-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2015; 5(6): 184-191
doi:10.5923/j.phr.20150506.03

Poor Birth Size a Badge of Low Birth Weight Accompanying Less Antenatal Care in Bangladesh with Substantial Divisional Variation: Evidence from BDHS - 2011
S. M. Raysul Haque , Shabareen Tisha, Nafisa Huq
School of Public Health, Independent University Bangladesh, Dhaka, Bangladesh
Correspondence to: S. M. Raysul Haque , School of Public Health, Independent University Bangladesh, Dhaka, Bangladesh.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In spite of having a pretty good progress in maternal and child health, low birth weight is still a serious public health issue for Bangladesh. The prime concern of this study was to crosscheck the eventual influence of antenatal care on poor birth size, a substitution of low birth weight and to explore the divisional variation along with its individual role on poor birth size. A nationally representative data, Bangladesh Demographic and Health Survey (BDHS) 2011 was used for this purpose. Sample size for this study was 7324 children from the different parts of the country born within last five years preceding the survey and all of them were the last child. Logistic regression analysis was applied to examine the influence of ANC on poor birth size as well as other relevant variables such as mother’s level of education, house hold income, division, age of mother at birth, birth order, sex of child, place of residence, media exposure etc. A total of 17.5% children had poor birth size (reported as “very small” or “smaller than average” by mothers) at the time of birth. The result of the analysis shows that ANC is negatively and significantly associated with poor birth size after controlling for all other potential factors. Four or more times ANC visited mothers, compared to no ANC visited mothers, have 26% lower risks of having poor birth size babies (p=0.002). Highest frequency (23%) of poor birth size was found at South-eastern part of Bangladesh which is Chittagong division and lowest frequency (10.1%) was observed in both Barisal and Khulna division. In comparison to Dhaka division, mothers living at Sylhet or Chittagong division have 42% or 35% higher risk of having poor birth size babies respectively(p=0.003 or p=0.001). As per current study it is well documented that provision of adequate antenatal care and proper utilization of it can effectively reduce poor birth size, eventually low birth weight in Bangladesh and divisional variation is also prominent in Bangladesh.
Keywords: Antenatal care, Poor birth size, Low birth weight, BDHS, Bangladesh
Cite this paper: S. M. Raysul Haque , Shabareen Tisha, Nafisa Huq , Poor Birth Size a Badge of Low Birth Weight Accompanying Less Antenatal Care in Bangladesh with Substantial Divisional Variation: Evidence from BDHS - 2011, Public Health Research, Vol. 5 No. 6, 2015, pp. 184-191. doi: 10.5923/j.phr.20150506.03.
Article Outline
1. Introduction
- Within limited time and capacity, Bangladesh has achieved a considerable progress in maternal and child health [1]. We need a long term sustainable approach, as infant mortality rate is still 38 per 1,000 live births [2]. Poor birth size which is a suitable proxy for low birth weight is a vital risk factor for neonatal mortality, eventually infant mortality. Current research evidence shows that low birth weight increases the odds of neonatal deaths by 20-30 times and infant death by 3 times [3, 4]. In case of very low birth weight, mortality rate is significantly high. Regardless of the gestational age if the birth weight is less than 2500 gram it is usually treated as low birth weight [5, 6] and in majority cases poor birth size coincide with low birth weight. In this particular study we have used this poor birth size as a symbol of low birth weight. Poor birth size is used for those babies whose mother reported their birth size as “very small” or “smaller than average”. At present around the globe about 20 million babies born with low birth weight and the vast majority, 95.6% are from developing countries [7]. The Prevalence of low birth weight is around 15% in developing countries [5]. According to “National low birth weight Survey of Bangladesh-(2003-2004)” over one-third of infants (36%) of Bangladesh born with low birth weight [8] which is more than twice of that 15% threshold which clearly indicates its public health significance. Recent evidence shows unexpected high prevalence of low birth weight in Bangladesh. Selina Khatun has reported 23.2% of low birth weight out of 465 samples at a maternal and child health training institute in Dhaka in 2008 [9]. Bishal Dhar has reported 15.18% low birth weight out of 316 samples in a government maternity hospital in Dhaka in 2002 [10]. Another community-based longitudinal study shows that infants who died before 12 months, 73% among them were low birth weight babies [11].Poor birth size a substitute of low birth weight is not only a vital risk factor for infant mortality it also causes severe physical and mental impairment to the survivors for the rest of their lives. A series of physical illness like malnutrition, cerebral palsy, breathlessness, higher incidence of diseases and growth retardation is very common [6, 12, 13, 14]. When low birth weight infants are grown up they usually face plenty of mental health issues like cognitive immaturity, poor social adaptation in school and other locations [12, 15]. low birth weight is also linked with a tendency to higher rates of coronary heart diseases, hypertension, diabetes and other future chronic diseases [16, 17]. Eventually low birth weight increases the overall burden of diseases.Risk factors and the causes of Poor birth size a substitute of LBW are multifactorial, complicated and are different among countries or regions. In the developed countries, preterm delivery and intrauterine growth retardation is the main common cause of low birth weight [18], however, in the developing countries biological and socioeconomic causes are more common. According to literature review we can consider the following factors for low birth weight in Bangladesh such as maternal age (lower than 20 or higher than 30), maternal under nutrition, birth order, maternal health conditions like diabetes, hypertension & anemia, obstetric factors, socio-economic factors like house hold income, maternal education, household leadership, service related factors like antenatal care (Care for the expected mothers up to child birth) [7, 8, 9, 19, 20, 21, 22]. Upon considering all the factors of low birth weight we may say maternal health condition especially during pregnancy period is the key determinant and it is also related with biological, social and service related factors. Antenatal care is an effective and feasible way by which we can monitor the health condition of both mother and the baby. It can efficiently reduce the low birth weight or poor birth size prevalence [22, 23, 24, 25]. So ANC with a link to low birth weight is not a new area to be discovered as WHO recommended 4 antenatal visits for a woman with normal pregnancy for a better pregnancy outcome [26]. In our country like the different parts of the globe, many studies have also been conducted so far targeting the same issue but majority of them was not representative for the entire country as some of them was done in urban areas, sample size was relatively small, lack of socio-demographic factors or based on clinical practice [7, 9, 10, 11]. An exploration on the current version of main national databases that can represent the whole country have not yet been done to oversee the linkage between ANC and low birth weight in Bangladesh. One of the major causes could be absence of the direct birth weight data in national representative health survey like BDHS (Bangladesh Demographic and Health Surveys), conducted every five years. In BDHS, direct measurement of birth weight is not available, because birth weight was not likely to be known for many babies, particularly for those born at home and in Bangladesh the majority of births occur at home. Data on birth size is available and even though subjective, this birth size is highly related with birth weight [27], so poor birth size could be a useful proxy for LBW. Another interesting finding regarding poor birth size in Bangladesh is regional or divisional variation. According to BDHS-2011, among the divisions (Bangladesh is divided into seven major administrative regions called division-2011), the highest percentage of very small children is seen in Chittagong and Sylhet (7%) though these two divisions are economically much more stable than others and the lowest (3%) is in Rangpur division [28]. So it is clear that region plays a vital role either independently or via other potential determinants. So, the aim of this study is to identify the independent effect of each of the factors of LBW with an eye to our key independent variable ANC and also to explore the divisional differences with a view to decrease poor birth size, eventually LBW prevalence in Bangladesh.
2. Research Hypothesis
- The hypothesis considered in this study is stated as “Less antenatal care (ANC) can increase poor birth size prevalence in Bangladesh eventually low birth weight prevalence”. It is not a new one but the interesting thing is here we are using birth size as a proxy for birth weight in a nationally representative dataset and want to observe whether it supports the mentioned hypothesis or not.
3. Data and Method
- The present study uses the data from Bangladesh Demographic and Health Survey (BDHS) 2011, conducted under the authority of the National Institute of Population Research and Training (NIPORT) of the Ministry of Health and Family Welfare and implemented by Mitra and Associates of Dhaka. ICF International provided financial and technical assistance for the survey through USAID/Bangladesh. The BDHS is part of the worldwide Demographic and Health Surveys program, which is designed to collect data on fertility, family planning, and maternal and child health. BDHS-2011 covered a nationally representative sample of 18,222 ever married women of age 12– 49 years and their children born 0–59 months prior to the survey date. It is the sixth national demographic and health survey. As a sampling frame BDHS used the list of enumeration areas (EAs) prepared for the 2011 Population and Housing Census, provided by the Bangladesh Bureau of Statistics (BBS). So the primary sampling unit (PSU) for the survey is an EA. The survey is based on a two-stage stratified sample of households. In the first stage, 600 EAs were selected with probability proportional to the EA size, with 207 clusters in urban areas and 393 in rural areas. In the second stage of sampling, a systematic sample of 30 households on average were selected per EA. Using this design; the survey selected 17,964 residential households of seven divisions of Bangladesh and 17,511 were found to be occupied. Within those households out of 18222 ever-married women 17842 were interviewed, yielding a response rate of 98 percent. In order to reduce the recall bias in the BDHS survey, information regarding Antenatal care (ANC), Post natal care (PNC), immunization, diseases etc. were asked only for the children of age less than 60 months. Therefore, a file was created for the sample of children of age 0–59 months including all variables of household and mother. In order to make it more precise and further reduce the recall bias, the data of last child (last life birth) were taken and the number was 7324 out of total 16025 births. Here we have considered twelve variables out of which one is dependent variable and other eleven are independent variables. Poor birth size is our dependent variable, outcome either poor birth size or not. In BDHS, direct measurement of birth weight is mostly not available, because birth weight was not likely to be known for many babies, particularly for those born at home. Therefore instead of direct measurement of birth weight, we have adopted the mother’s estimate of the baby’s size from the BDHS 2011. A mother’s report of a child being “very small”, “smaller than average”, “average or larger” in size, even though subjective, is highly related with birth weight and considered a useful proxy for low birth weight. So, here we have considered “very small” and “smaller than average” as poor birth size and “average or larger” as normal birth size. The key independent variable is the number of ANC (antenatal care) visit. Here we have categorized ANC visits into 3 groups: Never ANC visit group, 1 to 3 ANC visit group and 4 or more ANC visit group. Other independent variables are Age of mother at birth: three age groups are less than 20 years, 20 – 29 years and 30 years or above; Birth order: the categories of birth orders are first birth, 2nd to 3rd birth group and 4th or more birth group; Sex of the child: male or female; Mother’s body mass index (BMI): categories of BMI are less than 18.5 and 18.5 or more [29] and in BDHS BMI of mother was measured at survey time; Place of residence: as urban or rural; Exposure to media: as exposed or non-exposed; Belong to NGO as an proxy for sort of empowerment and also financial involvement; Region or Division: 7 divisions- Barisal, Chittagong, Dhaka, Khulna, Rajshahi, Rangpur and Sylhet; Maternal education: four levels of education, no education, primary education, secondary education and higher education group; Economic status: here we have used 3 categories for household economic status; poor, middle income group and rich.The analysis was done into multiple steps. Firstly, a univariate analysis was done for both dependent and independent variables. Then, bivariate analysis was done by the Chi-square test to examine the association between the dependent variable and all other independent variables separately. Finally, multivariate analysis was done by fitting the logistic regression model for LBW to examine the impact of ANC visit after controlling the other potential factors. This was done by following a step-by-step procedure and we have included the factors in the logistic regression model those are found to be statistically significant in the bivariate analysis (p<0.05). In first step, we have considered ANC as 1-3 visits and 4 or more visit in reference with no ANC visit and division as Barisal, Chittagong, Khulna, Rajshahi, Rangpur and Sylhe in reference with Dhaka for poor birth size. In second step along with ANC visit and division, we have also considered birth order as 1st birth and 4th or more birth in reference to 2nd - 3rd birth, sex of the child, mother’s level of education as primary, secondary and higher with the reference of no education, house hold income as poor and rich in reference with middle income and BMI of mothers.
4. Results
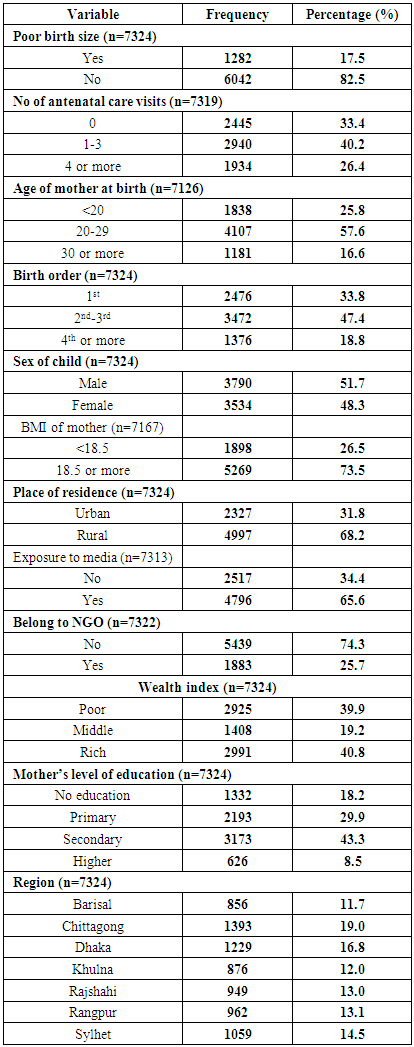
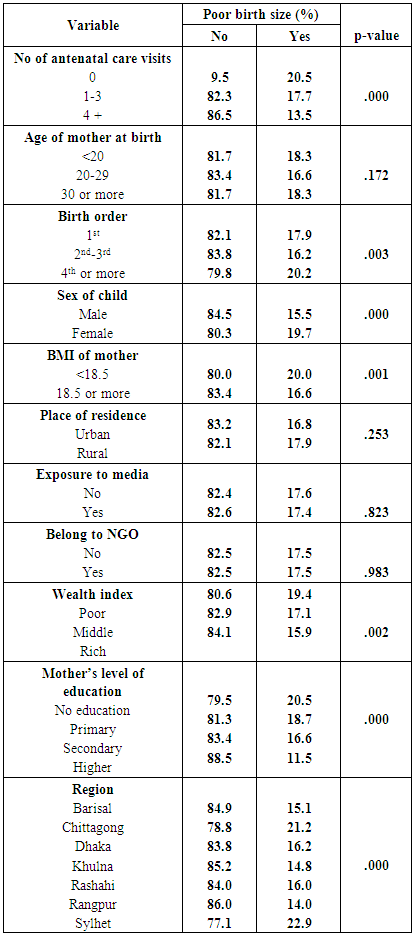
- Table 1 describes the profile of both dependent and independent variables. In case of dependent variable poor birth size out of 7324 cases 17.5% was poor birth size while 82.5% were not. Among the independent variables, our main point of interest is number of ANC visits. Within ANC visits 33.4% of mothers haven’t reported ever ANC visits while 40.2% of mothers have received from one to three ANC visits and the rest 26.4% of mothers have received 4 or more ANC visits. Regarding age of mother at birth, 57.6% of mothers were in-between 20 to 29 years and 25.8% were below 20 years while 16.6% were 30 years or above. Within Birth order, the 1stbirth group consists of 33.8%, the 2nd to 3rd birth group consists of 47.4% while 18.8% are in the 4th and more birth groups. Male sex ratio which is 51.7% is slightly higher than the female sex ratio that is 48.3%. Body mass index (BMI) of mother has categorized into the two groups; one, BMI <18.5, and the other, BMI >=18.5. BMI <18.5 represents lower BMI group which is 26.5%, on the other hand normal or higher BMI group consists of 73.5% mother. Among the respondents, 68.2% people reside in rural area while 31.8% reside in urban area. Respondents in exposure with media are 65.6% while 34.4% are not in exposure with media. In case of involvement with NGOs, only 25.7% mothers belong to NGO while 74.3% don’t. In case of wealth index, 40.8% are rich, 39.9% are poor and 19.2% are in middle class group. Within Mother’s level of education, 18.2% are in no education group, 29.9% are in primary education group, 43.3% are in secondary education group, while higher education group consists of 8.5%. Here we have considered 7 divisions named Barisal (11.7%), Chittagong (19.0%), Dhaka (16.8%), Khulna (12.0%), Rajshahi (13.0%), Rangpur (13.1%) and Sylhet (14.5%) which contain certain amount of our study population mentioned along with their names.
|
|
|
|
5. Discussion
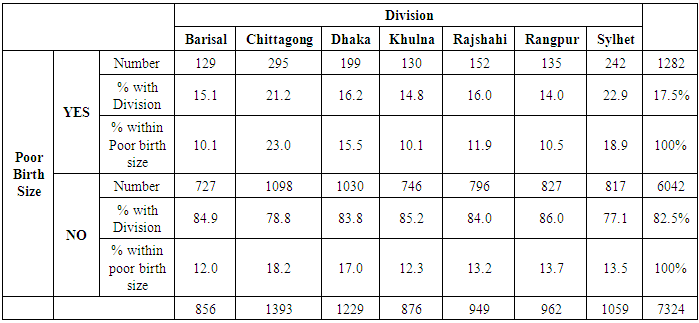
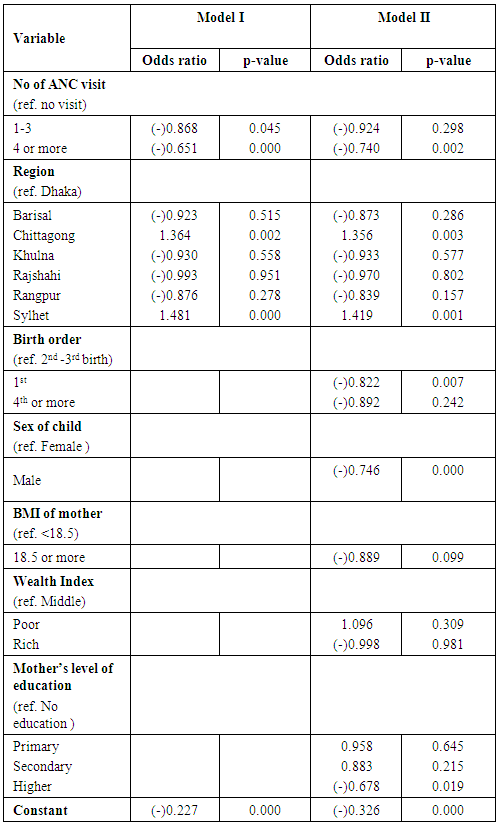
- It is very difficult to concentrate on a single factor and focus that as a predictor for poor birth size eventually low birth weight, especially in a developing country like Bangladesh, but definitely ANC is such a factor that can explain poor birth size from different perspectives. This is an attempt, which reports the factors linked with poor birth size based on the national level data which represent the whole country. One of the interesting as well as significant finding of this particular study is, 4 or more times ANC visited mothers have 26% lower risk of having poor birth size babies in comparison to no ANC visited mothers but we didn’t find any significant finding regarding poor birth size in case of one to three ANC visited mothers compared to no ANC visited mothers. One of our recommendation is at least 4 ANC is needed to get a desired outcome regarding poor birth size. One fourth of the poor birth size can easily be prevented by ensuring 4 or more ANC visit. Other modifiable risk factors that predict poor birth size could also be facilitated by ANC, focusing the general health condition of the mothers including nutritional support, weight gain during pregnancy, anemia control and further follow-up checkups. This study shows 4 or more times ANC visit is negatively associated with LBW which is also supported by other studies [7, 31] except one [18], although in that particular study they consider <6 ANC visit and ≥6 ANC visit and pointing towards the quality of ANC. So in policy level implication in Bangladesh, our focus should be at least 4 or more ANC provision during pregnancy period. In our study we have found that the prevalence of poor birth size eventually low birth weight is 17.5% which differs from other studies in Bangladesh as they have found 23.2% [30] or 24% [18] or even more, important reasons could be less sample size (350 and 583 respectively), place of the study (Central part of Dhaka and different villages of Nabinagar under Savar Upazila respectively) or time period of the study (2003 to 2005 and 2000 to 2001 respectively). Another interesting finding of this study is the divisional variation regarding poor birth size in Bangladesh. Northeastern (Sylhet) and south-eastern (Chittagong) part of Bangladesh is denoted as a higher risk zone for poor birth size. The highest prevalence of poor birth size was found in the port city Chittagong which is 23% and second to it was Sylhet (18.9%). The lowest prevalence of poor birth size was observed in both Barisal and Khulna division which is 10.1%. Overall scenario in aspect of provision and access to health care system, human resources and development of Dhaka division, the capital of Bangladesh is far better than Barisal and Khulna division. Despite of this, frequency of poor birth size is higher in Dhaka (15.5%) than Barisal or Khulna division. Division plays a vital role in determining poor birth size even after controlling all other potential factors. Mothers living in the Sylhet division have 42% higher risk of having poor birth size babies compared to mothers living at Dhaka division. Similar finding is also observed for mothers living at Chittagong division, they have 35% higher risk of having poor birth size babies compared to mothers living at Dhaka. This divisional inconsistency direct towards a strange scenario. Both Chittagong and Sylhet are economically stable divisions of Bangladesh but we did not find any significant effect of house hold income on poor birth size in this particular study after controlling with other factors. Most likely explanation could be both of these Chittagong and Sylhet have difficult topography with hilly areas and population distributions versus basic facilities are not uniform throughout the division. Poor transportations system, distance between the community and health care provider, social norms and culture, poor status of women empowerment and less employment opportunity; all of these could collectively affect maternal health during pregnancy and one of the outcome would be poor birth size. Quality of health care system including ANC could be a vital cause for this divisional variation but we didn’t consider the quality due to lack of information. Without any doubt these findings leads us to further research pointing divisional difference on poor birth size in Bangladesh. Another modifiable key factor to reduce poor birth size in this study is mother’s education. Mother’s level of education has a significant influence on the poor birth size of child. The finding of present study also comply with previous studies that incidence of poor birth size decreases as mother’s education level increases [9, 32]. This study also shows that there is a gradual decrease of the frequency of poor birth size as education level increases from no education to higher education. So with a view to decrease poor birth size the education level of this country should be raised with a special attention to create opportunities for mother’s education. Community and religious leaders should be encouraged to advocate in favor of maternal education and the awareness. In this particular study no statistical significance was observed between maternal age at birth and poor birth size which is also supported by few studies in terms of low birth weight [33, 34, 35 ] and also disagreed by other studies [7, 31, 32]. In case of place of residence, we did not find any significant association with poor birth size. One possible explanation could be, health care facilities are much more available in rural areas in comparison to previous years and there is no such big difference in urban and rural areas in aspect of facility provision. Another interesting finding is we did not observe any significant effect of house hold income on poor birth size. In line of this finding we can say, due to both governmental and non-governmental efforts money is not the prime factor to have health facilities as it was in previous ages. We also did not find any statistically significant effect of mother’s BMI on poor birth size. An acceptable explanation could be, this BMI of mother was measured at survey time. We found a significant effect of birth order and sex of the child on poor birth size as less poor birth size is seen in first birth group compared to 2nd -3rd birth group and in male child compared to female child.The focal limitation of this study is to use baby’s birth size as a substitute of direct measurement of birth weight as birth weight data is not available in BDHS 2011 and this birth size is also taken from the mothers assumption on the other hand however we can say that the baby’s birth size is a suitable proxy for birth weight as other findings of this study match with several finding of other studies in Bangladesh that used birth weight. Furthermore, because of lack of data, we could not evaluate quality of antenatal care visits, but only the number of ANC visits. As the data is not longitudinal in nature, we could not draw a causal implication and also due to recall bias, there is a possibility of under estimation of poor birth size eventually low birth weight.
6. Conclusions
- Using a nationally representative data set, it is verified that antenatal care can significantly reduce the poor birth size eventually LBW prevalence in a developing country like Bangladesh. Ensured provision of 4 or more ANC visit would be an effective public health measure to combat poor birth size in our country. There must be other hidden factors regarding poor birth size that led the substantial divisional difference which need to be evaluated by further mixed method research (both qualitative & quantitative) as we haven’t found much evidence.
ACKNOWLEDGEMENTS
- We would like to thank Dr. M. Omar Rahman, Vice Chancellor and Dean School of Public Health, Independent University Bangladesh and Dr. Wasimul Bari, Professor, Department of Statistics, Biostatistics and Informatics, University of Dhaka for their endless encouragement and kind support regarding this study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML