-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2016; 6(2): 52-58
doi:10.5923/j.phr.20160602.04

An Epidemiological Study of Drug Resistant Tuberculosis Cases: Survey in the Northern Part of Bangladesh
Himangshu Karmaker 1, Md. Abul Basar 2, Md. Reazul Karim 3, Md. Masud Rana 3, Md. Golam Hossain 4, Md. Abdul Wadood 5, Md. Rafiqul Islam 3
1Divisional Coordinator, MSH - Challenge TB Project, Rajshahi, Bangladesh
2Training Officer, DASCOH, Dingadoba, Rajpara, Rajshahi, Bangladesh
3Department of Population Science and Human Resource Development, University of Rajshahi, Rajshahi, Bangladesh
4Health Research Group, Department of Statistics, University of Rajshahi, Rajshahi, Bangladesh
5Md. Abdul Wadood, Deputy Chief Medical Officer, Medical Centre, University of Rajshahi, Bangladesh
Correspondence to: Md. Rafiqul Islam , Department of Population Science and Human Resource Development, University of Rajshahi, Rajshahi, Bangladesh.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Drug resistant tuberculosis (DR TB) is a global concern due to high fatality, and high cost and hazardous treatment. It is important to know the epidemiological factors of DR TB for effectively controlling this infectious disease. The aim of the present study was to indentify the epidemiological factors of DR TB patients in the Northern part of Bangladesh. Methods: A cross-sectional study was conducted of registered DR TB patients at two chest diseases hospitals (CDH) in Northern part of Bangladesh. Data was collected from 164 registered DR TB cases (male 113 and female 51) using pre and post tested standard questionnaire. Some information was also collected from available records at those hospitals. Results: The present study demonstrated that male (68.9%) was more affected by DR TB than female (31.8%). A decreasing trends was observed in DR TB patients with increasing age (excluded, age group (6-15)). When we adjusted age and sex, higher percentage of DR TB cases was especially pronounced among who were living in Rajshahi division (72.6%) and rural areas (86%), came from ‘Failure of Category–1’ (24%), ‘Relapse after Category–1’ (33%) and ‘Non Converters of Category–1’ (21%) and low income family (44%, BDT ≤10000). Among the cases, 32% were illiterate and 28% had primary level education, and the percentage of male DR TB patients habituated smoking were 56.63%. Conclusions: This study suggested that sex, age, type of treatment, residence, education and smoking status were important factors for getting MDR TB. It is expected that this study can help government to take activities for controlling and prevent MDR TB disease.
Keywords: Drug Resistant Tuberculosis, Northern Part of Bangladesh, Cross Sectional study
Cite this paper: Himangshu Karmaker , Md. Abul Basar , Md. Reazul Karim , Md. Masud Rana , Md. Golam Hossain , Md. Abdul Wadood , Md. Rafiqul Islam , An Epidemiological Study of Drug Resistant Tuberculosis Cases: Survey in the Northern Part of Bangladesh, Public Health Research, Vol. 6 No. 2, 2016, pp. 52-58. doi: 10.5923/j.phr.20160602.04.
Article Outline
1. Introduction
- Tuberculosis (TB) is a major Public health problem in Bangladesh. Considering the estimated number among total population, Bangladesh is a High TB Burden and High DR TB Burden country and it ranks 7th among 22 High TB Burden Countries [1]. The history of Tuberculosis in Bangladesh has different stages. 1965, tuberculosis services were mainly curative and based in TB clinics and TB hospitals. TB services were expanded to 124 Upazila Health Complexes (UHCs) during the 2nd Health and Population Plan (1980-86), and were operationally integrated to Leprosy during the 3rd Health Population Plan (1986-91) under the Mycobacterium Disease Control (MBDC) unit of the Directorate General of Health Services (DGHS). The National TB Control Program (NTP) adopted the revised DOTS strategy during the 4th Population and Health Plan (1992- 98) under the project “Further Development of TB and Leprosy Control Services”. The NTP started its field implementation in November 1993 in four Thanas (Upazilas) and progressively expanded to cover all Upazilas by mid 1998, The NTP was integrated into the Communicable Disease Control component of the Essential Service Packages under the Health and Population Sector Program (HPSP). In 2003, HPSP was renamed as Health Nutrition and Population Sector Program (HNPSP) (2003-2011). Now Ministry of Health and Family Welfare (MOHFW) has been implementing the Health Population and Nutrition Sector Development Program (HPNSDP) for a period of five years from July 2011 to June 2016. In all the sector programs tuberculosis control program has been recognized as one of the priority program [2]. The program is maintaining the high treatment success rates from the beginning and met the target of 85% treatment success since 2003. The program has been maintaining the treatment success rate of New Smear Positive (NSP) cases over 90% since 2006. Regarding case notification of NSP cases, the program made slow and steady progress from 2003 to latest year. In 2003 the notification rate of NSP cases was 40/100,000 population. It became 61, 73, 74, 70.5 & 68 during 2005, 2006, 2009, 2010 & 2013 respectively [2].At present, DR TB cases in Bangladesh are relatively low and a few XDR TB Cases exist. Along with the present DR TB Case load, Bangladesh falls into the category of High MDR TB Burden Country and ranks 13th among 30 such High MDR TB Burden Countries [1]. The NTP has carried out its first nation-wide Drug Resistance Survey (DRS) in Tuberculosis Patients in collaboration with WHO and Supra National Reference Laboratory (SNRL), ANTWERP, Belgium in 2010-2011. The result shows the overall number of MDR TB cases is low, 1.4% among new cases and 28.5% among retreatment cases. Although the rates of MDR TB in Bangladesh do not appear to be high, but the absolute number of MDR TB Cases is higher considering the overall high TB burden. MDT TB prevalence of 1.4% in new cases and 28.5% in Retreatment cases translate approximately an estimate of 4496 MDR TB cases among notified TB cases in 2013 [3]. In August 2008 NIDCH started enrollment of MDR TB patients with GLC approved 24 months regimen and supported by the Global Fund. By the end of December 2013 a total of 1301 confirmed MDR TB patients including 330 in 2013 have been enrolled. As a part of Programmatic Management of Drug Resistance TB (PMDT) plan NTP established one Regional TB Reference Laboratory (NTRL) at Chest Disease Hospital (CDH) of Chittagong in 2011 and also managing MDR TB patients from that year. In 2013 NTP has also started managing MDR TB in CDH Pabna and Khulna. The MDR TB patients are also managed in the CDH of Rajshahi division and in three other hospitals of Damien Foundation at Jalchatra under Tangail Hospital, Anantapur under Netrakona District and Shambhuganj under Mymensingh district with shorter regimen of 9 months and supported by Damien Foundation, Bangladesh under operational Research. Since May 2005 those centers have been managing MDR TB patients, and by end of December 2013 a total of 1161 patients including 189 in 2013 have been enrolled [2]. It is evident that the gap between estimation and diagnosis of DR TB cases is very high in Bangladesh. Those missing DR TB cases are a very big threat for the society as well as for the country. From the above discussion, we can have a clear picture of the problem of DR TB case diagnosis and management situation in Bangladesh. In comparison with the yearly estimation, the diagnosis is very low. In 2011, 2012 & 2013 NTP had diagnosed only 10%, 12% and 15% of the estimated cases. To increase the DR TB case detection, we have to know the epidemiological factors of presently detected DR TB cases. From the study we will be able to know the most vulnerable and risk groups for the development of DR TB. Thus we shall be able to design strategy to find DR TB cases in most effective way. It will also help to manage DR TB case in most efficient way. There are large numbers of studies on DR TB issues that had been carried out in different countries of the world. However, the study with DR TB patients has been poorly documented in Bangladeshi population. The purpose of the present study was to identify the epidemiological factors of DR TB among registered patients at two chest disease hospitals in the Northern part of Bangladesh.
2. Methods
- The northern part of Bangladesh consists of 2 divisions; Rajshahi and Rangpur. There are 16 districts under these two divisions. The two divisions cover together an area of 34,338 square kilometers which is 23.26% of the total area and have a population of 36,541,453 which is 23.63% of the total population of the country [2]. There are 4 Chest Disease Hospitals (CDH) at Rajshahi and Rangpur division for the treatment of TB and other chest diseases. Only Rajshahi and Pabna CDH among 4 CDH have the facility to treat DR TB patients. DR TB patients, who are diagnosed from different Upazilas of Rajshahi and Rangpur division, have to get admission and registered under those two hospitals. After necessary investigations and formalities, treatment is initiated for each DR TB patients. After certain period of initial treatment at those hospitals, patients are shifted to community to continue the rest of the treatment. The DR TB management program is implemented countrywide following a National Guideline. Present study was a cross-sectional descriptive study. The study area covered all 16 districts under Rajshahi and Rangpur divisions. The period of the study was May 2014 to December 2014. The target population included all registered DR TB patients at Rajshahi & Pabna CDH during the year 2013 and 2014. Non-random purposive sampling technique was used for selecting the sample. During the year 2013 & 2014, total 156 and 62 DR TB cases were registered at Rajshahi and Pabna CDH respectively. There were total 218 DR TB patients at both hospitals during study period. Minimum sample size was determined as 140 after statistical calculations. Finally 164 respondents were brought under the study to cover the minimum sample size. DR TB patients registered at Rajshahi & Pabna CDH but residing at out of the study area were excluded from the study to make it confined within Rajshahi & Rangpur divisions.Data were collected following pre-coded, open ended, pre and post tested questionnaire. One to one direct interview method with respondents was used in present study. Some data were also collected from registers, treatment cards and other documents of individual patients available at Rajshahi & Pabna CDH. The completed questionnaire was collected and checked for the completeness and clarity of the information to exclude missing or inconsistent data and then compiled together. Data was edited properly before analysis.
3. Statistical Analysis
- Frequency distribution was done in this study. Data analysis was done by using appropriate statistical software. Final analysis of the data was carried out using percentage, absolute numbers for categorical variables in IBM SPSS 20. For some purpose, Excel program was also used for analyzing the data.
4. Ethical Approach
- The study was conducted following the ethical consideration and all ethical issues were handled with appropriate care. A written document describing the purpose of the study and the individuals’ rights as study participants was prepared and it was informed clearly for every individual. All rules and regulations of the ethics committee, Institute of Biological Science (IBSC), Rajshahi University, Bangladesh have been followed in this study. Written consent forms were collected from each participant after a detailed oral explanation about the study.
5. Results
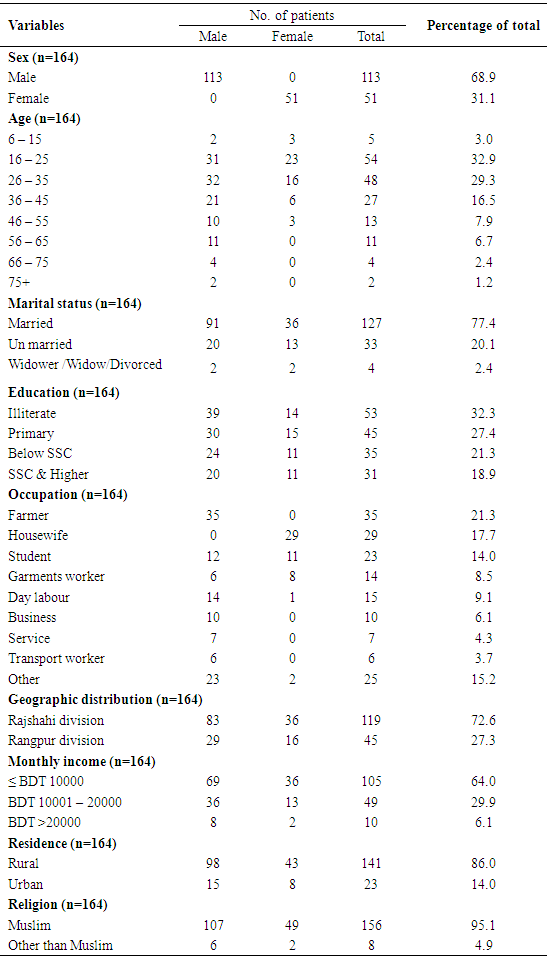
- Socio demographic profile Among 164 participants, 113 were male (68.9%) and 51 were female (31.1%). M:F was 2.2:1. Minimum age was 8 and maximum age was 85. The most vulnerable age for MDR TB was marked as 16 to 45. In this group total number of respondents was 129 which were 78.7% of total respondents. Highest number of respondents was from 16 – 25 (33%) age group, second highest was from 26 – 35 (29%) age group and third one was from 36 – 45 (16%) age group. We have also the division and district wise distribution of 164 respondents. It was found that 72.6% respondents are from Rajshahi division and only 27.4% respondents were from Rangpur division. In the study, we had checked the occupation of the respondents. Male had more variety in occupation than female. The data showed that most of the female are housewife. They were 17.7% among total and 56.86% among all female. For male, most were farmer and they were 21% among total & 30.97% among total male. There was a good number of students among male and female. Student occupied 14% among total respondents. 8.5% of the total respondents were Garments worker. All sorts of day labor accounts for 9.1%, different service occupied 4.3% and business occupied 6.1% among the respondents (Table 1). The analysis displayed that a high number of respondents were illiterate. Total 32.3% participants had no education. Among Male, 34.5% and among Female, 52.94% were illiterate. 28% of respondents had primary level of education. It was found by the study that most of the respondents were within family income group of BDT ≤10,000. It consisted 64% among the total. In 2nd group there were 49 respondents which consisted of 30% among total having a family income of BDT 10001 - 20000. Another 6% came from the group of ≥20,001. In general it can be said that most of the MDR TB patients were from very low income group. It is observed by the study that most respondents were from rural area (86%) and only 14% were from urban area. Among 164 respondents, 95.1% were Muslim, 4.9% were Hindu and Christian (Table 1).
|
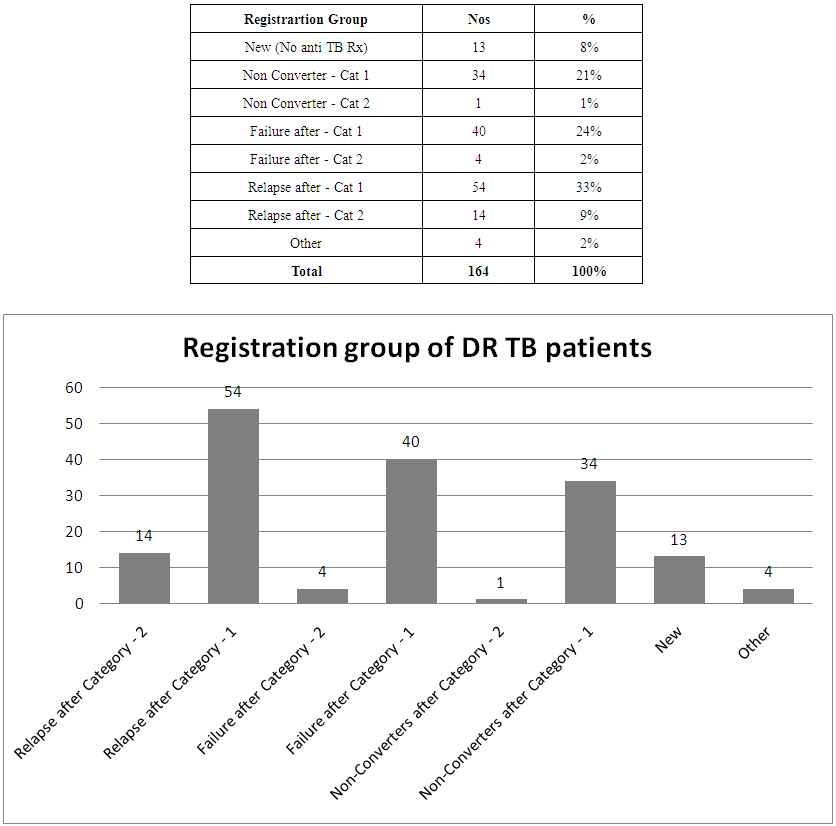 | Figure 1. Registration group of the respondents |
|
|
|
6. Discussion
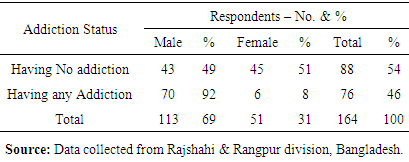
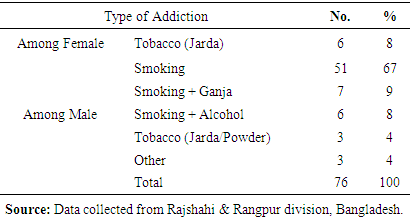
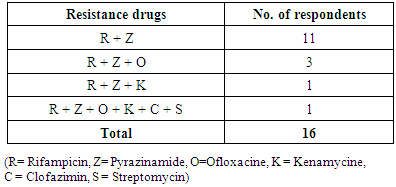
- The terminology “DR TB” and “MDR TB” both are used in this study synonymously. By definition they are different but the DR TB management program treats DR TB cases diagnosed by GeneXpert machine as MDR TB and they are treated under standard regimen of MDR TB [3]. For MDR TB, TB patients must have resistance to two most potent Anti TB Drugs – Rifampicin and Isoniazid. Similarly, DR TB is specified for patients who have resistance to any Anti TB Drugs. So it can be said that, all MDR TB are DR TB but not all DR TB are MDR TB. In our study, the DR TB patients are detected through GeneXpert MTB/RIF, a rapid diagnostic tool, which detects only Rifampicin resistance. But it has been proven by most of the studies that 95-99% Rifampicin resistance has co-resistance with Isoniazid. So, evidentially they are termed as DR TB but conceptually they are considered as MDR TB as we do not have any rapid testing tool to diagnosis Isoniazid resistance. To have evidence of Isoniazid resistance, it needs to perform Culture and Drug Susceptibility Test (DST) which takes comparatively longtime and not supportive in public health approach. It needs to make clear that the drugs that are used for normal TB treatment are called 1st line drugs. They are – a) Injection Streptomycin, b) Capsule Rifampicin, c) Tablet Isoniazid, d) Tablet Pyrazinamide and e) Tablet Ethambutol. In case of unexpected results in 1st line treatment, susceptibility tests are done for those drugs. The drugs that are used for DR TB treatment are called 2nd line Drugs. They are many in number and a combination is used by physicians. Any national program usually use combination (regimen) approved by WHO. The regimen that is used in Bangladesh National TB Control Program is a 24 months regimen and has the following drugs: a) Injection Kenamycin, b) Tablet Levofloxacin, c) Tablet Cyclocerine, d) Tablet Protheonomide and e) Tablet Pyrazinamide. Physician may use alternative from same group for adverse effect due to any specific drug. This study was conducted with a view to analyze the socio-demographic and epidemiological factors among registered DR TB cases at two chest disease hospitals of northern part of Bangladesh. Among the study subjects, male were more prevalent and the age group from 16-45 were mostly vulnerable. The mean age was 33.85 years. In late age, women were less likely to develop MDR TB but there were evidences of male having TB in the age of 80 or more. A study was conducted by Bhatt et al. (2012) at Ahemedabad of India on age and sex distribution of MDR TB [4]. That study had almost same finding in this regard. The study reports 2/3rd male and highest age group was 16-45 [4]. It should be a concern of policy maker’s to prevent DR TB in most productive age. More MDR TB was diagnosed at Rajshahi division and less in Rangpur division. It was a very important finding from the point of geographical distribution of MDR TB in Bangladesh. Number of TB case detection was higher in Rangpur division than Rajshahi division [2]. If we calculate 1.4% MDR among new and 29% among re-treatment TB, the number of DR TB cases should be higher at Rangpur division. But there were only 27.44% among 164 study subjects. It needs further research to explore the facts and under lying causes of low DR TB detection at a particular region. Most of the MDR patients had no education or low education. So, awareness level, motivation, understanding of risks may be low due to education. As an impact of no or low education can lead to creation of MDR TB. We did not find much study on educational impact of MDR TB. But it was also found in the study performed by Bhatt et al. (2012) where the educational level of the MDR cases was found primary level. Further study may help to conclude the findings [4]. Among the 164 respondents, 150 had at least one episode of Anti TB drug history which was 91.5%. At the same time, 12.2% had history of taking 2 episode of ATT. Most MDR cases were diagnosed from Category 1 or having no treatment. They were about 80%. From re-treatment category MDR cases were 20% of total. Primary MDR may be more emerging as around 8% DR TB had not received any ATT and around 21% had received only 2 months of ATT mostly under DOT. It needs to conduct an analytical study only on this topic. The finding of this study also provokes us to conduct Drug Resistance Survey (DRS) to know the latest DR TB pattern. It is commonly said that TB is a disease of poverty. It is also true for DR TB. The study showed that MDR TB was more prevalent among low socio-economic group of people. Due to low income, their life style may be affected positively to develop MDR TB. This was also established by several other studies [5]. In general, rural people were mostly affected by MDR TB and there was no ethnic sensitivity. DR TB developed from different religion group. This study was not suitable to make any comment on whether any religion is more vulnerable for TB or not. A number of occupations had been identified among the respondents. This study showed that DR TB a generalized disease. But at the same time some occupations were found more prone for developing DR TB. In this category garments workers are remarkable. Previous history was important for developing DR TB. Most of the MDR cases had previous anti TB drug history [5, 6]. Regularity of treatment and regular supervision of Drug intake (DOT) was important for development of DR TB.In this study, we had inquired about presence of contact history either with TB or DR TB. It was considered an important risk factor. Contact with MDR TB is most likely to produce MDR TB. MDR TB cases may have contact with Non-MDR TB but there may not have association to be transmitted from each other. Both may have different source of infection. It was identified from the study that 44 DR TB patients among 164 (26.8%) had history of contact with TB or DR TB patients. Among 44 DR TB cases 20 had history of contact with DR TB patients. This finding was very alarming and needs to take initiative to detect DR TB cases early and put them on treatment. Some other study also recommended the same [5]. In this study we had also inquired about co-infection of DR TB cases with other chronic disease. We had found that 9.1% DR TB patients were suffering from Asthma and 7.3% DR TB patients were suffering from Diabetes. DM patients are most vulnerable to develop TB & MDR TB. Also Asthma was a remarkable chronic disease among MDR TB. Some other study also had the similar findings [4]. Around 46% DR TB patients were addicted with smoking of Cigarette, Ganja, Tobacco and Alcohol. Some patients had addiction with single item and some had with multiple items. Studies in Russia showed alcohol abuse/dependence and smoking were associated with Drug Resistance. Several other studies also mentioned related findings [6-8]. Smoking was common for male and chewing Tobacco was common for female. Addictions with multiple items were also risk factor for developing MDR TB. MDR TB became more complicated if turns into XDR. XDR TB is an emerging threat to the world. In this study, we had learned about one XDR TB cases by performing culture & DST for 2nd line AT drugs. We should have established mechanism to detect XDR cases early and strong program to prevent development of XDR from MDR. This study presented us a clear view of socio-demographic status and epidemiological factors of registered MDR TB cases at Rajshahi and Rangpur divisions over the year 2013 & 2014. From the results, risk factors associated with MDR TB and elements for strategic planning can be identified.
7. Conclusions
- The study concluded that among the respondents, majority were within productive age group (16-45 years). Surveillance program need to conduct at Rangpur division to explain low MDR case detection in spite of high TB notification rate. Some important indicative risk factors for developing DR TB were identified such as education, low income, previous history, addiction, contact history, existence of XDR TB etc. It also urges to establish strong mechanism for early diagnosis and effective management of DR TB. The study put emphasis on effective contact tracings of the already detected DR TB patients, increase awareness of the patients and their family members regarding regularity of treatment and treatment under DOT. As the present study was confined only to MDR TB cases and there was no comparison group, definite conclusion regarding the factors responsible for developing MDR TB cannot be drawn. However, this study opens several scopes of further study and research on multiple issues. Based on the preliminary findings of this study, various social, behavioral and environmental aspects and their relationship with drug resistance TB can be better examined and analyzed. The study recommends that for early diagnosis of DR TB, National TB Control Program may develop policy for all new Smear Positive TB cases to be tested by GeneXpert during diagnosis as most of the cases are from Category – 1 treatment group. It can reduce treatment hazards and cost of treatment if DR TB treatment is provided from the beginning rather than a period of treatment under Category – 1 or Category – 2.
ACKNOWLEDGEMENTS
- We would like to extend our sincere gratitude to the authority of Rajshahi Chest Disease Hospital, Pabna Chest Disease Hospital and implementing partners of NTP at Rajshahi & Rangpur divisions for permitting me to conduct the study. We would also like to convey our gratefulness to all field staff members of partner organizations for their warm support to accomplish this study. We would also like to express our eternal thanks and appreciation to the respondents who were the source of information without which this research would not be possible.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML