-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2016; 6(4): 99-105
doi:10.5923/j.phr.20160604.01

Awareness Status and Associated Risk Factors for Hypertension among Adult Patients Attending Yala Sub-County Hospital, Siaya County, Kenya
Bob O. Awino1, Lilian A. Ogonda2, Grace C. Barno3, Ng’wena G. Magak4
1Department of Clinical Services, Bondo Sub-County Hospital, Bondo, Kenya
2Department of Biomedical Sciences, School of Public Health, Maseno University, Maseno, Kenya
3Department of Educational Management and Policy studies, Moi University, Eldoret, Kenya
4Department of Medical Physiology, School of Medicine, Maseno University, Maseno, Kenya
Correspondence to: Bob O. Awino, Department of Clinical Services, Bondo Sub-County Hospital, Bondo, Kenya.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Hypertension affects approximately 26% of the adult population worldwide and is a significant risk factor for cardiovascular diseases, stroke and renal failure. In Kenya, hypertension accounts for approximately 64% of stroke cases. However, information regarding its prevalence, awareness status and associated risk factors among patients seeking healthcare from hospitals in Kenya is unknown. Yala sub county hospital is one of the largest sub-county rural hospitals in Siaya County. In the past four years it had experienced increased number of patients diagnosed with high blood pressure (BP). But due to frequent breakages of BP monitoring machines and fewer medical staff at the outpatient department could make the reported data on hypertension not to be relied upon. This might lead to the true prevalence rate of the problem being underestimated. Moreover, lack of awareness regarding the disease status increases incidence of complications and mortality. The aim of the present study was to determine the prevalence, awareness and determinants of hypertension among adult patients attending Yala sub-county hospital, in Gem sub-county, Kenya. This was a hospital based cross-sectional study conducted on 393(144 males and 249 females) randomly sampled patients aged 18 years and above between February and March 2015. Study participants were considered to be hypertensive when they presented with a systolic blood pressure (BP) of 140mmHg and above and/or a diastolic BP of 90mmHg and above. Individuals who reported being on regular anti-hypertensive therapy were also grouped together with the cases. Data on demographics, social economic, exposure history to various potential risk factors for hypertension and awareness was collected using a pre-tested Questionnaire. Logistic regression analysis was used to identify factors associated with hypertension. The prevalence of hypertension in the study participants was at 36.9% (145/393) (male 38.9%, 56/144, females 35.7%, 89/249; p = 0.533). Out of all the hypertensive cases 85(58.6%) were found to be aware of their status and out of the 85 cases 75(88.1%) were on medication but only 21 of them (28.4%) had controlled blood pressure (systolic blood pressure <140mmHg and diastolic blood pressure <90mmHg. Factors independently associated with hypertension in this population were age > 30 years OR= 12.0 (2.7 - 52.3), body mass index (overweight, OR= 2.98 (1.85 - 4.79) and Obesity, OR= 4.23 (2.15 to 8.30), current tobacco smoking OR= 2.63 (1.32 - 5.23), high waist circumference, OR= 2.39 (1.57 - 3.64). Increasing education level was however associated with decreased likelihood of suffering hypertension. These findings suggest that in the Gem community hypertension is most prevalent among adults aged 30 years and above and the risk factors are the same as those that have been reported in other population (body mass index, obesity, high waist circumference, tobacco smoking and low education levels). Approximately half of the hypertensive cases were aware of their status and the available hypertension medications did not fully control the high pressure in all the cases. Therefore, there is need to have community screening programs, instituting awareness raising programmes through health promotion to target individuals at risk and interventions aiming at reducing the associated factors identified in this study.
Keywords: Hypertension, Prevalence, Risk factors, Awareness, Hospital-based study
Cite this paper: Bob O. Awino, Lilian A. Ogonda, Grace C. Barno, Ng’wena G. Magak, Awareness Status and Associated Risk Factors for Hypertension among Adult Patients Attending Yala Sub-County Hospital, Siaya County, Kenya, Public Health Research, Vol. 6 No. 4, 2016, pp. 99-105. doi: 10.5923/j.phr.20160604.01.
Article Outline
1. Introduction
- Hypertension is a major public health problem that affects approximately 26% of adult population worldwide [1] and causes about 7.1 million deaths per year [2]. In Sub-Saharan Africa, the disease prevalence ranges from 6 to 48 % [3]. The disease is categorized as either essential (primary) or secondary whereby essential hypertension is a rise in blood pressure with no identifiable cause that increases the risk of cerebral, cardiac and renal events [4]. Although the cause is unknown, several factors including age, gender, obesity, lifestyle (diet, lack of physical activity), stress and genetic factors [5] [6] increase the risk of developing essential (primary) hypertension. In secondary hypertension the elevated blood pressure is as a result of an underlying medical condition or medication. Some of the causes of secondary hypertension include kidney diseases, disorders of endocrine glands including hyperthyroidism, medications such as corticosteroids and use of oral contraceptives [7]. Secondary hypertension occurs in approximately 10% of adult hypertensive cases [8].Data on the prevalence and/ or associated risk factors of hypertension in Kenya particularly in rural settings in the western regions of the country is very limited. Published initial survey of 1986 was undertaken in a regional centre, among both rural and urban residents, reported non-standardized hypertension prevalence of 6.4% [9]. Another regional cross-sectional study done in 2008, restricted to subjects aged over 50 years and conducted in predominantly urban population in Nakuru District, reported a prevalence of 50.1% [10]. Similarly, a survey done in rural Kenya which included a sample of a specific target group composed of members of dairy farmer cooperatives and their families in the Nandi district, showed age-standardized prevalence of hypertension of 21.4% [11]. There is therefore need for documentation of the prevalence, and possible risk factors of hypertension among clients attending hospital visits in western Kenya. The present study was carried out to determine the prevalence, awareness and determinants of hypertension among clients attending Yala sub county hospital, a rural hospital in Gem Sub County, in western Kenya.
2. Methods
2.1. Setting and Sample Selection
- Yala Sub county hospital is a rural hospital situated in Yala division, Gem Sub County, of Siaya County. It is situated 42 kilometers northwest of Kisumu City and is approximately 500 meters off Kisumu- Busia road. Yala is one of two divisions of Gem Constituency, Siaya County, Western Kenya. Yala division has a population of 83,823 with an urban population of 2,438 [12]. The hospital has a catchment population of approximately 24,000 persons. Yala is situated at 0.1° North latitude, 34.53° East longitude and 1373 meters elevation above the sea level. Main economic activities include subsistence farming, livestock keeping, rice farming and small scale trading. Between February and March 2015, a sample of 422 outpatient clients attending treatment at the hospital was enrolled in this study. Study participants were selected through both simple random and systematic sampling. The first study participant of the day was selected through simple random procedure. This was done by giving the first five participants random papers labeled one to five, the client who picked paper number one became participant number one in the study. After which the subsequent participants of the day was through systematic sampling (after every 14th patient). The sampling interval was obtained by dividing 6000 (previous year’s two months outpatient visit, as sampling frame) by 422 (the sample size). This procedure of interval selection was repeated daily until a sample size of 422 participants was met. Only consenting adults aged 18 years and above were eligible for inclusion in the study. The conduct of this study was approved by Maseno University Ethical Review Committee.
2.2. Study Design and Measurements
- This was a cross-sectional study in which trained research assistants used standardized questionnaires to collected data on demographics, social economic and exposure history to various potential risk factors for hypertension, Blood pressure (systolic blood pressure (BP) 140mmHg and/or diastolic BP 90mmHg, or being on regular anti-hypertensive therapy), Body weight and height and waist circumference of participants. Potential risk factors for hypertension were classified into two categories, modifiable and non-modifiable. The modifiable potential risk factors measured included: history of alcohol use; tobacco use; fruit and vegetable consumption; physical activity; weight, occupation, highest level of formal education attained. Thenon-modifiable potential risk factors assessed included: height, age and first degree family history of hypertension.Height (in meters to the nearest 0.5 cm) was measured without shoes using a wooden platform and a height rule. Weight (to the nearest 0.5 kg) was measured with the use of an automated scale. Participants were permitted to keep on light clothing and without footwear. Body mass index (BMI) was calculated as body weight (kg) divided by height squared (m2). The blood pressure (systolic and diastolic) was measured with the participant in a seated position, and after at least 3 min rest. The BP measurements were performed on the right arm using automated sphygmomanometers (OMRON M3 HEM-7200-E Omron Matsusaka Co Ltd, Kyoto, Japan). Special attention was given to the use of appropriate cuff sizes (13×23 cm or 16×30 cm). Three blood pressure readings were taken 1 minute apart. The average of the last 2 readings was used in the analysis [13].
2.3. Statistical Analysis
- Data was analyzed using both descriptive and inferential statistics. Overall prevalence of hypertension was calculated as the percentage of participants classified as hypertensive, with all study participants as the denominator. Comparisons, among groups for quantitative data and prevalence of hypertension were done with the χ2 test. Chi square test was used to determine significance between independent variables (age, sex, level of education, marital status, waist circumference, BMI, occupation, smoking status, alcohol drinking status, family history of hypertension, physical activity) and hypertension. Significant variables at p≤0.3 were entered into logistic regression model to determine factors predictive of hypertension. Finally, factors which remained significant at p≤0.05 after adjusting for all others were considered independently associated with hypertension. Associations are reported in terms of odds ratios (OR) with 95% confidence intervals (CIs).
3. Results
3.1. Characteristics of Study Population
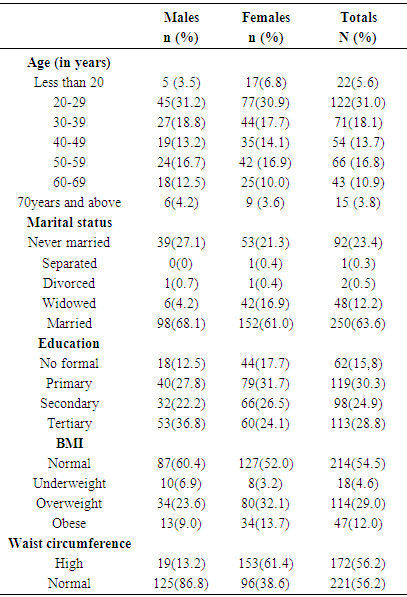
- Data collected from three hundred and ninety three subjects were analyzed. This was 93.1% (393/422) response rate. The sex distribution of the study population was 249 (63.4%) females and 144 (36.6%) males. The overall mean age was 39.53±16.43 years (Males = 40.21±16.46 years, Females = 39.14±16.42 years) (Table 1).
|
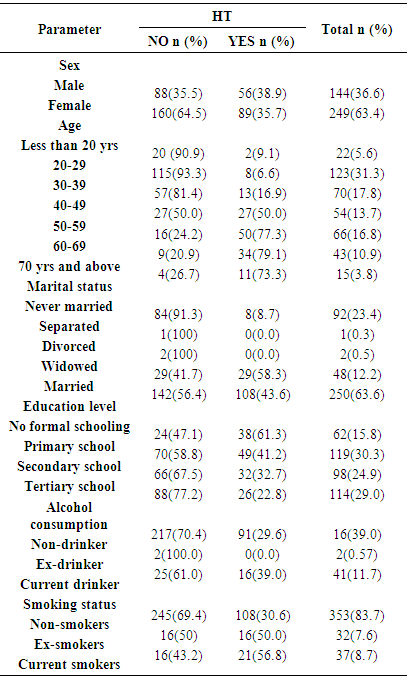
3.2. Prevalence of Hypertension
- The overall prevalence was 36.9%, 145/393; (35.7%, 89/249 in women and 38.9%, 56/144 in men) In terms of trend of hypertension with age, there was noted a progressive increase of hypertension prevalence with age. This pattern was seen in both sexes. With respect to marital status, prevalence was highest among the widowed 60.4%, n=29 and least among those participants who were not married 8.7%, n= 8. In terms of occupation prevalence was highest among the government employed 52.9%, n=27; and least among the students. The study results showed that hypertension prevalence was highest (61.3%, n=38) among those with no formal education and least (8.1%, n=7) among the students. Prevalence was almost the same among those with positive family history and those without positive history, 38.6% and 36.4% respectively. Among smokers, current smokers had the highest prevalence (56.8%, n=21) and non-smokers had the least (30.6%, n=108). In terms of alcohol consumption, current drinkers had the highest prevalence (39%). Those engaging in vigorous physical activity had the least (35.3%, n=60) prevalence of hypertension (See table 2).
|
3.3. Awareness Level of Hypertension
- The study results showed that out of the 145 participant who exhibited hypertension only 85 (58.6%) were aware of their hypertensive status, of which 30 (35.3%) were male and 55(64.7%) female as shown in figure 1.
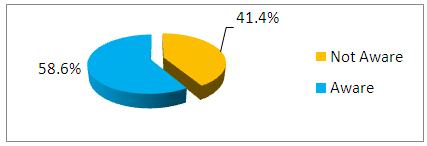 | Figure 1. Awareness status (Awareness was defined as a positive response to question, ‘did a doctor ever tell you that you have (had) high BP?’) |
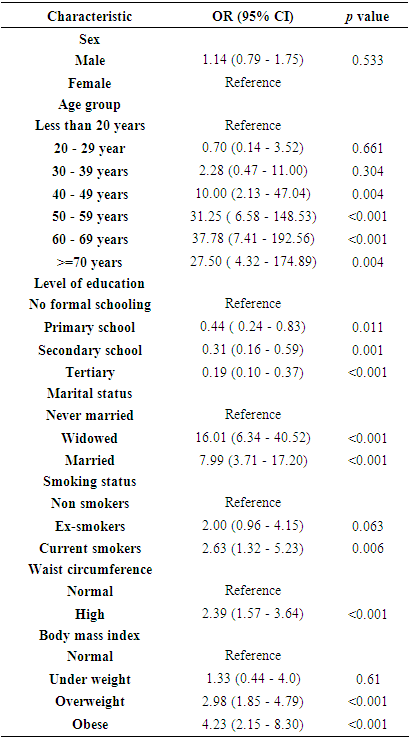
3.4. Associated Risk Factors of Hypertension
- Using binary logistic regression the following associated risk factors were identified as independent predictors of hypertension; age, marital status, employment status, smoking, BMI, waist circumference and education level. After controlling for confounding, the odds of being hypertensive in the males was OR (95% CI) = 1.14 (0.79 - 1.75), but this was not statistically significant, p = 0.533. Increasing age was statistically significant independent predictor of hypertension; respondents in the age bracket of 40-49 were 10 times likely to be hypertensive than those below 30 years OR (95% CI) = 10.0 (2.13-47.04) p= 0.004. In terms of marital status, the widowed were 16 times more likely to be hypertensive than those never married, OR (95 CI) = 16.01 (6.34-40.52) p = <0.001. With regards to smoking status, the current smokers were approximately 3 times likely to be hypertensive than the non smokers, OR (95% CI) = 2.63 (1.32-5.23), p= 0.006. Increasing BMI, was also an independent predictor for hypertension; the obese were 4 times likely to be hypertensive than those with normal weight, OR (95% CI) = 4.23 (2.15-8.30) p = 0.001. Participants with high waist circumference were 2 times likely to have hypertension than those with normal waist circumference OR (95 %CI) = 2.39 (1.57-3.64) p = <0.001. The summary of the results are as shown in table 3.
|
4. Discussion
4.1. Prevalence of Hypertension
- The prevalence of hypertension in this rural based hospital was 36.9% (36.6% of males and 63.4% of females). This prevalence falls within the reported range (6 to 48%) of hypertension cases in the Sub-Saharan Africa [3]. However, compared to specific reports, this estimate is higher than those reported from South Africa 23% [14], in Eritrea 16% [15], and in Rukunguri Uganda 30.5% [16]. Furthermore, comparing the present findings with those of specific groups in Kenya, it was found to be apparently higher than that found by a survey done on a group of dairy farmers in Nandi district which was at 21.9% [11] and adult population in two slum settlements in Nairobi which was at 19% [17]. This prevalence is however lower than the prevalence of 50.1% reported in a community of Nakuru district [10]. The prevalence difference may be due to the fact that this present study included a wide age range i.e., 18 years of age and above, while the Nakuru study had participants from 50 years and above. Since it has been found that hypertension is most common in the middle age and elderly [18].
4.2. Awareness Status of Hypertension
- Correct knowledge of blood pressure status can be regarded as the first step in the prevention of the cardiovascular complications of hypertension as such knowledge can serve as a platform for making necessary health decisions and developing adequate healthy behavior and lifestyle. In this study, 58.6% of the hypertensive individuals were aware of their hypertension status. Though this results was slightly higher compares to that found in studies done in Angola (21.6%), [19] in Uganda (10%) [16] and in rural Kenya of Nandi district (6%) [11]. The difference could be due to variations of the study settings and methodologies. However the awareness is lower than that found by studies done in done in developed countries. In the USA, for instance, awareness of hypertension is as high as 76% [22] reflecting the success achieved by a coordinated policy to detect individuals with higher-than-optimal BP levels.Awareness status of hypertension in this study was significantly higher among female participants. Similar findings were also demonstrated by Van de Vijver [17] and Pires [19]. This could be explained by the fact that females appear to be more concerned with their health compared to males, and this is expected since health status may affect body image which is more important for females. This difference among the sexes could also be explained by the fact that women are more in contact with healthcare services than men through maternal child health programs. The study also demonstrated that awareness status increased with increasing age in men and women. Similar finding was also noted by Mathenge et al., (2010) [10].
4.3. Associated Risk Factors for Hypertension
- In terms of education, this study found an inverse relationship between hypertension and education. The participants who reported tertiary education were less likely to be hypertensive than their counterparts who reported primary education. The study findings are similar to those from a study conducted in an urban population in early epidemiological transition in Tanzania where Bovet et al., (2002), reported that non-educated men were more likely to have higher systolic blood pressure than those with primary education (p< 0.01) [6]. Likewise in the developed world, studies have consistently revealed an inverse education-blood pressure association. In a multi-country study by Stamler (1992), it was reported that age-adjusted systolic blood pressure was 1.3mmHg higher (p-value = 0.05) for men and 4.5mmHg (p-value < 0.001) for women with 10 fewer years of education. The less educated were found to have higher sodium excretion, greater body mass, and a higher alcohol intake leading to increased blood pressure [23]. The participants who reported to be widowed were more likely to be hypertensive than their counterparts. Capell et al., (2001), showed that psychological factors can affect the entire neuroendocrine system ultimately leading to hypertension [24]. This may be associated to the psychological stress faced by this group of people. The findings in this study showed an association of cigarette smoking and hypertension, with current smokers being 2 times more likely to be hypertensive than the non-smokers. This finding is similar to those obtained by De Cesaris et al., 1992 and Dochi et al., 2009, who found out that significant odds ratio of smoking, were 1.13 for hypertension and 1.15 for systolic hypertension [25] [26]. Cigarette smoking makes blood vessels and blood cells sticky, allowing cholesterol and low density lipoproteins to build up inside them leading to a condition known as atherosclerosis. This in turn can lead to raised blood pressure and clot formation. Likewise it can cause increased blood pressure by increasing sympathetic activity especially a greater effect on sympathetic drive to the heart than to peripheral blood vessels [27]. Participants with a BMI greater than 25 were more likely to be hypertensive compared to those with a BMI of 25 or lower. Similarly, in Tanzania, Bovet et al., (2002) found that body mass index was strongly and independently associated with systolic and diastolic blood pressure (1.01 mmHg systolic BP per 1 kg/m2 increase in BMI) [6]. In Nigeria, Agyemang (2006) has also reported an independent association between BMI and BP [18]. Likewise Önal et al., (2004), found that hypertensive adults aged 25 years or older were twice more likely to be overweight or obese in Istanbul, Turkey [29]. These findings imply that having a normal weight, or losing weight among those who are overweight or obese, would reduce the chances of developing hypertension. Perhaps the risk imposed by these is all reflected in the BMI of the individual.With respect to age, adults aged 40 years or older were more likely to be hypertensive compared to those in the younger age groups. This is consistent with findings from Edwards et al., (2000), they found that hypertensive men and women in rural and urban areas in Tanzania tended to be significantly older compared to those who were not hypertensive [30]. Likewise, study done by Wamala et al., (2009), Participants with hypertension were significantly older with an average age of 44.5, compared to normal- tensive participants who had an average age of 37.6 [16]. Advancing age increases the risk of exposure to the lifestyle risk factors for hypertension and hence the observed increase in hypertensive risk with aging.
5. Conclusions
- These findings suggest high prevalence of hypertension among those who are more than 30 years and above and approximately half of them unaware of their hypertensive status. Therefore, there is need to have community screening programs, instituting awareness raising programmes through health promotion to target individuals at risk and interventions aiming at reducing the associated factors identified in this study.
ACKNOWLEDGEMENTS
- We are grateful for the guidance and support offered by the staff of Maseno University and Yala Sub-County Hospital.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML