-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2017; 7(3): 73-77
doi:10.5923/j.phr.20170703.03

To Assess the Tuberculosis Situation in Urban and Rural Areas of Bangladesh with Special Emphasis on the Facility of Treatment Scenarios
Sumaiya Rahman1, Shohel Ahmed2
1Department of Statistics, University of Dhaka, Dhaka, Bangladesh
2Department of Mathematics, Bangladesh University of Engineering and Technology, Dhaka, Bangladesh
Correspondence to: Sumaiya Rahman, Department of Statistics, University of Dhaka, Dhaka, Bangladesh.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

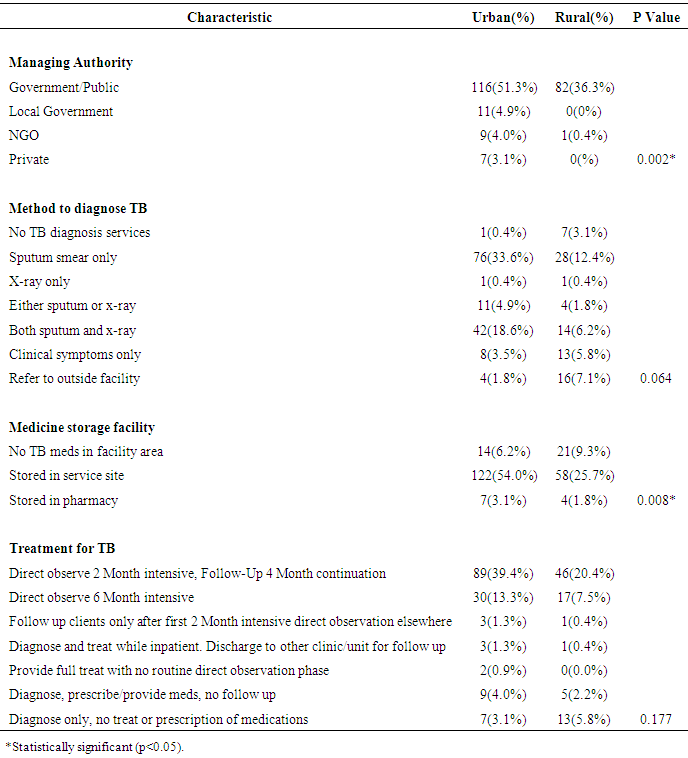
Background: Tuberculosis (TB) is one of the major public health challenges in Bangladesh. Though the country has achieved commendable success in Tuberculosis control, yet this success may deem out unless effective TB treatment control measures are taken based on strong general infection control for the diseases over the country. This study aimed to assess facilitators for health seeking practice among the urban and rural peoples Bangladesh. Methods: Present study used secondary data extracted from nationally representative Bangladesh Demographic and Health Survey (BDHS-2011) between May 2, 2014 & August 14, 2014, on TB patients receiving TB treatments in Urban and Rural areas from Seven Divisions of Bangladesh. Results: Out of 1596 study subjects, 226 TB patients took TB treatment of which Most of the TB patients were from urban (143, 63.3%), others from Rural (83, 36.7%) areas. Availability of treatment for TB from government/public health authorities are known to 116(51.3%) and 82(36.3%) from urban and rural areas respectively. Our study reflects most of the Tuberculosis medicine facility stored in respective urban service site (122, 54%) where else no Tuberculosis medicine facility in rural areas is 21(9.3%). The study has found that, most long term treatment facility has been provided in urban areas compared to rural areas and no association was found between methods to diagnose TB between urban/rural areas. Conclusions: Perceptions of TB and awareness associated with the disease increase the treatment scenarios, therefore promotion of media awareness campaign, engaging the rural people for treatment and effective community service all over the country is needed to increase treatment facility in the future.
Keywords: Tuberculosis, Urban, Rural, Illness perception, Health seeking practice
Cite this paper: Sumaiya Rahman, Shohel Ahmed, To Assess the Tuberculosis Situation in Urban and Rural Areas of Bangladesh with Special Emphasis on the Facility of Treatment Scenarios, Public Health Research, Vol. 7 No. 3, 2017, pp. 73-77. doi: 10.5923/j.phr.20170703.03.
1. Introduction
- Tuberculosis (TB) has been a major public health problem for centuries. It is a leading infectious disease that represents more than a quarter of the world’s preventable deaths. Increase in the incidence of TB in the developing countries and its re-emergence in the developed world led the World Health Organisation (WHO) to declare TB as a global emergency in 1993 [1]. Despite the availability of affordable, effective treatment, the annual total of 8.8 million new cases and an estimated 1.6 million of deaths from TB (WHO Report 2007) represents an intolerable burden of human suffering [2]. In Bangladesh, TB is a major public health problem and one of the leading causes of adult mortality and preventable deaths. Tuberculosis (TB) kills an estimated 75,000 people per year in Bangladesh [3]. According to the WHO, among 22 countries where TB is considered “high burden,” Bangladesh is ranked 6th with a mortality rate of 45/100,000 and an incidence rate of 225/100,000 annually, with a prevalence of 411 cases per 100,000 population and 10th among 27 high priority multidrug resistant (MDR) and extensively drug resistant (XDR) TB countries [4]. In Bangladesh, The National TB Control Programme (NTP) coordinates the diagnosis, reporting and treatment of TB cases according to WHO guidelines. In 1993, the Government of Bangladesh started NTP adopting the Directly Observed Treatment Short Course (DOTS) strategy in 4 pilot sub-districts. It was progressively expanded to 460 sub-districts by June 1998. At present the coverage is said to be 99% including metropolitan cities as Dhaka, Chittagong, Rajshahi, Khulna, Barisal and Sylhet [3]. TB can be completely cured through the Directly Observed Treatment Short Course (DOTS). DOTS is currently practiced as the most effective way of controlling the disease. Even though TB is completely curable, a large number of people still continue to become ill and die from the disease. Many cases remain undiagnosed due to the lack of proper treatment facility. Most TB cases are diagnosed through passive case finding. Three sputum specimens are obtained from TB suspects for sputum-smear microscopy. A new smear-positive TB case is diagnosed on the basis of one or more sputum specimens testing positive for acid fast bacilli. Conventional microscopy cannot detect TB bacilli when the concentration is less than 5000 bacilli per ml of sputum. In Bangladesh, 65% of the pulmonary TB can be detected by conventional microscopy and the rest (35%) remain undiagnosed [5]. These group of TB patients are called smear negative pulmonary TB. Smear-negative TB has to be diagnosed on the basis of symptoms, clinical features, and supportive chest X-ray findings.A nationally representative survey conducted in 2009 revealed that the prevalence of TB is 10 times higher among the lowest wealth quintile, compared to the highest; and greater in rural areas compared to urban areas. The NTP is credited with implementing directly observed therapy short course (DOTS) countrywide with an impressive 92% treatment success rate. Though the country has met WHO’s case detection rate of 74%, only 14% of cases are located in urban areas. This calls into question potential barriers and facilitators to both detection and treatment in urban and rural areas among vulnerable populations. The study’s results will be helpful for improving the design of TB control activities in urban and rural areas. This study will also provide evidence in the form of feedback to improve the operation of the NTP and toward improving the function of TB control activities in Bangladesh.
2. Methods
- This study used secondary data extracted from nationally representative Bangladesh Demographic and Health Survey (BDHS-2011) conducted by the authority of the National Institute for Population, Research and Training (NIPORT) of the Ministry of Health and Welfare, Bangladesh and funded by USAID. This study has been carried out between May 2, 2014 & August 14, 2014, on TB patients receiving TB treatments in urban and rural areas from Seven (Barisal, Chittagong, Dhaka, Khulna, Rajshahi, Rangpur, Sylhet) divisions of Bangladesh. There were total of 226 study subjects who had under TB treatment in the said duration. Parameters regarding socio-demographic profile include division, urban/rural, type of facility, managing authority. Study variables include storage of medicine, quality of care system, facility offer for TB tests, treatment for TB etc. Case definitions, treatment outcome definitions and other protocols have been followed as per global tuberculosis report 2016 published by World Health Organization. The data were analysed using IBM SPSS (version 20). Descriptive analysis was done (means, proportions, and percentages) for demographic details. Categorical variables were compared using Chi square test with P value of <0.05 was considered significant.
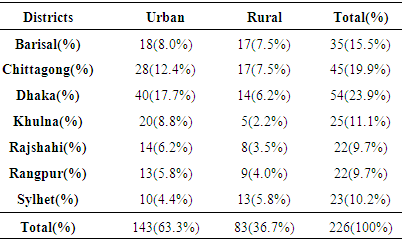
 | Figure 1. Study subjects from different districts of Bangladesh receiving TB treatment |
3. Results
- A total of 1596 study subjects were included in the final analysis. A total of 226 TB patients took TB treatment from seven districts of Bangladesh between May, 2014 and August, 2014. Most of the TB patients were from urban (143, 63.3%), others from rural (83, 36.7%) areas. Majority of the stakeholders (54 subjects, 23.9%) were from Dhaka (Capital of Bangladesh), 2nd highest from Chittagong (45 subjects, 19.9%), followed by (35, 15.5%) from Barisal, (25, 11.1%) from Khulna, (23, 10.2%) from Sylhet, (22, 9.7%) from Rajshahi and Rangpur (Table 1). Since the data came from BDHS, carried out in 2014, seven divisions were specified in region variable; Mymensingh was not considered separate division in this study since it was declared as new division on 12 January 2015.
|
|
4. Discussion
- In the present study it was found that 226 TB patients took TB treatment from seven districts of Bangladesh of which most of the TB patients were from urban (143, 63.3%), others from Rural (83, 36.7%) areas. A study conducted by Sayera Banu et al. on Tuberculosis in an urban Slum of Dhaka City revealed high prevalence of TB in an urban slum area which is more than two times higher than overall prevalence and nearly four times higher than the prevalence in urban settings [6]. Another study by Hossain, S showed in 2007, 18.5% of all TB cases were reported from urban areas that make up 28 % of the country’s population. This poor case finding in urban areas might happened due to delayed and lower coverage of DOTS in the urban areas and presence of excessive numbers of practitioners not connected to the NTP [7]. A study on Control of tuberculosis by community health workers in Bangladesh by Mushtaque R Chowdhury et al. showed that tuberculosis is more common in urban than rural areas [8]. Our study showed that the availability of treatment for TB from government/public health authorities is known to (198, 87.9%), where else private sector provides (7, 3.1%). A study on government–NGO collaboration in the case of tuberculosis control in Bangladesh by Zafar Ullah et al. showed that most TB patients prefer to seek care from the private sectors. This study also revealed the lowest-level health facilities providing appropriate TB care are Upazila Health Complexes located in the upazila headquarters (one hospital per 250 000 population). To improve reproductive health services GOB implement DOTS in Upazilas and four metropolitan cities with the collaboration of different NGOs [9].In the present study most of the Tuberculosis long term treatment facility and medicine stored has been provided in urban areas. Study conducted by Ziaul Islam et al. on case detection of tuberculosis among children in Bangladesh showed supply and maintenance of necessary diagnostics and child friendly TB drugs remained suboptimal in the country [10]. In 2014 Child TB case detection was 97% in urban and 13% in rural areas. A study on 432 key community members, 229 (53%) of all had good knowledge regarding TB and only 13 (3%) of them had poor knowledge [11]. A results from a countrywide care seeking tuberculosis survey in Bangladesh provided that a total of 273 TB cases, 240 (88%) from the TB registers. Among the 240 cases detected passively under NTP, 118 (49.1%) sought initial care from informal providers, 106 (44.2%) from formal providers and 16 (6.7%) used self-care [11]. This study revealed several key findings that will help to strengthen future TB control efforts in urban and rural areas in Bangladesh. We observed that the facility of treatment was altogether different in urban and rural areas of Bangladesh with respect to prescribing treatment and availability of drugs. However, unlike in the urban areas, there was almost a complete absence of diagnostic procedures and referrals in the rural areas. It can be said that most of the treatment facility for TB cases was sought from public sectors and limited to urban areas. A large proportion of patients remained in the rural areas during subsequent infection. It is imperative that the NTP should immediately take the initiative to engage all types of care providers, particularly the private sectors and NGOs. It is also necessary to strengthen the on-going advocacy communication and social mobilization activities to increase awareness of key TB symptoms, availability of diagnosis and medicine in an attempt to prevent Tuberculosis in Bangladesh.
5. Conclusions
- Tuberculosis long term treatment facility services are still underutilized and informal caregivers remained the major care providers for such cases in Bangladesh. In order to improve treatment strategy, it is necessary that the National Tuberculosis Programme immediately takes effective initiatives to engage all types of care providers including public and private sectors, particularly community service providers who are the first point of care for the majority of the TB suspects. Current TB treatments have proven to be more successful to facilitate urban people, while underprivileged populations lived in rural areas have fallen through the gaps in the system. So the NTP should implement strategies to raise community awareness alongside increasing the capacity of service providers and ensuring availability of diagnostics and pediatric TB drugs at the rural level.
ACKNOWLEDGEMENTS
- The authors wish to thank The Demographic and Health Surveys (http://dhsprogram.com/) [12] and Bangladesh Demographic and Health Survey for providing primary data used in this study. The authors would specifically like to thank NIPORT and USAID for their assistance in conducting Bangladesh Demographic and Health Survey (BDHS-2014).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML