probability of being diagnosed with prostate cancer is more than twice as high as in developing countries. This is mainly attributed to the utilization of prostate cancer screening tests in developing countries especially the Prostate Specific Antigen (PSA) test. This has resulted in lower mortality in developed countries due to early detection, while in developing countries, most cancer victims are diagnosed with late stage incurable tumours, pointing to the need for better detection programs [5]. The recent decline in cancer mortality observed in several countries was due to early detection and treatment of the disease [1]. Although early detection is an integral Component of a successful prostate Cancer therapy, a majority (87.5%) of the patients in Kenya present in hospitals with advanced disease due to low awareness and a lack of early screening services [4]. Findings from a study done in Kenya at the Kenyatta National Hospital, a major referral hospital indicated that majority of the prostate cancer patients presented in advanced stage of the disease when very little can be done in management of the patient [6]. Several factors have been associated with uptake of prostate cancer screening with low level of knowledge, low perception of self-vulnerability, low socio-economic status and fatalistic beliefs being the most cited factors. Studies done across countries have shown low levels of knowledge and uptake of screening despite high levels of awareness of prostate cancer. Studies done in Nigeria showed that men had relatively low levels of knowledge, low perception of self -vulnerability and low rates of uptake of screening [7, 8]. Fatalistic beliefs are a major barrier for uptake of screening and have been found to be more prevalent among underserved populations and black males. A study conducted in the United Kingdom associated fatalism with under-utilization of prostate cancer screening [9]. A study conducted among black Caribbean males found that there was a significant difference in perception of prostate cancer fatalism [10]. Similar findings were reported where the black men who were born in the USA had less prostate cancer fatalism compared to black men born in Caribbea [11]. Fatalist beliefs regarding Prostate cancer have been associated with low levels of education and low levels of awareness and knowledge of Prostate cancer [12]. The campaigns that support screening and creating awareness on cancer in Kenya have not been successful in targeting men. Despite much emphasis on prevention and control of cancer, more emphasis has been on cancers affecting women in Kenya, especially breast and cervical cancer with very little attention being given to prostate cancer [4]. One of the most effective intervention tools for prevention and control of prostate cancer is screening and early diagnosis [13]. However, the lack of knowledge on the disease and the low uptake of routine screening among men most at risk of developing prostate cancer escalates the problem. In Kenya 65% of men are aware of prostate cancer while only 3% have undergone screening for prostate cancer [14]. The discrepancies could also be worse in underserved populations of low socioeconomic status. Despite other studies showing low uptake of prostate cancer screening among populations, no studies have been carried out in Kenya on the underserved populations especially among the populations living in the slums. The main aim of the study was therefore to assess the knowledge, perception and uptake of prostate cancer screening among men at Mathare North Health centre in Kenya.
2. Materials and Methods
- The study was conducted in Mathare North Health centre, which is a level III Hospital situated in Nairobi County, Kenya. The facility is located in a geographically underserved area which is inhabited mainly by slum dwellers. It offers preventive, curative, and promotive services mainly to clients of low income status from the sprawling Mathare slums, Huruma, Kariobangi and Babadogo estates. The study design was descriptive Cross-Sectional. Systematic random sampling was used to select men aged 30 years and above who were attending Mathare North Health centre during the time of the study. A total of 80 men were included in the study. A structured interview based questionnaire was used to collect quantitative data which was cleaned, coded and analyzed by use of computer Software Statistical Package for Social Scientists (SPSS) version 22. Participants autonomy and privacy was observed during the process of data collection.
3. Results
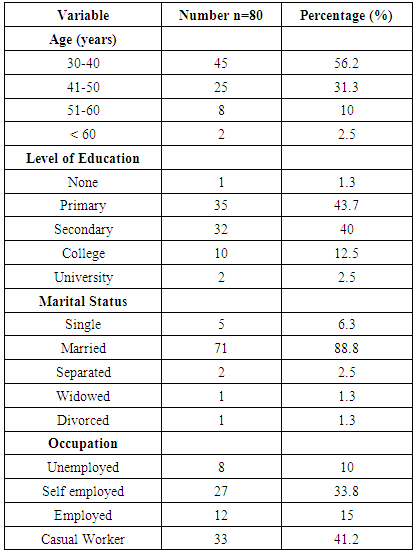
3.1. Socio-Demographic Characteristics
- The socio-demographic characteristics of the study participants are summarized in Table 1. A total of 80 men aged 30 years and above were interviewed with the mean age being 40 years among whom 88.8% were married while the rest were single, divorced or widowed. A Majority (43.7%) had only attained primary school education or lower indicating low levels of education in the area. The main occupation of most of the men was casual work (41.2%), others were self-employed with small businesses (33.8%) while 10% were unemployed. Only 15% were in formal employment.
|
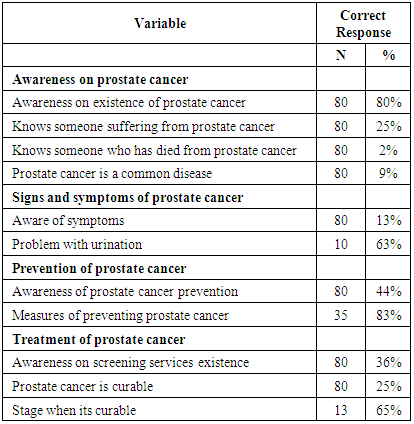
3.2. Knowledge and Awareness of Prostate Cancer
- Majority of the respondents (80%) were aware of the existence of prostate cancer however majority of the respondents (75%) did not know of anyone suffering from the disease and 98% did not know of anyone who had died from the disease. The mass media was the most cited (55.2%) source of information. A relatively small proportion (6.4%) of the respondents got information from health care workers as indicated in figure 1. This shows a gap in health education of the community by the health workers especially during visits in the hospital.
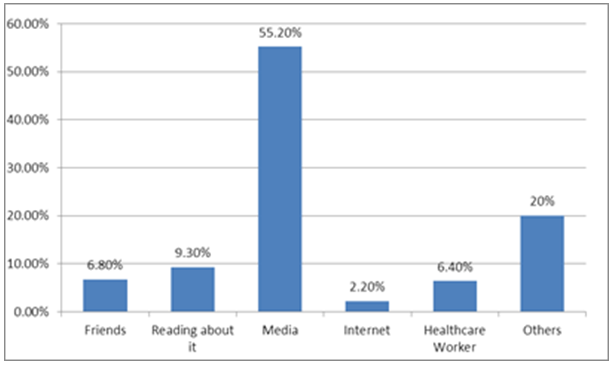 | Figure 1. Sources of information on prostate cancer |
|
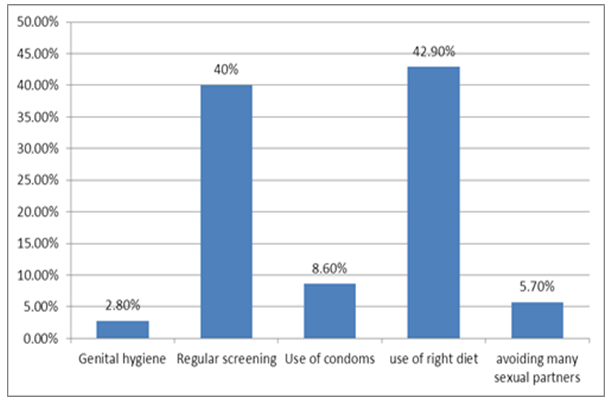 | Figure 2. Knowledge on ways of preventing prostate cancer |
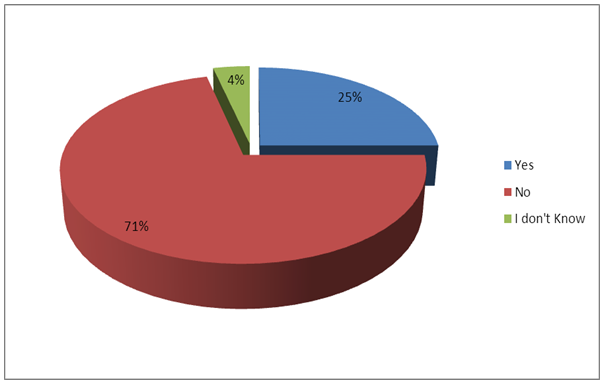 | Figure 3. Respondents knowledge on cure of prostate cancer |
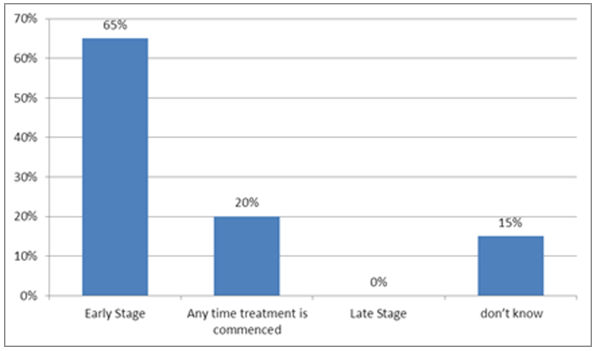 | Figure 4. Respondent's Knowledge on stage of cure of prostate cancer |
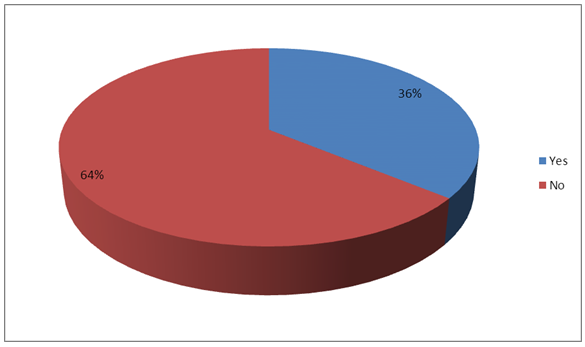 | Figure 5. Respondents awareness on prostate cancer screening |
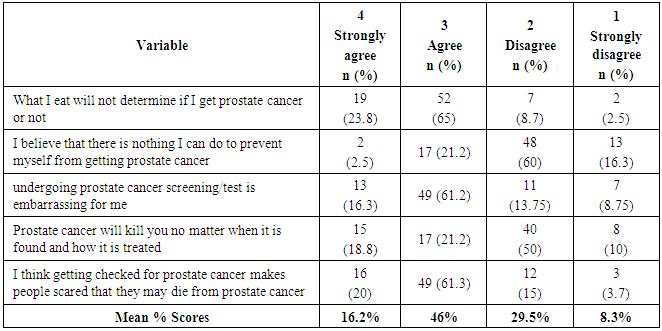
3.3. Perceptions towards Prostate Cancer
- Regarding the perception of self – vulnerability towards prostate cancer, 37% of the respondents perceived themselves at risk of developing the disease while 63% perceived themselves as not being at risk of developing the disease. Eight point eight percent (8.8%) of the respondents perceived themselves as being susceptible to prostate cancer in the future. Ninety one point two percent (91.2%) of the respondents believed that prostate cancer is not a common disease; however 99% of the respondents perceived prostate cancer as a serious disease. Regarding the respondents fear of developing prostate cancer, 23% of the respondents reported varying fears of developing prostate cancer ranging from being very afraid to some believing that it’s the will of God.The fatalistic beliefs towards prostate cancer among the respondents was assessed using a 4-point Likert scale (i.e. 1 = strongly disagree, 2 = disagree, 3 = agree, 4 = strongly agree). The overall average proportions of the respondent’s fatalistic beliefs towards prostate cancer were: strongly agree (16.2%), agree (46%), disagree (29.5%) and strongly disagree (8.3%). A total of 62.2% of the respondents had fatalistic beliefs towards prostate cancer as indicated in Table 3.
|
3.4. Uptake of Prostate Cancer Screening
- Majority of the respondents (98.7%) had never been screened for prostate cancer while only 1.3% had ever been screened as indicated in figure 6. The one respondent who had been screened for prostate cancer was screened more than 3 years ago. None of the respondents knew any person who had undergone prostate cancer screening in the last one year. This is an indication of low uptake of prostate cancer screening despite a relatively high level of awareness of the existence of the disease.
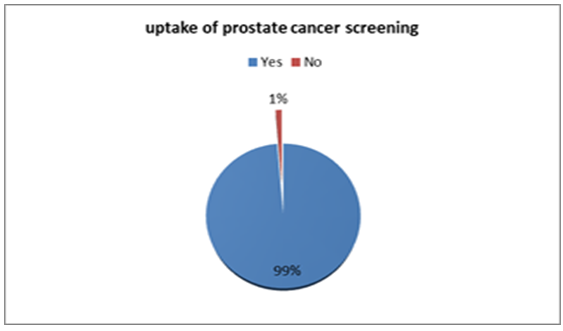 | Figure 6. Uptake of prostate cancer screening |
4. Discussion
- Findings from the study showed high levels of awareness of prostate cancer among the respondents. Majority (55.2%) of the respondents got the information from media while only 6.4% got information from a health care worker. The study findings differ from a study done in Italy which reported that majority of the men had heard about prostate cancer from their physicians which translated to more men (29%) taking up screening [15]. This is an indication that the health care providers are not actively involved in empowering of the patients visiting the health facility on the existence of prostate cancer and the importance of early screening. This is despite other studies conducted demonstrating recommendations from health professionals as the strongest association with prostate cancer screening uptake [16]. Knowledge on prostate cancer in the various domains was low with majority of the respondents not being aware of the signs and symptoms, prevention, prognosis and screening services. There were myths and misconceptions regarding prevention and prognosis of prostate cancer which shows the existence of knowledge gaps in prostate cancer that require to be addressed. These results correspond with findings of a previous study among a native urban Nigerian population with low education status which showed that a large population of men (71%) had little knowledge about prostate cancer disease including screening. [7]. Similar findings were reported among men of black ethnicity where the overall, knowledge of prostate cancer scores were low, especially in domains of knowledge of prostate cancer risk factors, prevention, management and screening [17]. There is need to scale up health education to men regarding those domains to enhance informed decision making on uptake of screening. Perception of self-vulnerability has been associated with uptake of prostate cancer screening as men who perceive themselves at risk are more likely to take up screening [7, 18, 19]. The study findings show low perception of self - vulnerability towards prostate cancer as 63% of the men perceived themselves as not being at risk of developing prostate cancer and only 8.8% of the respondents believed that it was likely for them to get prostate cancer in the future. This compares to a study in Nigeria where only 19.4% of the respondents believed they were at risk of developing prostate cancer [8]. Similar findings were reported among Chinese men where more than two thirds of the men did not perceive themselves as susceptible to cancer development in the future [20]. Fatalistic beliefs among men create the misconception that they have no control over the events related to occurrence or management of cancer. Fatalistic beliefs and fear of developing cancer are major barriers to the uptake of prostate cancer screening [12]. A significant proportion of the respondents had fatalistic beliefs towards prostate cancer. Similar findings were reported in a study done in a rural community in Kenya where 75% of the men held fatalistic beliefs towards prostate cancer and a significant number feared being diagnosed with prostate cancer. Fatalistic beliefs are also associated with intention to take up screening [21]. Fatalist beliefs regarding prostate cancer have been associated with low levels of education and low levels of awareness and knowledge of prostate cancer. [12] There is need for planning of education of men regarding prostate cancer to overcome negative beliefs that are likely to prevent men from uptake of health preventive strategies towards prostate cancer. Despite screening being a very vital preventive measure of prostate cancer, only 1.3% of the respondents had ever been screened. This is an indication that despite the high awareness on prostate cancer, uptake of screening is very low. This extremely low level could be attributed to the study area being pre-dominated by men of low socio economic status. Others studies done have shown that underserved population and black men tend to record low levels of screening for prostate cancer [22, 23]. The low uptake could be attributed to lack of knowledge of availability of the screening services as 60% of respondents were not aware of the existence of screening services for prostate cancer. Similar findings were reported in Spain where only 10% confirmed that they had ever had a PSA test with majority of those who had never been screened citing screening services being not available and their perception of the tests being not necessary [24]. Similar findings were reported in studies carried out among African men where there were screening rates of 4.1%, 4.5% and 10% in Kenya, Nigeria & Namibia respectively [7, 8, 25]. This is worrisome as lack of screening has been attributed to increase in mortality from cancer due to patients presenting in advanced stages in the health facility. There is need to educate men on the importance of routine screening in the absence of symptoms.
5. Conclusions
- Arising from the findings of the study, the level of awareness of prostate cancer among men was high with the main source of the information being mass media. Despite the high level of awareness of the disease the knowledge levels was low in various domains including the signs and symptoms, prevention and screening. Majority of the respondents had low perceived risk of self-vulnerability to the disease and held fatalistic beliefs regarding prostate cancer. Consistent with the low level of knowledge, low perceived risk of vulnerability and existence of fatalistic beliefs the uptake of prostate cancer was low at 1.3%. We recommend widespread education in the community regarding prostate cancer to improve knowledge, perceptions and uptake of screening for prostate cancer.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML