-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2017; 7(6): 123-135
doi:10.5923/j.phr.20170706.01

The Role of Mobile Health in Supporting Cancer Prevention, Detection, Treatment and Palliative Care in Low and Middle Income Countries: A Scoping Review
Dabo Galgalo Halake, Isaac Machuki Ogoncho
Department of Nursing, University of Kabianga, Kericho, Kenya
Correspondence to: Dabo Galgalo Halake, Department of Nursing, University of Kabianga, Kericho, Kenya.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Cancer is one of the non-communicable diseases with high morbidity and mortality rates, particularly in low-and-middle income countries. Increasing cancer burden is attributable to lifestyle risk factors, poor health system infrastructures, rapid population growth and ageing. These challenges are predicted to persist for years to come; thus the cancer burden is feared to become a major public health crisis hence need for innovative approaches to manage it. Though the widespread use of mobile health technologies in low and middle income countries can potentially address these challenges, evidence on mobile health use has not been fully explored. This study aim to examine the existing published and unpublished literature on the use of mobile technology-based interventions designed to support cancer prevention, detection, treatment and palliation in LMICs. The study adapted a scoping review approach using Arksey & O’Malley (2005) methodological framework. Six electronic databases; Medline, EMBASE, PsycINFO, PubMed, Web of Science and WHO Global Health Library were systematically searched for relevant studies between 1990 to 2014. The search also included additional sources from trial registers, Google, Google Scholar and reference lists. The search yielded 523 articles of which 16 were reviewed, one of these being an ongoing trial. The key findings revealed that mHealth technologies had significantly contributed to the positive outcomes in the cancer care in various contexts with all mobile technology-based features used showing improvement in care delivery. The cell phones were the common mobile device used (46.6% of the studies) followed by Smartphone (26.6%), while SMS was a commonly used mHealth feature. Mobile health interventions predominantly targeted cancer screening and diagnosis in the continuum of care, with less focus on treatment and palliation support. In conclusion, mobile health interventions have a high potential to transform cancer services in low resource settings.However, there is a paucity of evidence on mobile health interventions for cancer care. Most of the reviewed studies were descriptive, hence the need for robust studies with multidimensional focus, including control of risk factors, treatment compliance and palliative care.
Keywords: Mobile Health, mHealth, Cancer, Low and middle income countries
Cite this paper: Dabo Galgalo Halake, Isaac Machuki Ogoncho, The Role of Mobile Health in Supporting Cancer Prevention, Detection, Treatment and Palliative Care in Low and Middle Income Countries: A Scoping Review, Public Health Research, Vol. 7 No. 6, 2017, pp. 123-135. doi: 10.5923/j.phr.20170706.01.
Article Outline
1. Introduction
1.1. Overview of Cancer Burden
- The burden of non-communicable diseases (NCDs) particularly in low and middle income countries is growing rapidly with prevalence estimated at 80% [1]. Among the most rapidly growing NCDs is cancer causing high morbidity and mortality worldwide [2]. It accounts for 8.2 million deaths, 14.1 million new cases and 32.6 million people are living with diagnosis of cancers in 2012 [3]. The International Agency for Research on Cancer (2014) and WHO (2014) estimate that more than 60% newly diagnosed annual cases as well as 72% of the world’s cancer mortality occurred in Low and Middle Income Countries (LMICs) particularly in Africa, Asia, Central and South America. These countries also have lower survival rates due to late diagnosis hence presentation of cancers at advanced stage. The global economic cost incurred due to disability or death caused by cancer is approximately 900 billion US dollars which exceeds that of heart disease [6].Moreover, many low and middle income countries are experiencing epidemiological transitions whereby they are facing a double burden of infectious and chronic diseases [7]. This epidemiological shift has been attributed to a number of factors including progressive globalisation and unplanned urbanization which are aggravating lifestyle risk factors for cancer. With the rapid population growth and ageing, cancer catastrophe is predicted to become crisis soon especially in LMICs with projected upsurge of global new cancer cases from estimated 12.7 million cases in 2008 to 20.3 million new cases by 2030 while global cancer-related deaths are projected to rise from 7.6 million in 2008 to 13.2 million by 2030 [1]. Cancers affect a population’s health by placing considerable burden on the fragile health systems of developing countries as well as destroying the quality of life of patients and their families. Although, LMICs bear most of the cancer burden currently, health systems in these countries are ill prepared, less equipped and resource-constrained to face this challenge [8]. Health care systems in the majority of LMICs are fragmented, under-staffed, under-funded and with competing priorities such as tackling infectious diseases [9], hence less or no attention is given to chronic diseases like cancers both by the government and donor agencies. This poor health care infrastructure coupled with weak referral systems have a detrimental impact particularly on rural populations with already disadvantaged disparities in terms of allocation of resources and inaccessibility of health services due to distance [10, 11]. Rural populations often experience late diagnosis of cancer cases and significant suffering exacerbated by the paucity of the palliative care services available.In addition, many populations in the low resource settings have significant unmet needs for health information. There are communication gaps between patients and health care providers including consultation breakdowns between rural-based health personnel and experts, and poor patient follow-up and management.In most LMICs, decreasing the overall burden of cancer by reducing health care costs, addressing communication gaps and enhancing access to care to save lives remain a key priority in health service delivery.Prevention, early detection and early management of cancer through integration with ever evolving technology innovations is being advocated by the WHO and ITU (The International Telecomunication Union) particularly emphasising on ubiquitous use of mobile health technology in low resource settings [12].
1.2. Background of Mobile Health
- Mobile health (mHealth) is defined by the Global Observatory for eHealth (GOe) as a subcomponent of electronic health (eHealth) for medical and public health practice supported by mobile communication devices such as mobile phones, personal digital assistants (PDAs) and other wireless devices [13]. In some literature the term ‘mHealth’ has been used interchangeably with ‘telemedicine’ and ‘telehealth’ (which are also part of eHealth for providing clinical health care at a distance), in this review it refers to mobile and wireless technologies. The evolving mobile phone and wireless technologies have the potential to change the face of 21st century healthcare by providing a new dynamic platform for supporting health service delivery in cost effective, scalable and sustainable ways [13], specifically in resource limited settings. The International Telecommunication Union (ITU) estimated mobile phone subscriptions to be about six billion at the end of 2011 across the globe with 70% of these subscribers living in LMICs [14]. The widespread mobile network coverage in LMICs transcends other essential infrastructure such as roads, health facilities, electricity and fixed line phones [15]. This presents immense opportunities that can be harnessed to overcome structural barriers and resource limitations to provide cancer care services. With the advent of advancing mobile communication technologies in recent years, the scope of mHealth is not only limited to basic cellular phones but also expanding to encompass more powerful tools like Smartphone and tablets [16]. Mobile phone technologies used in health care delivery range from basic cell phone functionalities like short messaging service (SMS), standard voice call, and multimedia messaging service (MMS) to more complex forms such as global positioning system (GPS), general packet radio service (GPRS), third and fourth generation mobile telecommunications (3G and 4G systems), Bluetooth technology [13] as well as Geographic Information System (GIS) and Smartphone applications with recent technological advancement. These mHealth innovations enable linkage of patients to health professionals or health care system facilitating sharing of health information in different settings and population in right time and places.Currently, mobile and wireless technologies are used to support a wide range of public health activities within the health sector. There has been a rapid uptake of mobile communication technologies within the health sector taking advantage of its expanded networks as well as their availability, accessibility, innovativeness, cost effectiveness, real-time access to information and portability qualities [14]. Although, the mHealth field is still in its emerging phase in many LMICs, it has shown the ability to transform health care systems through its potentials of enabling spread of health information and services to hard-to-reach population and promoting a shift toward consumer-centered health care delivery [16]. The emerging epidemiological shift of disease burden in LMICs has compelled researchers, policy makers and donor agencies to form partnerships with governments to leverage mobile communication technologies to build interventions. The WHO and ITU in conjunction with the Global Adult Tobacco Surveillance system have launched mHealth initiatives in 17 countries to capture data on tobacco use [12] to prevent and manage its risk factor which also causes rise of cancer burden in LMICs. Similarly, there is also ongoing applications of mHealth technologies specifically to oncology field in LMICs such as the Communication in Oncologist-patient Encounters (COPE) project for enhancing patients and oncologists interaction via mobile internet tools and Africa Oxford Cancer Foundation’s (AfrOx) interest in improving cancer care in Africa by use of mobile technology [17]. In addition, some of the international cancer mHealth programme collaborations have been initiated in India, for example partnership between Narayan Hrudaya-laya Hospital and Harvard/MIT was formed to implement the Sana mHealth platform for oral cancer screening [18], Stanford University researchers developed Oscan device based on camera phone to detect oral cancer at early stage and refer patients to dentists [19]. Clearly, these projects have exhibited the potentials of mHealth applications to oncology to lessen its burden by bridging the gap between the health systems, care providers and clients although most of them are still in their pilot phase which need to be scaled up.
1.3. Justification of the Scoping Review
- Despite the prospects of mHealth for cancer care in addressing its burden particularly in LMICs, a rigorous evidence-based study on its effectiveness and use is limited. The existing literatures related to mHealth for supporting cancer are mostly in developed countries while a few exist in LMICs which range from expert opinions, case surveys about the applicability and feasibility of mobile technologies to cancer context in resource-poor settings [17, 20]. While a limited number of systematic reviews of mHealth addressed non-communicable diseases and their associated risk factors, none focused exclusively on gathering the evidence available on cancer in LMICs. Systematic review of mHealth for NCDs in sub Saharan Africa [21] also identified the need for a more comprehensive evidence-based approach to address the multiple gaps which exist across the continuum of care such as detection and diagnosis, referrals, point of care service coordination. Systematic reviews on smartphone applications in the domain of care, prevention, detection and management for cancer in high income countries [22] have not led to similar reviews in LMICs and the evidence on the use of mobile technology for cancer remains undocumented. This review seeks to explore the findings of a range of relevant literature in order to summarise, identify the gaps in the current evidence on mobile technology for cancer in LMICs and provide future directions for research. Since this is a fairly new research area, a scoping review methodology by Arksey & O’Malley, (2005) was employed.
1.4. Aim and Objectives
- The study aim to establish the extent and nature of the published and grey literature on the use of mobile health-based technologies for cancer prevention, detection and management in low-and-middle income countries. It is guided by the following objectives:Ÿ To determine the extent, range and nature of evidence available on how mobile health interventions are used in cancer context in low and middle income countriesŸ To map out and summarise the current state of evidence on mHealth for cancer in LMICsŸ To identify major research gaps and emerging themes from the mHealth literature for cancer in LMICs. Ÿ To make recommendations for future research, practice and policy related to mHealth for cancer in LMICs.
2. Materials and Methods
2.1. Framework of the Scoping Review
- This review was based on the framework developed by Arksey & O’Malley (2005) [23]. The framework allows for mapping of key concepts underpinning a specific research area, the main sources and types of evidence available, and can be undertaken as standalone projects, especially where an area is complex or has not been reviewed comprehensively before [24]. Arksey and O’Malley’s methodological framework for conducting a scoping review has 6 stages which were adopted for this review: (1) identifying the research question; (2) identifying relevant studies; (3) study selection; (4) charting the data; (5) collating, summarizing, and reporting the result using both the descriptive numerical and thematic analysis; and (6) a consultation exercise which is an optional stage [23]. This review aimed at answering the following research questions: what are the extent, range and nature of evidence available on the use of mHealth interventions to support cancer care? What are the current states of evidence on how mHealth technologies are being used and for what purposes are they used in cancer context? What are key emerging themes from the evidence and major research gaps in the literature? What recommendations can be made for the future research, practice and policy?
2.2. Search Strategy for Identifying Relevant Studies
- Relevant articles are identified systematically through a search strategy using appropriate search terms and keywords. Appropriate electronic databases and additional sources for both published and unpublished literatures on cancer related to mobile health interventions in developing countries were also identified. The search queries were constructed by dividing the review topic into the following three domains: terms related to (i) ‘mobile communication devices’ or ‘mHealth technology interventions’, (ii) ‘cancer’ and (iii) ‘low-and-middle income countries’ or ‘developing countries’ or specific country names from the list obtained from the World Bank, (2013) [25]. The search terms used to structure the search strategies were developed from identifying their subject headings (Medical Subject Headings-MeSH) for selected databases and free text words related to the components. In addition, generic terms used by other researchers [26], [27] were adapted to broaden the search strategy. The set of terms constructed in each domain were combined with Boolean operators ‘OR’ to retrieve any of the term it separates and all the domains were joined by conjunction ‘AND’ to obtain all the words it separates in the search. Restrictions applied to each database include articles published between time span: 1990-2014 since the first mobile health technologies-based interventions commenced in early 1990s [28], language restriction was not applied. Sources of literature (published and unpublished) were searched comprehensively regardless of the study designs, type of participants, specific cancer case or mobile health technology-based interventions to ensure all the relevant articles were obtained. The literature searching was performed iteratively in two stages to comprehensively identify all the articles which meet the inclusion criteria. Firstly, systematic literature searching was carried out in 6 electronic databases selected based on the multidisciplinary nature of the articles they contain using the search strategy developed and adapted to suit each database.Additionally, to make the search more extensive and capture all the relevant articles, other additional sources were searched which include: hand searching for key journals, trial registers for ongoing and completed studies, reference lists and citations of included studies as well as grey literature sources. Detailed descriptions of these sources are as follows:
2.2.1. Electronic Databases
- The following online databases were searched: MEDLINE, EMBASE, PsychINFO, WHO Global Health Library (limited to regional indexes), Web of Science and PubMed. All the eligible articles were identified using the subject headings and keywords which form part of the search strategy appropriate for each database. The search results were downloaded to reference manager (Endnote) for screening and assessing their eligibility according to the inclusion criteria by reviewing the title, abstract and full-text of relevant articles.
2.2.2. Additional Sources of Literature
- Besides, searching electronic databases for the relevant literature, published and unpublished articles were identified using the following sources: key journals were identified through reference lists of included studies and by consulting the experts in mobile health. They include the Journal of Medical Internet Research (JMIR), Journal of Telemedicine and Telecare, Asian Pacific Journal of Cancer Prevention, BioMed Central (BMC cancer) and Journal of Biomedical and Health Informatics. Further scanning of reference lists of the included studies was performed to identify supplements of relevant literatures. Recently completed, ongoing and unpublished trials were also searched in the specific trial registers. The following trial registers were searched: clinicaltrials.gov (http://www.clinicaltrials.gov), the metaregister of controlled trials (www.controlled-trials.com/mrct) and WHO International Clinical Trials Platform Registry (www.who.int/trialsearch). These trial registers were selected since they contain international trials classified according to the regions and countries where they are being conducted making even those eligible trials in developing countries available for selection. Apart from some of the relevant conference papers retrieved through Web of Science and Medline, other specific sources sought for grey literature include: ProQuest Dissertations and Thesis Full Text database, Google and Google Scholar which are identified to be relevant websites [29]. Scanning of these sources was done using the title search terms described in the search strategy.
2.3. Study Selection
- Literatures obtained from the search strategy were screened against the following inclusion and exclusion criteria to assess their eligibility:
2.3.1. Inclusion Criteria
- Ÿ Type of participants: mHealth studies for cancer involving health care providers/ community health workers, clients/patients, informal or family caregivers of the cancer patients regardless of their age, sex, socio-economic status.Ÿ Type of interventions: All the mHealth interventions aimed at supporting cancer prevention, surveillance, detection/diagnosis, treatment and palliation.Ÿ Type of mobile technology: Any mobile communication device or wireless technological features supporting delivering of cancer care in LMIC ranging from but not limited to SMS, voice calls, applications, MMS, GPS (Global Positioning System).Ÿ Type of mobile communication devices: all mobile or wireless digital devices ranging from cell phones, smartphones, personal digital assistant device, GPS tracker, tablet computers.Ÿ Type of settings: All countries listed by the World Bank (2013) in the categories of low and middle income countries including low-income, lower middle income, middle income denoted by the Gross National Income (GNI) per capita ranging from below $1,045 to less than $12, 746. Both the community and health care settings were also included in the review. Ÿ Type of studies: All study designs such as experimental studies (randomised controlled trials), observational studies (cohort, case control, cross sectional, ecological), descriptive research (case reports, case series), reports, expert opinions, conference proceedings, books were included.Ÿ Type of cancers: All cancers targeted by mHealth interventions across the continuum of care were considered without restricting sex or age of the cancer patients.
2.3.2. Exclusion Criteria
- Ÿ Studies targeting non-human such as those using model to demonstrate or test the designed mHealth interventions.Ÿ Mobile health interventions for supporting cancer conducted in high income countries.Ÿ mHealth interventions delivered through non- mobile communication devices or wireless technology like desktop computers, facility-based telemedicine.Ÿ Studies using mHealth interventions for other diseases such as chronic or communicable diseases.
2.4. Study Screening
- Articles resulting from the search of the literature sources were managed using endnote (reference manager) and duplicates were removed. Initially, articles were screened by titles and abstracts to identify those that potentially meet the inclusion criteria explained above. Relevant articles suitable for the inclusion were retrieved to assess full-text for eligibility. These literatures were further assessed repeatedly against the inclusion criteria to ensure that they were eligible to be included in the review.
2.5. Data Extraction
- Specific data were retrieved from the included studies using a customised data extraction form. This was an iterative process in which the data extraction form was being updated and refined as familiarity of the relevant studies was gained due to heterogeneity of the included studies. After piloting the initial data extraction form with 5-10 of the studies and amendment of format made in the process to gain consistency of the data extracted, a final extraction form was developed.
2.6. Collating, Summarizing and Reporting the Results
- Findings from different studies were sequentially gathered, their contents analysed numerically to determine the extent, nature and distribution of the included studies and thematically to identify recurring themes from the data and establish the breadth of the evidence to present them in a narrative form [23]. However, this approach has been criticised due to a lack of methodological detail on how the results were produced [30]. Therefore, this review adapted the three distinct steps recommended by Levac et al. (2010) in order to provide the findings in a systematic and rigorous manner. These steps include: Analysing the data using a descriptive numerical summary analysis and thematic analysis; reporting the results and outcome of the study through charts, tables, narrative showing the strengths and gaps in the evidence; providing the overall implications of the findings for future research, clinical practice and policy.A descriptive numerical analysis was carried out using a SPSS version 21 while the content of each study was critically analysed to identify the recurring patterns of themes emerging from the evidence. The results are presented in tables and chart forms, alongside a narrative account to describe the findings of the study.
3. Results
- Sixteen studies were selected from different sources of literature based on the study settings, context of care, population, designs, and data presentation in the form of tables and charts. However, one ongoing study was not included in the analysis but its key characteristics were described in this review. Hence, only fifteen studies with full report were considered in the analysis and fully discussed. The following sections provide details of the included studies.
3.1. Description of Literature Searching Process
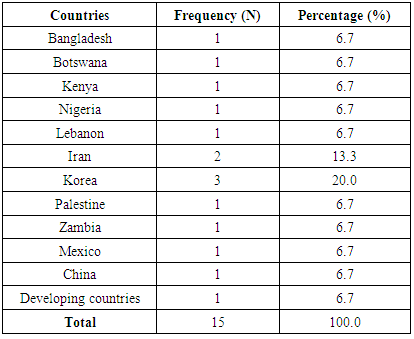
- The initial search of electronic databases and additional sources of literature yielded a total of 523 articles. Of these, 20 articles were duplicates and removed from further review. The remaining 503 papers were screened by reading titles and abstracts and 445 of them did not meet the inclusion criteria hence excluded. Further eligibility assessment was carried out on the 58 full-text articles using the inclusion and exclusion criteria and 43 studies were excluded for not meeting the inclusion criteria hence 15 articles were retained with an addition article from an ongoing trial. An elaborated flowchart which illustrates the different search strategy processes taken for literature searching is shown in figure 1 below:
 | Figure 1. Study flow diagram showing literature searching process |
3.2. Characteristics of the Included Studies
- Studies included in this review were carried out in various settings in low and middle income countries. Of the 16 studies used, 14 papers were published in journals; one was a book chapter, while the other is an ongoing study. The on-going study was an interventional RCT being conducted in China with the aim of investigating the effect of real-time monitoring of cancer pain and quality of life using a mobile phone-based cloud computing concept system application.
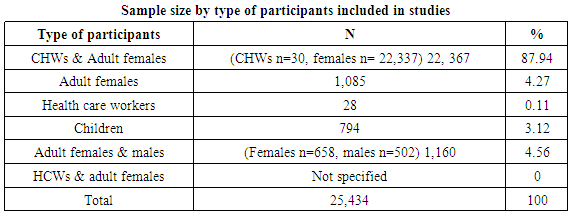
3.2.1. Trends and Geographical Settings of the Included Studies
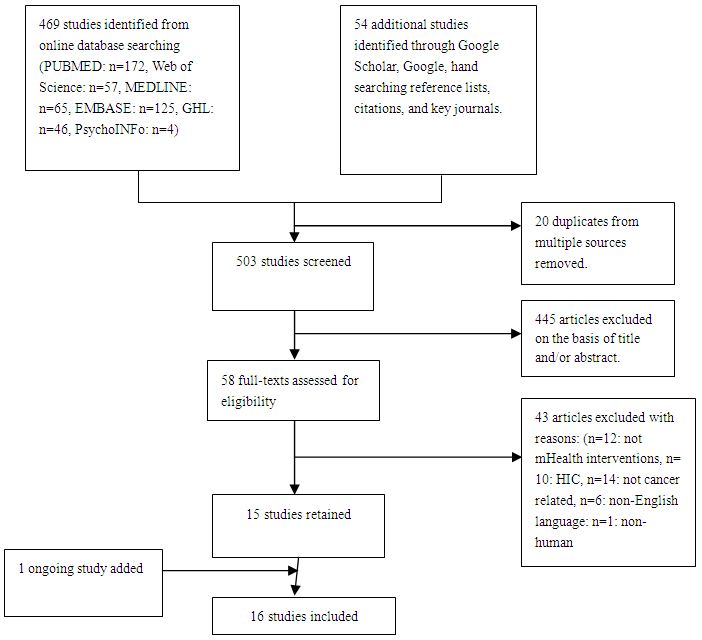
- The search strategy covered the period from 1990 to 2014 and publication dates ranged from 2007 to 2014. Figure 2 below shows the trend of the publications of the studies included in the review:
 | Figure 2. Time trends of included articles |
|
3.2.2. Study Designs of the Included Studies
- Diverse methodological approaches were employed with 20% (n=3) using cross-sectional design [31-33], feasibility studies [34-36] accounted for another 20% (n=3), randomised controlled trials [37, 38] encompassed 13.3% (n=2). Others studies utilised case control [39], cohort [11], secondary data analysis [40], ecological method [41], comparative study [42], single center report [43] each accounting for 6.7% (n=1) while one article [44] was from a book so it did not use any design.
3.2.3. Aims of the Included Study
- The included studies have various aims, with many overlapping in their objectives targeting different type of cancers and mHealth interventions. Generally, most of the studies evaluated the effect of mHealth interventions across the continuum of cancer care; For cancer prevention purpose, the majority (n=5) of the studies [32-34, 37, 42] assessed the use of mHealth interventions designed for health promotion and education through patient reminders on self-examination, empowering health care workers and patients to access cancer information. Three studies, [38, 39, 44], also evaluated effectiveness and accuracy of mHealth interventions for cancer screening and diagnosis through appointment reminders to patients, linking on-site health care workers to off-site experts. Another two, [35, 36], investigated the feasibility of mobile technology in data collection and information sharing between patients and health care workers. Effectiveness of mobile technology-enabled interventions for supporting consultation for cancer diagnosis and follow up were assessed by two studies [11, 31]. Two studies, [40], [41], investigated the feasibility of the use of mobile devices for analysing spatial and temporal data on cancer mortality, risk factors and cancer patterns.
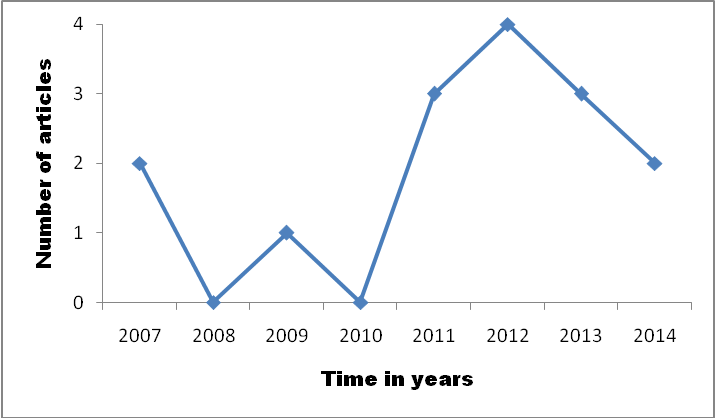
3.3. Study Population Characteristics
- Since all the reviewed studies were targeting several populations, six categories of participants were formed according to the similarity of the target population. Most of the studies 53.33% (n=8) involved adult females while a few involved Health Care Workers (HCWs) 13.33% (n=2) and children 6.67% (n=1) as illustrated in figure 3 below.
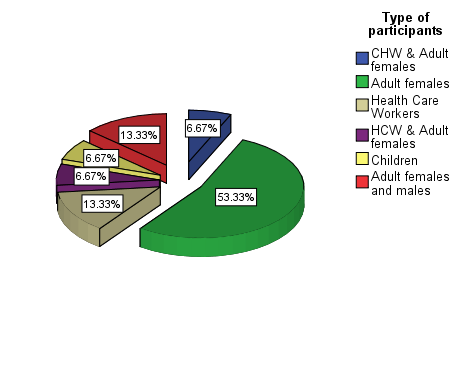 | Figure 3. Type of participants of included studies |
|
3.4. Findings on the mHealth Interventions Use in the Included Studies
- The studies utilised mobile health interventions in a variety of ways using diverse mobile communication tools with their respective technological features targeted to support cancer services delivery as follows:
3.4.1. Mobile Communication Tools Used
- Majority (46.6%) of the mHealth interventions were delivered by cell phone, followed by Smartphone (26.6%). The least reported by the studies were cell phone camera, digital geographic information system tool and personal digital assistant.
3.4.2. Mobile Technology Features Used to Support mHealth Interventions
- A number of studies (n=3) reported the use of smartphone applications for data collection during interviewing clients for cancer screening [37], encouraging and modifying breast self-examination behaviour [45] and collecting data on sleep disturbance for patients receiving chemotherapy [36]. In another study, Short text Message Service (SMS-text) reminders were sent to clients to invite them for screening [38]. In addition, other studies done were the use of text messaging by rural women to receive breast cancer prevention information [33], and comparative study on the effect of teaching about breast cancer by sending SMS versus the traditional learning method among the gynaecology residents [42]. The use of mobile telemedicine (using mobile phone camera and Multimedia Messaging Service-MMS) by health care workers for prospective case control study to screen patients for cervical cancer and in consultation with experts was done [39]. The use of mobile phones internet in accessing information on cancer treatment and management was also explored [32]. The use of voice calls was investigated by two studies [11], [31] one study investigated its effectiveness in increasing communication between cancer patients and the health care providers in medical care follow-up and another assessed the accuracy of diagnosis done via phone calls to HCWs by the clients in which patient referrals were made. The potential of GIS software in geographical cancer patterns tracking and mapping of the risk factors of cancer mortality were assessed in two studies [40, 41]. A feasibility study adopted personal digital assistant in home hospice information system for collecting, recording and transmitting data to health centre information system to enhance quality of end of life point of care services [35]. One study included had multifaceted mHealth technological features like text messaging, photo transmission via email for distance consultation to off-site experts so as to provide decision support on diagnosis and referral as well as patient education [43]. In a book chapter on breast and gynaecological cancers, a general description of how mobile telemedicine are employed in screening and diagnosis of cancers in the developing countries was captured.
3.5. Thematic Areas Identified from the Studies
- The findings were clustered according to six themes arising from the aim of the mHealth interventions designed to improve cancer care services as follows:
3.5.1. Cancer Prevention and Awareness
- Three studies [33, 34, 42] reported the use of mobile technology based interventions designed to promote awareness of cancer for prevention purpose. One of which reported a higher prevalence of clients who preferred receiving text messages on cancer prevention information was higher than cell phone calling by 16% (36 vs. 20%) [33]. Another study reported moderate increase of 8.9% (62.2% to 71.1%) on frequency of clients using smartphone applications and educational video for practising breast self-examination [45]. The effectiveness of mobile learning by receiving the learning material on breast cancer through SMS was significantly higher compared to paper-based method in the study conducted among gynaecology residents [42].
3.5.2. Cancer Screening and Diagnosis
- Four studies [38, 39, 43, 44] reported the use of mHealth interventions in supporting cancer screening and diagnosis with one study targeting other multiple components of care like patient education, consultation and medical documentation of care [43]. Among these studies, a single center report showed that multiple features (SMS, internet use, cameras) of mHealth technologies had facilitated monitoring and evaluation of HCWs performance by supporting rapid access to off-site experts for consultation on diagnosis, continued education of both HCWs and patients as well as record keeping [43]. Another study described different components of mobile technology enabled telemedicine which demonstrated potential role of mHealth in supporting screening and diagnosis of breast and gynaecological cancers in LMICs [44]. A study on accuracy in diagnosis using mobile telemedicine [39] noted very good agreement between the remote and expert diagnoses using photograph of the cervix readings.
3.5.3. Treatment Compliance and Management
- One study [32] reported the level of mobile phone internet use as compared to computer internet on management of cancer. There was a higher level of mobile phone use to get information about cancer management (96.5%) i.e. medication reminder alerts, booking appointments, consultations and to access health education messages to computer internet.
3.5.4. Data Collection and Support Tool for Health Care Workers
- Three studies [35-37] demonstrated the effectiveness of the mHealth technologies in data collection to guide in clinical decision-making process. Of the three studies, RCT showed the efficacy of smartphone application in guiding interview process and recording data for monitoring clinical appointment adherence of patients after clinical breast examination ,whereby a significant difference of 20% (63% vs. 43%, p-value<0.0001) was observed between the intervention and control arms [37].Another study also found 45% compliance rates reporting of sleep disturbance symptoms by patient receiving chemotherapy via smartphone applications which was seen to be feasible method of data collection [36]. In addition, feasibility of PDA-based home hospice information system demonstrated effective management of patient information which resulted in saving of 8.5 minutes (from 19.2 to 10.7 minutes) in nursing record entry time and improvements in quality of point-of-care services [35].
3.5.5. Consultation, Referral and Follow-up
- The findings of two studies [11, 31] showed the effectiveness of mobile technology in improving communication between the health care provider and patients. This had been demonstrated by a cross sectional study which found breast consultation service in which women make inquiries by calling medical specialists to be highly effective in making diagnosis [31]. Additionally, the other study reported the effectiveness of mobile communication between patients and health care providers in medical follow-up whereby increased clinical appointments attendance were noted in those who called the oncologists than patients who did not while there was decreased level of cost of travel and delayed referrals [11].
3.5.6. Cancer Patterns Tracking and Mapping of Risk Factors for Health Care Planning
- Bailony and colleagues applied a GIS software to analyse childhood cancers using a cancer registry in Palestine. This study reported a clear identification of geographical patterns of cancer incidences and health care accessibility using the GIS software [40]. The GIS spatial techniques also established a significant association between environmental risk factors and cancer mortality in China. [41].
4. Discussion
4.1. Summary of Key Findings
- This scoping review provides useful insights into the current state of evidence on how mobile-health technology-based interventions were used to support cancer care in the developing countries. Overall, the results of this review demonstrate that mobile health technology significantly contributes to positive outcomes in the cancer care context and is a promising field for supporting cancer care service delivery. The existing evidence showed considerable diversification in terms of the study methodologies, mobile communication devices and mobile technology features, the aims of the interventions, targeted population and type of cancers.
4.2. The Current State of Evidence
- This review revealed that most mHealth studies focusing on cancer care were descriptive with a few experimental studies. Most of the studies demonstrated how the use of mobile communication tools have addressed various challenges in cancer care service delivery.In addition, most of these studies on mHealth applications to support cancer care were cross-sectional and feasibility studies, further pointing out the paucity of experimental studies in this area. Similarly, authors previously noted the insufficiency of studies, especially the trials of high methodological quality in the field of mHealth in low resource settings [21, 26]. The most targeted population in these studies were adult females hence mHealth technologies were mainly tailored to support interventions related to cancers affecting females specifically breast and cervical cancers in LMICs settings. This finding reflect the effort of mHealth interventions to address gender disparity due to socio-cultural barriers to access health care services by women in the underserved populations which was also highlighted in a study done in Bangladesh on breast cancer outcomes [46]. The particular contexts of mHealth initiatives delivery were commonly carried out at primary and secondary levels of care, both accounted for 80% (12 studies) while tertiary level implementation of these projects was minimal (13.3%) in the present study. This suggests that mHealth interventions for cancer management are well positioned to support provision of primary care services to those residing in the remote regions. Although mobile communication tools including smartphone, cell phone, PDA and GIS-enabled devices were used to achieve delivery of cancer care services, most of the studies used cell phones to support their interventions. This is highly consistent with the fact that the cell phone is ubiquitously used as compared to other mobile devices like smartphone in low resource setting [47].With advent of smartphones in low resource settings, the use of smartphone applications were identified by some studies and its great potentials for supporting multiple interventions were well demonstrated [37]. Recent clinical trials conducted in Madagascar [48] as well as Kenya [49] reported feasibility of smartphone image application for cervical cancer screening as an alternative colposcopy.Moreover, the increased adoption of smartphone in LMICs mainly by health workers for mHealth interventions due to its advanced features such as web browsing, GPS navigation, efficient voice and data transfer systems was observed [50]. However, among the poor population, an expansive use of basic cell phone was reported [51]. In the studies reviewed, Short Message Service (SMS) was the leading feature among the mobile technologies used while smartphone applications (Apps) and voice calls followed in the utility ranking. Indeed, text messaging has been recognised to be the most accessible feature for supporting mobile phone-based health interventions irrespective of the setting [52, 53]. In contrast, voice messages or phone calling over text messages were cited to be advantageous for illiterate populations and also when considering confidentiality and privacy issues [51], particularly in remote settings where males are more likely to own a mobile phones and females share with their male partners. The review also have showed SMS technical capabilities of delivering effectively a wide varieties of interventions ranging from reminders for screening appointment, clinical attendance adherence for diagnosis follow-up, dissemination of prevention and educative cancer information. The study found that nearly all the mobile technology-based features showed significant improvement of care delivery across the cancer continuum and bridged the communication gap between the clients and health care providers in wider geographical settings.
4.3. Key Themes and Gaps from the Literature
- Themes arising from these studies’ findings were grouped into 6 categories as detailed in subheading 3.5. Mobile communication devices provided a wide range of platforms for promoting or supporting prevention, detection, treatment and palliation of cancer as reported in various studies in this review. The common theme for the mHealth technology-based intervention, nonetheless, was on cancer screening and diagnosis. On the contrary, a literature review done on mobile technologies for cancer supportive care revealed that mHealth was mainly used during treatment of clients and to a lesser extent for prevention and diagnosis [54].The reviewed studies reported positive outcomes on the uptake of screening rates and the effectiveness of mHealth interventions in facilitating early diagnosis. This is a particularly important finding as early cancer diagnosis increases the chances of effective treatment and survival rates [55], thus reducing the advanced stage presentation which is common in LMICs. A number of the cancer patients in rural settings were unable to access health centres or communicate with health workers due to either geographical barrier or insufficiently trained health professionals [6]. Studies using mHealth interventions conducted in these settings have well demonstrated positive impact in resolving such barriers. For instance, a mobile health study in Botswana using mobile telemedicine (camera, MMS) for screening of cervical cancer indicated that 70% of cases remotely diagnosed using mobile phone images were fully in agreement with in-person diagnosis [39], hence promoting safe and efficient early detection of the cancer.Cancer prevention and awareness were emphasised by three studies in this review, and an overlap of this theme with screening and diagnosis phase was noted in some of other studies. Cancers can be prevented from escalating, and are treatable if detected earlier hence preventive measures are deemed to be effective [56]. In their recent article, Jay and colleagues noted that lack of a strong community-based education program for cancer prevention to raise awareness, change behaviour and inform about risk factors using culturally acceptable messaging, could lead to limited uptake of mHealth technology among patients as well as health care workers [57].It was also pointed out that accessing updated cancer information on a mobile phone cost less and accelerates communication and dissemination of information among the cancer community particularly those with limited access to computer internet [58]. Therefore, it is imperative for both health professionals and patients to keep abreast with the emerging mobile technology for quicker access to latest cancer information.Additionally, 20% of the included studies targeted data collection and used mobile technologies as a support tool for health care workers. Of these studies, accurate data entry, efficient transfer of data from point of care to health centre were reported in providing palliative services at home hospice [35]. Equally, a significant effects of an mHealth model for guiding interviews during patient navigation was found [37] while self-reporting of symptoms by patients via smartphone applications were recognised to be feasible [36]. Similarly, mini-review findings also concurred on the important role mobile devices played in providing access to accurate and timely cancer data while emphasising on importance of data privacy and security during data transmission [59]. Although, the effectiveness of the mHealth technologies in data collection was reported in a policy white paper [16], data security, confidentiality, and ownership were cited as major barriers. Thus, consideration of the ethical-legal aspects is of paramount importance when handling data in the mHealth field for cancer care. A few studies focused on consultation, referral and follow up of cancer care demonstrated that through telephone consultation, health care providers were able to make accurate cancer diagnosis and refer patients to the appropriate care services [31]. In addition, significantly effective communication between patients and oncologists using a mobile phone reduced travel cost for consultation and medical follow-up care [11]. Cancer pattern tracking and mapping of risk factors in specific geographic settings can make a major contribution to healthcare specifically for health care planning of resource allocation, policy-making in controlling risk factors and prioritising research activities. Such projects have been made feasible by GIS tool which was employed in two studies [40], [41]. Therefore, more evaluation of its effectiveness can be carried out using primary data sources.Although, mHealth interventions supporting cancer care showed significant improvement of various outcomes, there is a scarcity of evidence-based literature in the application of mHealth within the cancer context in LMICs. This is especially true for randomised controlled trials which are the best design for evaluating the effectiveness of an intervention [29]. Even though observational studies were more common than RCTs in this review, their methodological rigour was low and most of them were in pilot phase which may not be generalised to other settings. The mal-distribution of studies in low and middle countries was of concern with only 11 countries engaged in research involving mHealth studies applied in cancer context despite the escalating cancer burden. Of the varieties of studies included in this review, most were focused on cancers affecting females, while a few studies looked generally into cancers related to both sexes. Hence, mHealth interventions related to cancer affecting males were limited.The mHealth technology employed in most of the studies was one-way text messages, whereby patients receive SMS from health care workers. Thus, there was no interactive communication, and there is a lack of psychosocial support and real-time consultation between health care providers and cancer patients in this type of intervention. Nearly all the identified studies conducted in low and middle income countries, were funded by foreign countries, apart from studies in Korea and one study carried out in Kenya. This may pose a challenge to the sustainability and scalability of these studies from pilot stage. Hence, there is a gap in implementation of these projects at the grassroot level.
4.4. Recommendations for Future Research, Practice and Policy
- The evidence in this review was based on a very limited number of studies with low methodological rigour. Therefore, more studies need to be conducted to evaluate the impact of mHealth interventions on cancer care particularly more robust RCTs are needed in these settings to assess the impact of already designed mHealth tools on the quality of care. In addition, future research should also focus on examining the effects of two-way communication interventions on psychosocial support of both the cancer patients and their family support system. More emerging mHealth tools such as smartphone applications, mobile-based GIS tool should be explored in future studies for monitoring cancer patterns and prioritising equal resources distribution in health sectors. For clinical practice, mHealth features used at the point of care need further examination. Although, studies in this review showed the effectiveness of mHealth tools in data collection, description on how the collected data in terms of security and confidentiality was handled is lacking thus ethical-legal issues involved can be scrutinised. As cancer share four modifiable risk factors with the other non-communicable diseases, future studies can focus on finding out on mHealth potentials to support control of these risk factors to guide in formulating regulations or policies on control of tobacco use, alcohol and unhealthy food sales at various levels.A persistent dependence on donor funding to implement mobile health projects for cancer highlights the need for an effective transition from pilot phase to larger scalable programme using alternative government revenue funds so as to make the projects sustainable and leveraged by government initiatives.
4.5. Strengths and Limitations of the Review
- This scoping review has a number of strengths being the first in examining mHealth evidence in cancer context in LMICs. Thus its findings are valuable in advancing state of knowledge in this particular field. Another key strength is the comprehensiveness of literature searching undertaken using appropriate search terms for the selected databases and grey literature sources. This thorough search resulted into a wide variety of study designs providing broader findings. On the other hand, some limitations were noted in this scoping review. Due to the heterogeneity of the studies, developing the data extraction form was challenging. Summaries of the complex concepts arising from each study required to be extracted in more consistence and meaningful manner. Consultation of stakeholders is another optional stage in the scoping process, which Arksey & O’Malley (2005) recognised as a stage for adding more evidence to the review. However, this was limited by poor and untimely responses by some key stakeholders. In addition, most studies from LMICs are not captured in recognised journals especially because mHealth for cancer use is relatively new field. Studies which could not be translated into English were excluded from the review thus some of the potential literature might have not been missed.
5. Conclusions
- This scoping review formed the basis for a mapping of the existing literature examining how mHealth interventions have been used in various settings of LMICs. The overall results showed that there is a paucity of evidence examining the use of mobile health to support cancer care in these settings. Most of the employed mHealth technologies reported positive outcomes across the continuum of cancer care.Finally, mHealth interventions have demonstrated potential roles in addressing various challenges facing cancer care in low resource settings; hence a promising field for supporting cancer care, if research gaps identified in this review are further explored.
ACKNOWLEDGEMENTS
- The authors would like to express their gratitude to Dr. Liz Grant and Dr. Claudia Pagliari of University of Edinburgh, Centre for Population Health, UK who supervised this review and Halkano J. Boru for his inspirational guidance and encouragement during this study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML