-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2016; 6(5): 132-142
doi:10.5923/j.phr.20160605.02

The Threats of Globalization on Global Public Health with Specific Reference to Tobacco Control
Laud A. Dei Jnr 1, Marian Fabyan 2
1Monitoring and Evaluation, World Education Inc, Ghana
2Mental Health, North Pointe Psychiatry, Denton, Texas, USA
Correspondence to: Laud A. Dei Jnr , Monitoring and Evaluation, World Education Inc, Ghana.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The context of Globalization in health is viewed as a concerted global effort towards the prevention, elimination and eradication of disease, and the promotion of human health worldwide. As a result, the domestic and international spheres of public health policy are becoming more intertwined and inseparable. The spread of global tobacco products may indicate one of the instances of globalization of the spread of non-communicable diseases. The tobacco epidemic kills around six million people a year, and more than five million of those deaths are the result of direct tobacco consumption, while more than 600 000 are the result of non-smokers being exposed to second-hand smoke. This is one of the major public health challenges ever faced in the world. Tobacco and Cigarette smoking have negative effect on nearly every organ of the body, causes many diseases, and reduces the health of smokers in general. Smoking and passive smoking cause more than 20 major categories of fatal and disabling disease, including lung and other cancers. It is projected that tobacco use will cause 8.4 million deaths by 2020, 70% of which will occur in developing countries. Of the 100 million projected tobacco-related deaths over the next 20 years, about half will be of people in the productive ages of 35-69. In general, 9% of women in developing countries and about 22% in developed countries currently smoke. Without robust and sustained initiatives, these figures are expected to rise dramatically, with today's 250 million women smokers rising to 340 million by 2020. This article discusses the key problems and opportunities of globalization and how it could be used to control tobacco production within the global public health.
Keywords: Globalization, Public Health, Tobacco Control
Cite this paper: Laud A. Dei Jnr , Marian Fabyan , The Threats of Globalization on Global Public Health with Specific Reference to Tobacco Control, Public Health Research, Vol. 6 No. 5, 2016, pp. 132-142. doi: 10.5923/j.phr.20160605.02.
Article Outline
1. Introduction
- Globalization is defined here as a process of closer interaction of human activity within economic, political, cultural and other social spheres, and along spatial, temporal and cognitive dimensions (Lee 2001). According to Kumar’s article written in 2003 titled “A Critical Methodology of Globalization: Politics of the 21st Century?” he made it clear that definitions of globalization are presented against the reality of the global situation. With this in mind, globalization has been defined in this paper: “as the process where countries depend on each other for trade in terms of the sale of consumer goods and services which is free from the control of public health expects, for individual, economic and political gains.” The context of Globalization in health is viewed as a concerted global effort towards the prevention, elimination and eradication of disease, and the promotion of human health worldwide (Bennett & Tomossy 2006). As a result, the domestic and international spheres of public health policy are becoming more intertwined and inseparable. The spread of global tobacco products may indicate one of the instances of globalization of the spread of non-communicable diseases. The tobacco epidemic kills around six million people a year, and more than five million of those deaths are the result of direct tobacco consumption, while more than 600 000 are the result of non-smokers being exposed to second-hand smoke. This is one of the major public health challenges ever faced in the world. Tobacco and Cigarette smoking have negative effect on nearly every organ of the body, causes many diseases, and reduces the health of smokers in general. Smoking and passive smoking cause more than 20 major categories of fatal and disabling disease, including lung and other cancers. It is projected that tobacco use will cause 8.4 million deaths by 2020, 70% of which will occur in developing countries.1 Of the 100 million projected tobacco-related deaths over the next 20 years, about half will be of people in the productive ages of 35-69.In 2013, 21% of adults globally were current smokers, 950 million men and 177 million women. Despite increasing global population between 2007 and 2013, smoking prevalence has actually declined worldwide, preventing an increase in the number of smokers in the world (WHO 2015). Even though there is some evidence of a decline in smoking prevalence globally, how significant is this decline? In 2013, according to the WHO Tobacco prevalence estimates, there is a total of 1.1 billion smokers globally, this represents one third of the worlds adult population. Smoking prevalence is highest in high-income countries, with a quarter of adults (25%) in 2013 being current smokers. In contrast, 21% of adults living in middle-income countries and 16% of adults in low-income countries were current smokers (see figure 1 below). Tobacco still causes some 3.5 million deaths annually worldwide (National Plan of Action on Smoking for 2008 – 2012, 2008 p. 14).
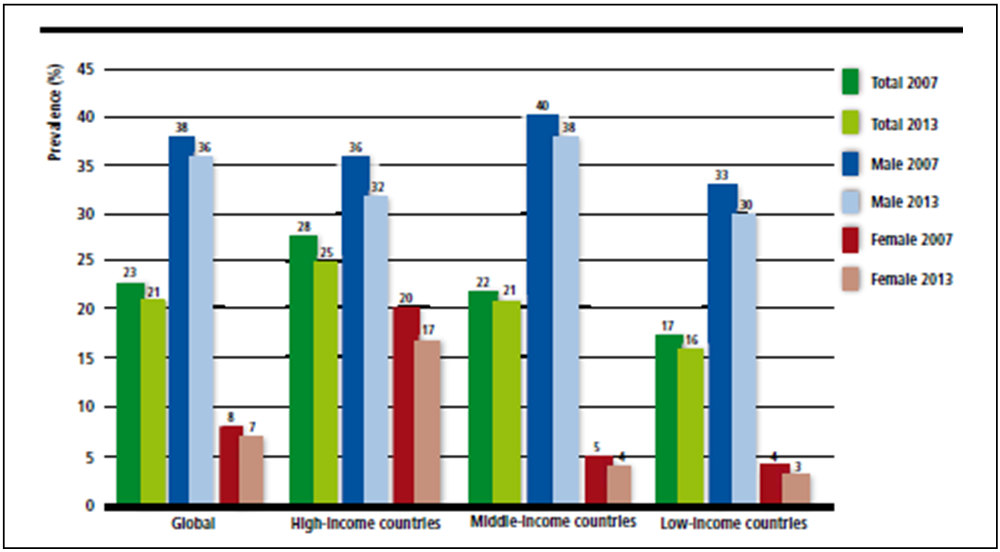 | Figure 1. Adult Tobacco Smoking Prevalence, 2007 - 2013 (Source: WHO Prevalence Estimate2) |
2. Health and Tobacco Use
- Critics argue that globalization creates challenges for the governance of global health, including the need to construct international regimes capable of responding to global threats to public health. These problems are not new, the globalization of public health led to the development of international health diplomacy and international regimes for public health beginning in the mid-19th century. There has always been a sharing of goods, services, knowledge and cultures between people and countries, but in recent years improved technologies and a reduction of barriers means the speed of exchange is much faster. This means that bigger markets could make bigger profits which leads to greater wealth for investing in development and reducing poverty in many countries. China, India, Uganda, and Vietnam, for example, have all experienced surges in economic growth since liberalizing their trade and inward investment policies.Figure 2 below shows the top ten leading producers of tobacco, of which, four countries namely, China, Brazil, India, United States and Indonesia produce two-thirds, representing 97% of the world’s tobacco. China alone produces 36.4% of the world’s total tobacco, followed by Brazil, the second largest producer with less than half of China and then India producing approximately 1% below Brazil.
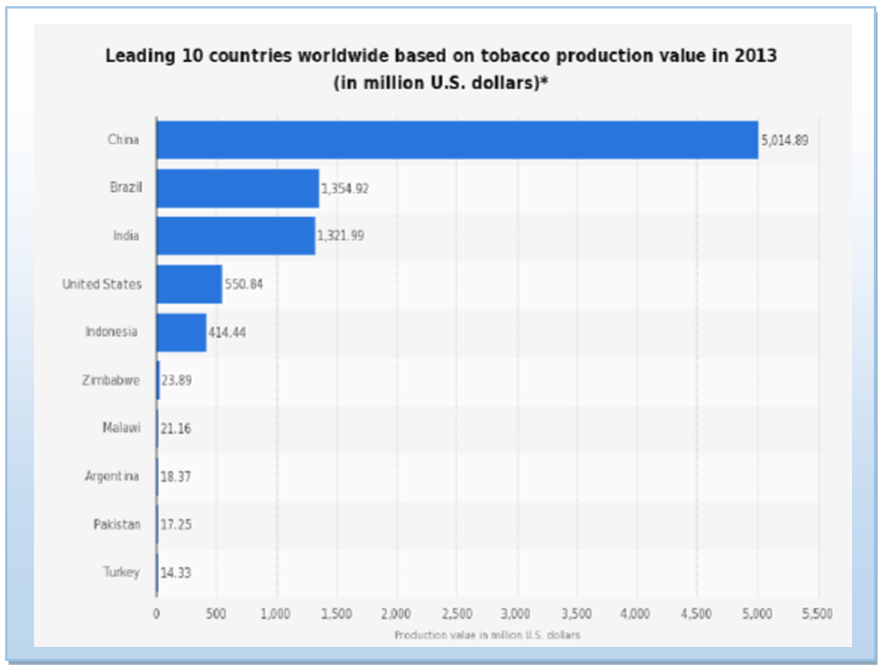 | Figure 2. Source: Statista  |
3. Globalization and Tobacco Control
- The tobacco industry not only seeks to promote use of its products and expand into new markets, but also seeks to weaken strong tobacco control policies and undermine public health advocacy efforts (Yang & Malone 2008), especially in countries where tobacco is the main foreign exchange earner. The WHO Framework Convention on Tobacco Control, which was adopted in May 2003 by WHO’s 192 member States, is intended as a common framework in which countries can work together to address the challenge that tobacco use represents at the global level. The efforts to strengthen tobacco control worldwide is a clear example of the impact of globalization on public health. Beginning in the 1950s, the tobacco industry has undergone significant restructuring over the past half century to become a highly globalized industry. This change poses a number of important challenges, both positive and negative for health.Tobacco is one of the rare lethal products legally and widely traded at the global level. Its products have a transnational dimension when it comes to smuggling, global advertising and promotion, or international cooperation on information sharing. The tobacco epidemic has thus become globalized, and its globalization restricts the capacity of countries to regulate tobacco through domestic legislation alone.With globalization, even some non-communicable diseases traditionally considered to be private goods are developing stronger public characteristics. Scientific evidence has firmly established that tobacco consumption, after decades of latency, can increase the risk of lung and bladder cancer and heart and lung disease. The world’s 1.1 billion smokers, 800 million of whom are in developing countries, account for about 3 million tobacco-related deaths a year (Nakajima 1997, p. 327).Consumption of tobacco is usually considered voluntary, yet we now recognize that individual choice is not entirely free from structural workplace constraints, peer pressures or the biology of addiction. Indeed, many behavioral health risks and consequences are not strictly private. While addiction to tobacco may be voluntary, studies have confirmed the powerful behavioral influence of commercial advertising are often targeted at teenagers and women. Moreover, neither the health effects of tobacco use or the costs of treatment are entirely private, because passive smoke is hazardous to non-smokers, and most tobacco-related costs are passed on to the public through medical insurance or social security. Thus global tobacco control has strong public goods characteristics.In the case of tobacco, cognitive globalization shapes mental frameworks on tobacco use around modernity, prosperity, and “western” values. Cognitive Globalization is profoundly influencing how we see ourselves and the world around us. The main agents of change here are the mass media, the advertising industry, consultancy firms, research institutions, political parties, religious groups and other institutions seeking to win “hearts and minds”. In the process, our cultures, wants or perceived needs, values, beliefs, knowledge and aspirations are being changed (Lee, 2003). Current and prospective tobacco users, regardless of which country they live in, are subjected to nearly ubiquitous messages promoting tobacco use. These messages are both direct (e.g. billboards and magazine advertisements) and indirect (e.g. tobacco use depicted in movies or tobacco industry-promoted concerts). Campaigns to counter these messages, whether through education, fear, entertainment, or ridicule, have been shown to be an important element in broader campaigns to prevent or reduce tobacco use (Farrelly, 2005). These counter marketing campaigns have been aimed at both youth and adults. They are effective in raising consciousness about the tobacco issue; demoralizing it; exposing tobacco industry tactics; and involving youth and adults in local, regional, and national campaigns to change tobacco policies, such as clean indoor air regulations and channeling tobacco taxes to tobacco control and other health care needs. Although media-based advertising can be expensive, and the tobacco industry will always far outspend tobacco control advocates, novel, entertaining, cutting-edge tobacco counter marketing campaigns, often supported by local governments and with the help of pro bono support from creative marketing firms, have been shown to attract attention and support far beyond the amount of funds spent on the campaign and, importantly, to have a direct effect on reducing tobacco use (Farrelly 2005). Cognitive globalization is supported by illegal smuggling of global brands and by systematic policy interventions, including concentrated efforts to forestall any international agreements, international governance efforts and regulation at national or international levels. Ethically, cognitive globalization of tobacco products threatens the autonomy of nations and their ability to protect the health of their citizens. It also violates the principle of non-maleficence insofar as there is no safe level of tobacco use and thus any promotion of trade in tobacco is in effect malevolent.However, globalization offers opportunities for strengthening tobacco control worldwide through improved coordination, information sharing and policy learning. The signing of the Framework Convention on Tobacco Control (FCTC) in 2003, and its implementation, represented a unique opportunity to strengthen global governance for health. A review of public health efforts to reduce tobacco use in the United States which mirrored similar approaches in, for example, Australia and the United Kingdom captured, in capsule form, both the successes and the errors made in these efforts, which, ultimately, have cut tobacco use by 50% or more in the majority of the high income countries since population prevalence peaked during the early 1960s (Fiore et al, 2009). The industry has become dominated by a small number of large and powerful companies increasingly operating across national borders. The capacity for the public health community to effectively regulate and hold to account the activities of the industry has become more difficult as a result. There has been a clear shift in focus by Transnational Tobacco Companies (TTCs), from traditional markets to so-called emerging markets in Eastern Europe, Asia, Africa and Latin America. This is predicted to lead to a major shift in the global burden from tobacco-related diseases to the developing world. There is clear data indicating that the tobacco epidemic has now expanded to, and become more focused on, the world’s low- and middle-income countries (LMIC), largely due to the expansion of the multinational tobacco industry’s marketing efforts in Eastern Europe, Asia, Africa, and Latin America (Shafey O et al., 2009; WHO, 2008). There is a need to strengthen understanding of the key contribution of the tobacco industry in promoting the rising prevalence of smoking in low and middle-income countries, its targeting of particular populations, and its undermining of tobacco control research and policy. Fortunately, although the sharply increasing tobacco use prevalence rates in these regions is very alarming, the deadly experience of the high income nations need not be wholly repeated in the LMICs. Resources that were not available in the mid-1960s now abound: The World Health Organization’s brilliant Framework Convention on Tobacco Control (FCTC) and its MPOWER report and funding from other sources, such as the Michael R. Bloomberg Foundation, the Bill and Melinda Gates Foundation, and the Pfizer Foundation, and more modest, such as Canada’s International Development Research Corporation, the Norwegian Cancer Society, the American Cancer Society, and Cancer Research UK. In addition, there is a significant body of tobacco-focused public health research and intervention experience, as well as experience in addressing both communicable and non-communicable diseases (NCDs), on which the LMICs may now draw as they address the tobacco epidemics in their regions.Due to the ubiquity and lucrative nature of tobacco growth and sales, tobacco products are often included in negotiations surrounding global, regional, or country-to-country trade agreements. For many years, tobacco products were treated no differently than fruits, textiles, or metals. The appalling health effects of tobacco products were not considered as negotiators made arguments about the size of tariffs, the types of tobacco products, and the amount of unprocessed leaf, that would be included in a given agreement. In recent years, however, due to the resistance some countries, such as Thailand, have offered in demanding that tobacco imports not always be a natural part of any trade agreement, there has been a growing recognition that excluding tobacco from free-trade agreements would protect health. Successful arguments have been made that excluding tobacco from trade agreements is compatible with international law, which provides for other harmful products such as landmines to be exempted (Taylor et al, 2000; Bianco, 2004).Duty-free and reduced-cost sales of tobacco (e.g. for military personnel, in hospitals, etc) have a dual, negative effect on tobacco control efforts. First, as noted above, the reduced cost of tobacco products results in increased consumption. Second, the visibility of low-cost, duty-free tobacco products (as well as low-cost tobacco products in other venues) counteracts efforts to “denormalise” tobacco use; hundreds of millions of global travelers and consumers of low-cost tobacco products are regularly exposed to the implied message that tobacco is not only a broadly accepted product, but also that its ubiquity and low cost must make it acceptable, both socially and with regard to its effects on health (Wilson et al, 2009). Trade liberalization has also significantly increased tobacco use, particularly in low and middle income countries (Chaloupka 2000). Under the support of free trade, increased competition leads to reduced prices and increased marketing efforts for all traded goods. However, nations may apply a variety of trade protections, including tariffs, quotas, and price supports for locally grown agricultural products. In addition, marketing restrictions, licensing, restricted product lists, foreign exchange controls, content requirements, and production subsidies are also used to protect national agricultural products and markets. However, these national trade policies do not pretend to focus on health as the basis for intervention; they are primarily intended to protect state monopolies in certain products and to support national agricultural product markets. Public health concerns should be grounds for restrictions on free trade, even if raising these concerns may impede market liberalization for some imported goods, that is, those that are clearly harmful to health (Taylor, 2000). Inhalation of second-hand smoke, in addition to causing cancers among non-smokers, also causes coronary artery disease and numerous illnesses among infants and children. Nevertheless, in many parts of the world, daily exposure to second-hand smoke is an ordinary and pervasive occurrence (Shafey et al, 2009). Local ordinances and regulations to reduce exposure have been increasing for some time, and spreading from the industrialized countries to the LMICs. Beginning with Ireland’s nationwide effort to reduce second-hand smoke exposure in 2004, an increasing number of nationwide bans have begun taking effect. It is vital, not only for the health of non-smokers but also for smokers who may be encouraged to quit or reduce their smoking due to the reduction of opportunities to smoke, for the prevalence of smoke-free areas to continue to spread and, eventually, become the norm.Several years after the WHO Framework Convention on Tobacco Control, and the introduction of MPOWER to support parties to meet their WHO FCTC obligations, there has been some evidence of steady progress in global tobacco control. According to the World Health Organisation (WHO 2015) Report on Tobacco Epidemic, progress in global tobacco Control was significant between 2012 and 2014, compared to the previous WHO Report on the global tobacco epidemic, 2013, which reported data from 2012. The global population covered at least one MPOWER measure increasing from 2.3 billion to 2.8 billion in 2014, an increase of half a billion people (7% of the world’s population). The number of countries implementing at least one MPOWER measure at the highest level has increased by 11 since 2012, from 92 to 103. Each MPOWER measure saw new countries implementing best tobacco control practice since 2012.
3.1. Increasing Tobacco Prices as a Control Intervention
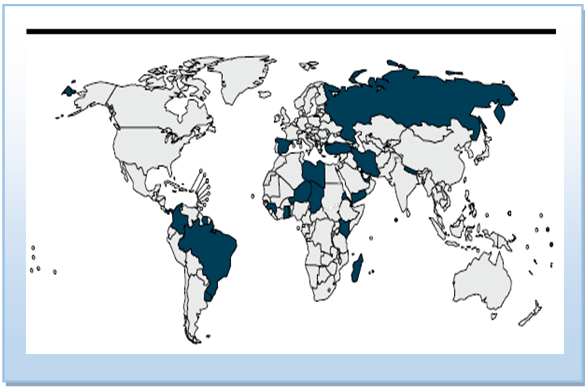
- In the 1994 Uruguay round of General Agreement on Tariffs and Trade (GATT) negotiations, tobacco product tariff rates among developed nations were reduced by more than half, from an average of 22.1% to 10.2% (Guha-Khasnobis, 1998). Due to this reduction in tariffs, there was an increase of 42% between 1993 and 1996 in global exports of tobacco products; globally, tobacco consumption was found to be on average 10% higher than it would have been in the absence of these actions (Chaloupka 1998). Globalization of tobacco use and the ensuing disease burden challenges national governments’ sovereignty to protect the health of their populations (Kickbusch 2002). Increases in tobacco taxes is perhaps the most effective intervention to reduce tobacco use (van Baal et al 2006).According to the International Agency for Research on Cancer (IARC 2011), hundreds of studies from countries around the world have examined the impact of tobacco taxes and prices on tobacco use. Before 2000, nearly all of this research was conducted in high-income countries (Chaloupka et al 2000), however, research from dozens of low- and middle-income countries confirms that higher tobacco taxes and prices lead to significant reductions in tobacco use (IARC 2011). Studies from a number of countries typically show that half of the decline in tobacco use associated with higher taxes and prices results from reduced prevalence (i.e. from users quitting) (IARC 2011). The remaining half comes from reduced intensity of use (i.e. users consuming less by switching from daily to occasional smoking, or reducing the number of cigarettes smoked each day).In the United States of America (USA), cigarette prices rose nearly 350% between 1990 and 2014, in large part because of a five-fold increase in average state cigarette taxes and a six-fold increase in the national cigarette tax (Orzechowski & Walker 2014). During this time the number of cigarettes smoked per capita dropped by more than half, and the percentage of adults who smoke fell nearly one third.6 Tax and price increases in Brazil explain nearly half of the 46% reduction in adult smoking prevalence between 1989 and 2010 (Levy, de Almeida and Szklo 2012). In total, only 33 countries with a combined population of 690 million have effectively imposed high taxes on tobacco as a control measure.
 | Figure 3. Raise Taxes on Tobacco – Highest Achieving Countries, Territories and Areas, 2014 (Source: WHO Report on the Global Tobacco Epidemic, 2015) |
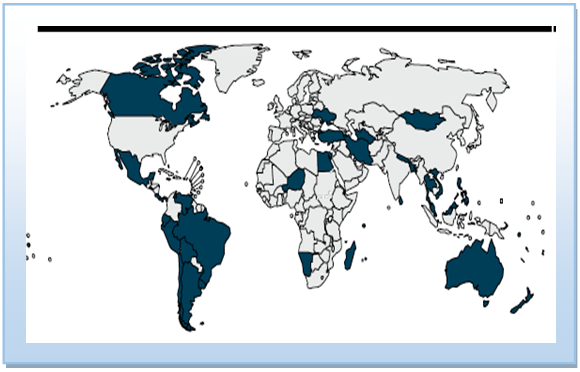
3.2. Ban on Tobacco Advertising and Promotion
- Tobacco companies spend tens of billions of US dollars worldwide each year on Tobacco Advertising, Promotion and Sponsorship (TAPS) activities.7 The primary purpose of TAPS is to increase tobacco sales,8 and they are effective in encouraging non-smokers to start (particularly youth and women in low- and middle-income countries) (Lee, Ling and Glantz 2012), and current smokers to continue. TAPS also blunt tobacco control efforts by “normalizing” tobacco use and influencing media and other businesses that benefit from TAPS expenditures. To counteract this, complete bans on all TAPS activities are needed as a key tobacco control strategy. Partial bans and voluntary restrictions are ineffective, having little or no effect (Saffer and Chaloupka 2000). Employing Comprehensive TAPS bans will delay the industry’s ability to promote and sell its products, and reduce tobacco consumption in all countries regardless of income level (Saffer and Chaloupka 2000). In particular, TAPS bans reduce youth smoking initiation and prevalence rates, which may lead to lower levels of adult smoking in future years (Centers for Disease Control and Prevention 2007). To be effective, bans must completely cover all types of TAPS activities, both direct advertising in all types of media, and indirect advertising, promotion and sponsorship (Saffer 2000), including point-of-sale advertising in retail stores. Due to the effectiveness of TAPS bans in reducing tobacco use and initiation, the tobacco industry strongly opposes them and is increasingly aggressive in circumventing their proscription. Employing Comprehensive TAPS bans will delay the industry’s ability to promote and sell its products, and reduce tobacco consumption in all countries regardless of income level (Saffer and Chaloupka 2000). In particular, TAPS bans reduce youth smoking initiation and prevalence rates, which may lead to lower levels of adult smoking in future years (Center for Disease Control and Prevention 2007). As at 2014, only 29 countries with a total population of 832 million representing only 12 per cent of the world’s population have passed a complete TAPS ban globally. This is an increase 3 per cent compared to the global coverage of ban on TAPS in 2012.Figure 4 below indicates countries with the highest level of achievement of enforcing advertising, promotion and sponsorship of tobacco. They include: Albania, Bahrain, Brazil, Chad, Colombia, Djibouti, Eritrea, Ghana, Guinea, Iran (Islamic Republic of), Kenya, Kiribati, Libya, Madagascar, Maldives, Mauritius, Nepal, Niger, Panama, Russian Federation, Spain, Suriname, Togo, Turkey, Tuvalu, United Arab Emirates, Uruguay, Vanuatu, and Yemen.
 | Figure 4. Enforce Bans on Tobacco Advertising, Promotion and Sponsorship – Highest Achieving Countries, 2014 (Source: WHO Report on the Global Tobacco Epidemic, 2015) |
3.3. Increase Health Warnings on Tobacco Use
- Globally, the right to health information is key in any given population, including accurate information about the health effects of tobacco use (Kozlowski and Edwards 2005). Even though there is clear evidence of the health risks tobacco usage poses, many smokers do not fully understand the risk of tobacco use to their health or the health of others (Hammond et al 2006). Accurate warnings about the harms of tobacco use and second-hand smoke exposure will influence people to decide against using tobacco (Fathelrahman et al 2009). Health warnings also change social norms about tobacco use, which reduces tobacco use and increases support for tobacco control measures (Hammond et al 2006).An effective health warning label to provide a direct health message to smokers, raising awareness of their health risks and increasing the likelihood that they will reduce or quit tobacco use. Warnings that are boldly written to cover at least half of both primary tobacco package surfaces are more effective than smaller prints or those that contain only text (Borland et al 2009). Warning labels can be implemented at virtually no cost to governments (Hammond et al 2007), and generally are more strongly supported by the public than most other tobacco control interventions (Kamyab, Nonnemaker and Farrelly 2015). They should be specific in describing the health effects of tobacco use, and be periodically rotated to maintain their impact (WHO 2013). These warnings should not contain any deceptive terms, such as “light” or “mild” they suggest some products are less harmful which is never the case (WHO 2013). Plain packaging enhances the impact of health warnings and other packaging and labelling measures, and reduces the marketing impact of package design (Yong et al 2015). Use of graphic pack warnings has increased; more people are protected by this MPOWER measure than by any other. Around 1.4 billion people (almost 20% of the world’s population) were protected by strong pack warnings in 2014, up from 14% in 2012 (WHO 2014). According to the WHO report on the 2015 Global Tobacco Epidemic, although 86% of countries have pack warning legislation, only a third have successfully mandated graphic warnings, and less than a third have mandated that warnings be sufficiently large to cover at least 50% of the main package surfaces. Figure 5 shows countries with the highest level of achievements which include: Argentina, Australia, Bangladesh, Plurinational State of Bolivia, Brazil, Brunei Darussalam, Canada, Chile, Costa Rica, Djibouti, Ecuador, Egypt, El Salvador, Fiji, Islamic Republic of Iran, Jamaica, Madagascar, Malaysia, Mauritius, Mexico, Mongolia, Namibia, Nepal, New Zealand, Niger, Panama, Peru, Philippines, Samoa, Seychelles, Singapore, Solomon Islands, Sri Lanka, Thailand, Trinidad and Tobago, Turkey, Turkmenistan, Ukraine, Uruguay, Vanuatu, Venezuela (Bolivarian Republic of), and Viet Nam.
 | Figure 5. Health Warning Labels About the Dangers of Tobacco – Highest Achieving Countries, 2014 (Source: WHO Report on the Global Tobacco Epidemic, 2015) |
3.4. Programs to Help Smokers Quit
- Most smokers want to quit, especially if they are aware of the full range of harms caused by tobacco use, but many find it difficult to do so unaided because of the extreme addictiveness of nicotine (Centres for Disease Control and Prevention 2011). Although most smokers who quit are able to do so without assistance, cessation interventions greatly increase quit rates, at least three types of clinical treatment, such as, Cessation advice in primary health care systems, Free telephone help lines (quit lines) and Pharmacological therapy, should be included smoking cessation programs (Fiore et al 2008). People who quit tobacco experience immediate and significant health benefits, and reduce most of their excess health risk within a few years (Doll et al 2004). Clinical cessation interventions are effective, and are also extremely cost-effective when compared to other health care system interventions (Cromwell et al 1997). To ensure successful smoking cessation programs worldwide, the Government’s support is essential to ensure health care systems assume primary responsibility for such programs. Cessation services are most effective when incorporated into a comprehensive national tobacco control program (Centres for Disease Control and Prevention 2014). For example, even in Brazil the second largest producer of tobacco, have since the 1990s effective tobacco control measures which have significantly reduced its adult smoking rates by nearly 50%, from 34.8% in 1989 to 18.50% in 2008 (see figure 6 below) (Monteiro et al 2007 cited in Szklo et al 2012 pp 162–167). Due to this significant decrease in tobacco use, 420,000 premature deaths were prevented between 1990 and 2010 (Levy, de Almeida and Szklo 2012).
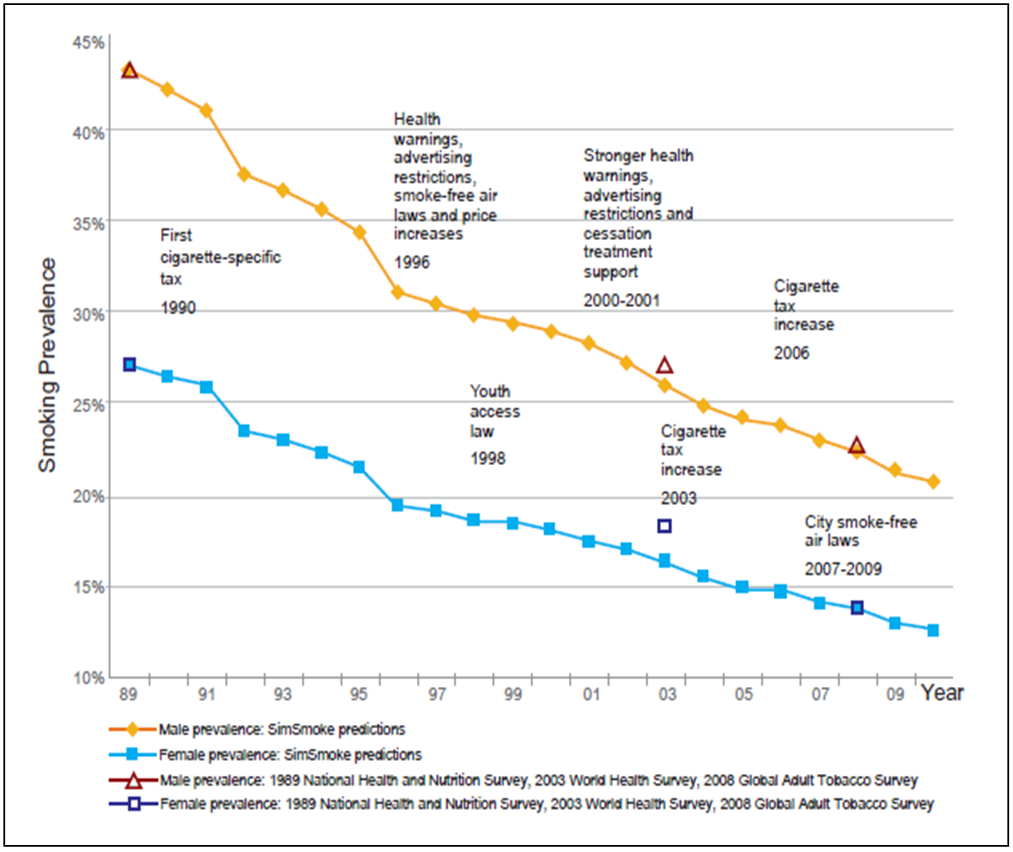 | Figure 6. Brazil Smoking Prevalence for Individuals Aged 18 and Above, 1989–2010 (Source: Levy (2012) SimSmoke Predictions and Various Surveys) |
4. Conclusions
- The number of people who die prematurely because of tobacco use is a major global public health concern. Even though there is some evidence of reduction due to high taxes and ban on promotions and advertising on tobacco, the number of people who still smoke and die prematurely due to tobacco use are high. Countries at all levels of development are victims of the tobacco epidemic. The WHO FCTC strongly suggests that every Party should establish and adequately finance a national tobacco control coordination mechanism to build needed capacity for implementing effective and sustainable policies to reverse the tobacco epidemic. The ministry of health or equivalent government agency should take the lead on strategic tobacco control planning and policy setting, with other ministries or agencies reporting to this centralized authority. The health impact alone of tobacco warrants significant investment in strong tobacco control programs. However, the health consequences of tobacco use are only one side of the tobacco epidemic. It is important that policy makers reflect on the values and aspirations of people everywhere for a fair globalization, one which respects the diversity of needs and perspectives, and where there is greater opportunity for all. The task ahead is to generate the political will which can turn commitment into action. Progress demands a more open exchange and an improved quality of dialogue between all concerned. I would suggest that new initiatives which respond to current needs for the better governance of globalization, both between countries and within them. They are based on the awareness of growing interaction and interdependence and guided by a sense of solidarity. Additionally, it is necessary to encourage a wider participation of people and countries in the making of policies which affect them. They require those with the capacity and power to decide in governments, parliaments, business, labour, civil society and international organizations, to assume their common responsibility to promote a free, equitable and productive global community. It can be difficult to generate sufficient political will to overcome opposition, including from the tobacco industry, to raising tobacco taxes. The tobacco industry has long opposed any strengthening of tobacco control measures, and is particularly active in attempting to prevent any type of tax increase leading to actual higher prices. The industry makes false claims of economic harm caused by higher taxes, which are not borne out by the evidence. One particular claim is that higher taxes lead to increased smuggling and illicit trade, but again there is no evidence to support this. But because tobacco taxes are generally better accepted than other types of taxes, it is possible to achieve widespread public support, even among tobacco users, especially if at least some of the new tax revenues are used for tobacco control, health promotion and other public health program. Hence, ensuring people in all countries have access to the benefits of a more health friendly globalization.
Notes
- 1. http://www.who.int/trade/glossary/story089/en/ 2. http://www.who.int/tobacco/global_report/2013/appendix_x/en/ 3. http://www.statista.com/statistics/261173/leading-countries-in-tobacco-production/ 4. http://monographs.iarc.fr/ENG/Monographs/vol83/mono83.pdf 5. http://www.who.int/tobacco/publications/en_tfi_gbd_intro_methods_results.pdf?ua=16. http://ash.org/wp-content/uploads/2014/01/full-report.pdf 7. https://www.ftc.gov/sites/default/files/documents/reports/annual-report-congress-regarding-operation-hart-scott-rodino-premerger-notification-program-federal/050809cigrpt.pdf8. http://cancercontrol.cancer.gov/brp/tcrb/monographs/19/m19_complete.pdf
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML