-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2017; 7(3): 78-84
doi:10.5923/j.phr.20170703.04

Awareness and Factors that Influence Birth Preparedness and Complication Readiness among Pregnant Women Attending Antenatal Clinic in the General Hospital Calabar, Nigeria
Ubong Akpan1, Udeme Asibong2, Mabel Ekott1, Beatrice Moko3, Saturday Etuk1
1Department of Obstetrics and Gynaecology, University of Calabar Teaching Hospital, Calabar, Nigeria
2Department of Family Medicine, University of Calabar Teaching Hospital, Calabar, Nigeria
3Department of Nursing Science, University of Calabar, Calabar, Nigeria
Correspondence to: Ubong Akpan, Department of Obstetrics and Gynaecology, University of Calabar Teaching Hospital, Calabar, Nigeria.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

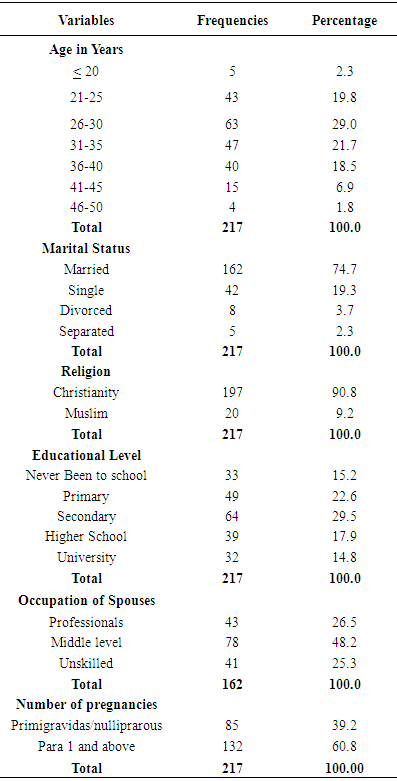
Every pregnant woman is at risk of developing complications during the period of pregnancy and immediate post delivery period. Proper birth plan/preparation and ability to recognize danger signs can help reduce the various phases of delays and ensure prompt and quality care when needed. However, various studies have shown that the knowledge and level of birth plan and complication readiness (BP/CR) among pregnant women is low. Hence this study was embarked upon to determine the impact of Focused Antenatal Care (FANC) with regard to BP/CR and suggest possible ways of improving maternal care. A questionnaire based cross-sectional descriptive study was conducted among 230 pregnant women receiving ante natal care in the General Hospital Calabar. Simple random sampling method was used to select participants. The response rate was 94.33% (217). Effective BP/CR was recorded in 33.1% of the respondents. Level of education (p<0.05, x2=33.4), partner’s support, and previous bad obstetric experiences (p=0.003) were positively associated with effective BP/CR. Lack of awareness was a major reason for poor BP/CR. There is need for male/partners involvement in care of pregnancy and antenatal education should lay more emphasis on the issue of BP/CR.
Keywords: Awareness, Birth preparedness, Complication readiness, Antenatal care
Cite this paper: Ubong Akpan, Udeme Asibong, Mabel Ekott, Beatrice Moko, Saturday Etuk, Awareness and Factors that Influence Birth Preparedness and Complication Readiness among Pregnant Women Attending Antenatal Clinic in the General Hospital Calabar, Nigeria, Public Health Research, Vol. 7 No. 3, 2017, pp. 78-84. doi: 10.5923/j.phr.20170703.04.
Article Outline
1. Introduction
- Individual birth plan is one of the goals of focused antenatal care (FANC) adopted and recommended by World Health Organization (WHO) in 2002 to promote safe motherhood. It involves arrangement made in advance by the woman and her family with the help of a skilled health provider about the birth process and possible complications during pregnancy (Kuganab-Lem et al, 2014). It has the advantage of minimizing disorganization at the time of birth or in an emergency and it also ensures timely and appropriate care (McPherson et al, 2006). According to WHO (2002), this can help improve maternal health outcomes in ensuring that women can attain skilled care at delivery.Furthermore, a study by Kabakyenga et al (2011) revealed that effective birth preparedness reduced the delays that occur when women experience obstetric complications, such as recognizing the magnitude of the complication and deciding to seek care, reaching a place where skilled care is available and receiving care from qualified providers at the facility.The Federal Ministry of Health (FMOH) in 2012 developed an oriented package for health care providers in Focus Antenatal Care (FANC) and Malaria in Pregnancy (MIP). It listed the essential elements of individual birth plan (IBP). They include the following:1) Facility or place of birth: during the period of pregnancy (antenatal care) the woman should decide where she would like to put to birth, home or health facility, and appropriate facility for emergencies. 2) Skilled care provider: It is well known that delivery outcome is better when labour is conducted by skilled birth attendants (WHO/UNFPA/UNICEF/World Bank, 1999). It is therefore important for each pregnant client to decide in advance who would likely attend to her during labour; doctor, nurse/mid- wife or any other health personnel. Women with previous caesarean section or other high risk pregnancies are expected to be supervised by a physician care giver during labour due to increased likelihood of operative deliveries (WHO/UNFPA, 2014).3) Provider/facility contact information: Information about the place of delivery, level of care, facilities for intervention should be made available to the pregnant client before onset of labour. Even within the facility, during antenatal clinic (ANC), women should be given orientation about the labour room/ward, bed-space, neonatal care and canteen, source of water supply and laboratory services.4) Transportation: A reliable and accessible transportation arrangement should be made, especially for odd hours (Ekanem et al, 2005). This would avoid delay in reaching the health facility in time of obstetric emergency.5) Funds: Source of funds either from personal savings, salaries, emergency funds, community loan schemes or peer group contribution should be ascertained. The woman should be informed of likely estimate of her delivery fees and other charges prior to onset of delivery.6) Decision making: Who make decisions especially in an emergency situation? Is it the woman, her husband, in-laws or others including the possible input from her religious leader? Several studies have shown that delay in taking decisions to seek care in time of emergency contributes significantly to maternal mortality rates (Hailu 2011 & Kuganab-Lem 2014; Thaddeus & Marine, 2004).7) Family and community support: Care for woman’s family in her absence and birth companion during labour. An older sick child may need prompt attention while the woman is the hospital. Also outcome of labour is better when there is a companion during labour (Morhason-Bello et al 2009).8) Blood Donor: The woman should know during the antenatal period or beforehand, her blood group, possible donors (walking donors). The donors should be available during the time of birth or when needed. Their blood group should be cross matched with that of the pregnant woman and certified compatible during the antenatal period in case there is need for emergency blood transfusion like severe postpartum haemorrhage.9) Danger signs/signs of advanced labour: The vital components of essential birth plan is the woman ability to recognize danger signs in pregnancy such as vaginal bleeding, persistent headache, upper abdominal pain, or liqour drainage, also signs of labour (Solomon et al, 2015). They should know when to start going to hospital.Because life threatening complications can occur during the early postpartum period, birth preparedness also includes preparing/planning for accessing postpartum care during the first week after delivery and at six weeks after recovery. WHO (2014), estimated maternal mortality ratio of 510 maternal deaths per 100,000 live births in Sub-Saharan Africa and 560 maternal deaths per 100,000 live birth in Nigeria in 2013. Since every pregnant woman faces risks of sudden unpredictable complications that could result in maternal death or injury or poor neonatal outcome due to lack of advance planning and preparation for emergency intervention (Tobin et al, 2014), birth plan and complication readiness is very essential in improving pregnancy outcomes. In view of these numerous problems and inadequate data on the issue in our locality, this research aims at assessing the awareness and level of birth preparedness and factors influencing BPCR among the pregnant women in Calabar.
2. Methodology
2.1. Study Design
- This was an interviewer-questionnaire based descriptive study conducted among antenatal women in the General Hospital Calabar.
2.2. Study Setting
- The research was conducted at the general hospital Calabar. The hospital is the only state owned secondary health facility in Calabar metropolis. The hospital renders maternal and new born care including antenatal care, family planning, delivery and post-natal services.Also high-risk pregnant cases or complications are often referred from government primary health centers in Calabar and its environment. The hospital boasts of standard operating theatre and ambulance services for essential obstetric care. Cross River State has recently adopted focused Antenatal Care (FANC) which emphasizes on individual birth plan/preparedness and complication readiness.Calabar has an area of 40km2 and a recent population projection of 431200 according to the Geonames geographical database. Calabar is often described as the tourism city in Nigeria.
2.3. Study Population
- The study involved all consenting women attending antenatal care at the general hospital Calabar during the study period. Pregnant women who had attended ante natal clinic at least twice in the hospital in the index pregnancy were recruited during the period of study. Each willing participant was required to give a written consent for the purpose of the research.
2.4. Sample Size Calculation
- In a recent study in an African country only 14.6% % of pregnant women sampled knew about birth plan and complication readiness (Morara J, 2016). The sample size was thus calculated to be 191.5 using the Leslie Kish formula with a 95% confidence interval and a sample error of 0.05. But to allow for at least 10% non-response, the sample size of 230 was chosen.
2.5. Sampling Technique
- Simple random sampling was used to select participants. The first individual for the sample was chosen by a simple balloting method and this was done by blindly picking one out of the two pieces of paper numbered 1 & 2. This individual represented the index subject for the study, and thereafter every 2nd subject was included in the sample frame systematically until the desired sample size was realized.The sample interval was determined by dividing the total number of antenatal attendants in two months (estimated population) by the sample size. The study period was two months, from 1ST September to 31st October, 2016.
2.6. Instrument for Data Collection
- Data were collected using interviewer administered questionnaire. The questionnaire was pretested for validity and reliability. The questionnaire was adopted from the safe motherhood questionnaire developed by maternal and neonatal health programme of Johns Hopkins Program for International Education in Gynaecology and Obstetrics (JHPIEGO), the affiliate of John Hopkins University, with some modification based on the aim of the study. The questionnaire has five parts. Part one: Socio-demographic characteristics.Part two: Obstetrics information. This include number of pregnancies (gravidity), number of deliveries (parity), number of abortions if any, number of living children, gestational age of current pregnancy, number of antenatal visits, obstetric complication during previous pregnancies, and place of previous delivery, neonatal complication. Part three: Knowledge and practice of birth preparedness and complication readiness. The assessment based on the number of components of BPCR listed in the introduction (FMOH 2012) which is expected to be followed by a pregnant woman during labour or emergency. Those who intended to follow at least 6 components of BPCR were regarded as “well prepared” and those who intended to follow less than 6 were regarded as “less or partially prepared”. Knowledge on BPCR was considered adequate for those who maintained at least two components among five basic components of BPCR as listed in the introduction. Part four: Knowledge on danger signs in pregnancy. Knowledge on danger signs during pregnancy, delivery, and post-delivery. Those who knew at least a total of three (3) obstetric danger signs during pregnancy, delivery and post-delivery were regarded as knowledgeable. The rest including those who did not mention anything were regarded as less knowledgeable.Part five: Facilitating factors or Barriers to effective birth plan and preparedness.
2.7. Data Analysis
- Completed questionnaire was cleaned and entered into computer excel software. The data were analyzed using SPSS version 20. Demographic information was presented in percentages and proportion. Categorical data and association between variable and test of hypothesis was done using student t-test and chi square test. The statistical significant among variable was considered at P<0.05.
2.8. Ethical Issue
- Approval was obtained from the State Ministry of Health Research Unit through a signed letter and the officer in charge of the maternity unit. Participation in the research was voluntary and information obtained was handled with confidentiality. Refusal to participate in study by any patient did not in any way affect the care patient received from any member of research team or hospital staff under the health program.
3. Results
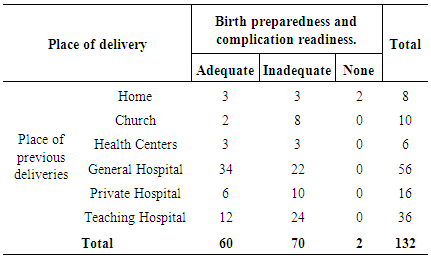
|
|
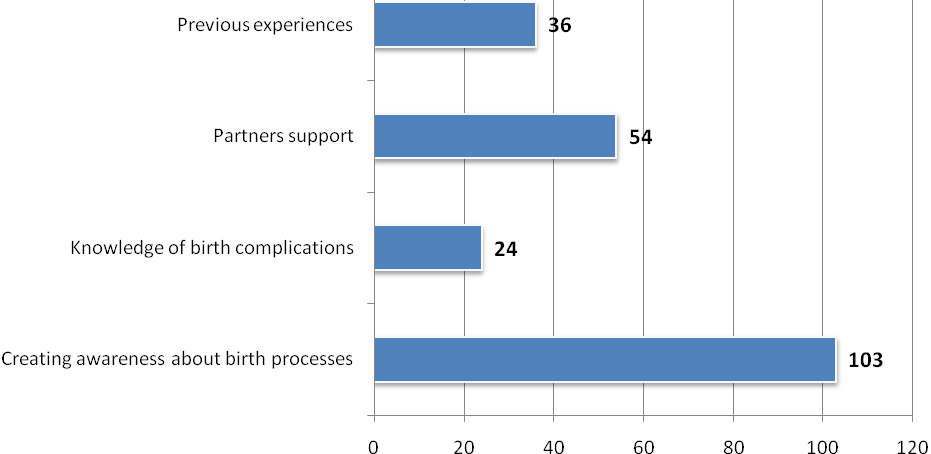 | Figure 1. Barriers to birth plan preparedness |
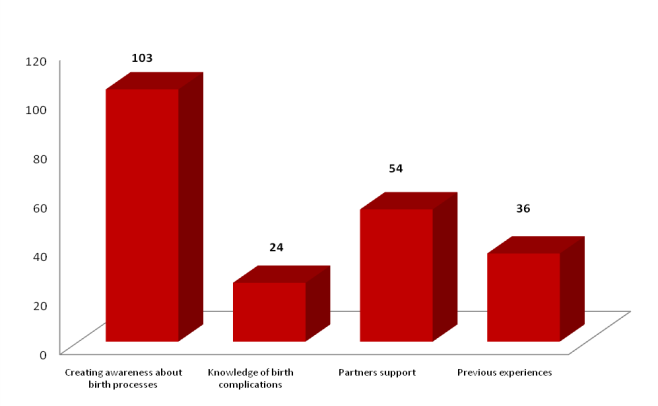 | Figure 2. Facilitators to birth plan preparedness |
|
|
|
4. Discussion
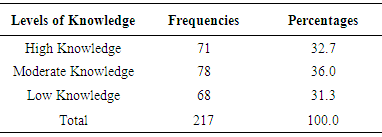
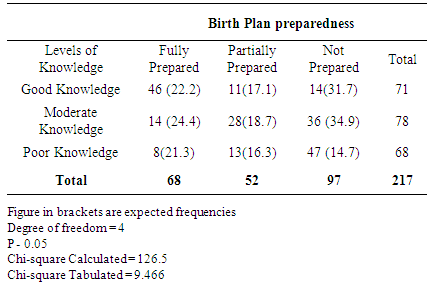
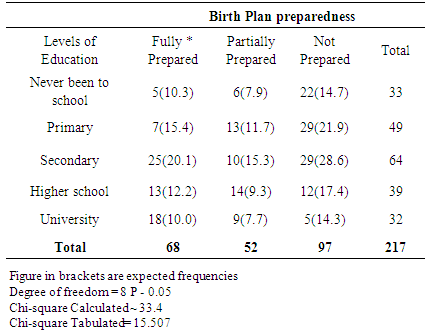
- Despite the implementation of focused antenatal care (FANC) protocols in the state, the level of awareness and practice of Birth Plan and complication readiness is still low. This study revealed that only 32.7% of the respondents exhibited good knowledge on BP/CR and 31.3% were well prepared for child birth and complications. The proportion of women with adequate birth plan in this study is in keeping with 29.9% reported by Morara, 2016 in Kenya. However, this proportion is higher than the figures reported by Ukaegbu et al who observed that most pregnant women had poor knowledge about birth plans. The authors further revealed that only 19.6% of the women could at least identify signs associated with pregnancy and labour. The difference might be due to the good ante-natal health education received during health talks/education and one-on-one counseling promoted by FANC. Also this study was conducted among a group of pregnant women who attended ante-natal clinics in a general hospital. This might however be different if the sample was drawn from the community or general population of pregnant women. This study revealed that most of the respondents made some preparation for birth, but only a few made adequate preparation which entails preparation for emergencies, transportation, support during delivery, potential blood donors, care for family members and choice of health facility. Similar finding was reported by Urassa et al (2012). Also, this study revealed lack of awareness and partners support as major barriers toward effective birth plan preparedness. Nigeria is a male dominated society and male support could really influence a woman’s preparedness toward proper and adequate birth plans. This implies the need to actively involve men in making important decisions regarding maternal care.The inferential statistics showed a significant relationship between BP/CR and level of women education. Level of education also correlated with the identification of danger signs associated with pregnancy and labour. This implies that the more educated women are the more they have information which enhances awareness with regards to reproductive health and they are also more likely to adhere to essential health advice. This finding was similar to that of Kyenga et al (2011) who asserted that education creates high level of awareness, and FACN should be adopted to enhanced individuals plan of birth to reduce neonatal and maternal morbidity and mortality.Furthermore, in this study there was a positive association between women who had experienced previous pregnancy complication or operative delivery and level of BP/CR in index pregnancy. These categories of women usually stay longer in hospital compared to those with uncomplicated vaginal delivery. They are also more likely to be managed by higher cadre of medical staff during admission and in the process they receive more counseling on different pregnancy complications and are better educated on risk factors and preparation for subsequent pregnancies. People who had delivered in a general hospital showed a higher positive tendency to effective BP/CR compared to those who utilized tertiary or private health facility although the difference was not statistically significant. Perhaps the implementation of FANC by the state government owned health facilities has enhance health education and counseling since it emphasizes spending more time on each pregnant woman by the health worker.
5. Conclusions
- This study shows that although FACN has been implemented in the state for the past few years, a vital component of it, Birth Preparedness and complication readiness, is still lacking behind and much work need to be done on the areas of increasing awareness and access to important health information to promote maternal care.
6. Recommendations
- 1. There is need to create more awareness about the need for birth plan and complication readiness to the general public.2. There is need to actively involved male partners in reproductive health of women.3. Government may need to provide subsidized care during pregnancy to those who may not afford, this entails making financial allowances for all pregnant women.4. Education and empowerment programs should be incorporated into the safe-motherhood initiative.
ACKNOWLEDGEMENTS
- We wish to acknowledge the nursing staff of the maternity unit of the General Hospital for the contribution to the success of the research.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML