Oscar O. Apondi , Dennis M. Njenga, Duke O. Nyakundi
Department of Mathematics, Masinde Muliro University of Science and Technology, Kakamega, Kenya
Correspondence to: Oscar O. Apondi , Department of Mathematics, Masinde Muliro University of Science and Technology, Kakamega, Kenya.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
Abstract
Objectives: The study aimed to determine the knowledge, awareness and access of existing health care facilities and prevention services amongst the people infected with HIV and also to find out the knowledge and level of awareness of HIV related illnesses amongst people infected with HIV. Methods: The data used for analysis in this research project is got from Kenya Indicator Survey (KAIS 2012) in which a sample of 13,720 total adults were interviewed out of the target sample size of 23,896 for women and men aged 15 to 64 years. The remaining 10,176 of the sample was dropped mainly because the sampling frame for the North Eastern region was not available at the time of survey. Data Analysis: The data was analysed using STATA-software version 13, and report presented in form of tables and graphs. Results: This project found out that majority of people infected with HIV and AIDs are not aware of the importance of sleeping under mosquito net, taking daily nutritional supplements and treating water as preventive measures against opportunistic diseases. Conclusion: The results revealed that there was little knowledge, awareness and access of existing health care facilities and prevention services amongst people infected with HIV. Moreover, It was also found out that there is high knowledge and level of awareness of HIV related illnesses amongst people infected with HIV especially TB.
Keywords:
Health care utilization, Kenya, KAIS, AIDS related illness
Cite this paper: Oscar O. Apondi , Dennis M. Njenga, Duke O. Nyakundi , Health Care Utilization and Preventive Services among HIV-Infected People in Kenya, Public Health Research, Vol. 5 No. 4, 2015, pp. 120-128. doi: 10.5923/j.phr.20150504.06.
1. Introduction
HIV stands for Human Immunodeficiency Virus, and is the virus that causes AIDS. HIV destroys certain blood cells that are crucial to the normal functioning of the immune system, which defends the body against illness. [1]AIDS stands for Acquired Immunodeficiency Syndrome. It occurs when the immune system is weakened by HIV to the point where a person is susceptible to any number of Opportunistic Infections (OIs) or diseases. Having AIDS is defined as presenting with HIV and one or more OIs. Opportunistic infections (OIs) are illnesses caused by organisms that do not usually cause disease in persons with healthy, functioning immune systems. [1].Kenya is the fourth-largest HIV epidemic in the world. In 2012, an estimated 1.6 million people were living with HIV, and roughly 57,000 people died from AIDS-related illnesses. [2]. Since 2003, annual AIDS related deaths have declined from approximately 167,000 to 58,465 in 2013. [3]. Tuberculosis (TB) is an infectious bacterial disease caused by Mycobacterium tuberculosis, which commonly affect the lungs. [4]. The (TB) epidemic in Kenya has been fuelled by the concurrent HIV epidemic. TB is one of the leading causes of mortality among people with HIV, and, conversely, HIV infection is a risk factor for active TB. Despite the majority of HIV-infected persons with a prior TB diagnosis, (61.1% with any TB diagnosis and 56.8% with a recent TB diagnosis) were aware of their HIV infection there is still, 11.1% who had never had a diagnosis of TB. [5].Chronic diarrhoea is a leading killer of people infected with HIV. Contaminated water is often the source of microbes that cause diarrhoea. Treating water to make it safe for drinking dramatically improves the health of all people, particularly those with HIV infection who may have a weaker immune response to fight against simple waterborne infections. Overall, 54.5% of HIV-infected persons lived in a household that did not treat its main source of drinking water. [5]. Malaria-related illness can also be fatal for immune-compromised individuals; the Government Of Kenya (GOK) has adopted malaria prevention as a key aspect of basic care for HIV-infected children, adolescents and adults. Eight out of 10 HIV-infected adults are not sleeping under treated bed nets and therefore vulnerable to potentially malaria infection through mosquito bites. The above low number may be due to lack of access and knowledge. [5]. The number of people with insecticide-treated nets (ITNs) is still low with 59 percent of households in Kenya own at least one ITN and 34 percent own at least one ITN for every two persons who stayed in the household the night preceding the survey (Kenya Demographic and Health Survey). [6].Nutritional supplements and multi-vitamins have been proposed as a method of providing caloric and micronutrient support for HIV-infected people in resource-limited countries. Studies suggest that people with HIV benefit from receiving nutritional and multivitamin supplements, as these may reduce morbidity and delay progression to advanced stages of disease. In Kenya, among HIV-infected adults who knew they were infected with HIV, only 7.3% reported taking one or more daily caloric supplements and only 4.6% reported taking immune boosters. The most common supplement taken was a daily multivitamin; 36.4% of HIV-infected persons who knew they were infected reported taking multivitamins on a daily basis. [5]. Daily use of cotrimoxazole (trimethoprim- sulfamethoxazole) or Septrin® prevents certain bacterial and parasitic infections that cause pneumonia, diarrhoea and malaria and prolongs the lives of adults and children who have HIV [5]. In Kenya, 12.1% of HIV-infected adults were taking cotrimoxazole or Septrin daily to prevent infections; an estimated 1.25 million HIV-infected people were in need of Cotrimoxazole. Use of CTX among those aware of their HIV infection was high at 89%. This was an increase from 2007, where CTX use was 76% among HIV-infected persons who were aware of their HIV infection. Overall, 40.5% of antiretroviral (ARV)-eligible adults were taking ARVs. At the time of the survey, an estimated 214,000 people were eligible for daily ARVs but not taking any. Among those who knew they were infected with HIV, access to care and treatment was high: 76.1% were taking cotrimoxazole daily, and 91.6% of ARV-eligible adults were taking ARVs. [7]. Problem statementIn Kenya roughly 57,000 people died from AIDS-related illnesses in the year 2012. [2]. Most people living with HIV or at risk for HIV DO NOT have access to prevention, care, and treatment, and there is still no cure. [8]. In 2012 KAIS, among all HIV-infected persons aged 15 to 64 years who were aware of their infection and eligible for ART, 88% were on antiretroviral (ART) meaning 12% are still not on ART. [7]. Moreover, In 2007 KAIS, 9.7% or 138,000 individuals of the estimated 1.42 million HIV-infected adults were taking ARVs nationwide. The remaining 1.28 million HIV-infected adults were not taking ARVs; however, not all were eligible. [5].There are a number of reasons why HIV-infected adults may not take daily cotrimoxazole or why eligible HIV-infected adults may not take daily ARVs; some may relate to the health care system or individual behaviours. Many have never been tested for HIV and are therefore not aware of their HIV status, which is a significant barrier. Among those aware, some adults may not take cotrimoxazole or ARVs because they lack knowledge on appropriate use or may be unwilling to take medications because they feel healthy or because they suffered from adverse side effects from medications. Additionally, while these medications should be available to those who need them, wait times at health centres and transport cost to facilities may prevent enrolment of HIV-infected adults in care and treatment. [5].Tuberculosis (T.B.) i.e. OIs remains the leading cause of death for people living with HIV. [9]. In 2011, it was estimated that 79 percent of TB and HIV co-infection occurs in sub-Saharan Africa. TB is estimated to cause one out of 4 AIDS-related deaths. Approximately 430 000 people died of HIV-associated TB. A majority of these deaths occur in Africa, where the mortality rate from HIV-related TB is more than 20 times higher than in other world regions. [5].Chronic diarrhoea is a leading killer of people infected with HIV. Contaminated water is often the source of microbes that cause diarrhoea. In Kenya, Overall, 54.5% of HIV-infected persons lived in a household that did not treat its main source of drinking water. [5]. Salmonellosis bacterial infection from contaminated food or water is another common infection to people who are HIV-positive. [10].Around the world, 3.2 billion people are at risk of contracting malaria. In 2013, an estimated 198 million cases occurred, and the disease killed approximately 584,000 people-mostly children under age five in Africa. On average it kills a child every minute. [11]. Malaria-related illness can also be fatal for immune-compromised individuals; the Government Of Kenya (GOK) has adopted malaria prevention as a key aspect of basic care for HIV-infected children, adolescents and adults. Eight out of 10 HIV-infected adults are not sleeping under treated bed nets and therefore vulnerable to potentially malaria infection through mosquito bites. [5]. Nutritional supplements and multi-vitamins have been proposed as a method of providing caloric and micronutrient support for HIV-infected people in resource-limited countries though there is still low percentage (as indicated in KAIS 2007 report) of people using them. This may be attributed due to lack of knowledge and access. [5].Daily cotrimoxazole(CTX) and treatment with antiretroviral (ARV) medication, along with other HIV specific care, prevent illnesses and diseases and dramatically prolong the lives of people with HIV. [5]. Objective of the Study1. To find out, knowledge, awareness and access of existing health care facilities and prevention services amongst the people infected with HIV.2. To find out the knowledge and level of awareness of HIV related illnesses amongst people infected with HIV.Research Questions1. Are people infected with HIV aware and have knowledge and access of proper health care facilities and prevention services?2. Do people infected with HIV know or aware of the HIV related illnesses?JustificationThe problem of getting access to health facilities has been the set back to reducing mortality; 1.6 million people have died of AIDS-related causes. [12] And in 2012, only 9.7 million people could access treatment [9]. HIV-infected adults may not take daily cotrimoxazole or eligible HIV-infected adults may not take daily ARVs; some may relate to the health care system, while others relate to individual behaviours. Among those aware, some adults may not take cotrimoxazole or ARVs because they lack knowledge on appropriate use or may be unwilling to take medications because they feel healthy.Overall, 54.5% of HIV-infected persons lived in a household that did not treat its main source of drinking water. [5].HIV-infected adults are not sleeping under treated bed nets and therefore vulnerable to potentially malaria infection though mosquito bites. This may be due to lack of access and knowledge. [5]. Hence this research paper will be very important in showing how lack of access, knowledge and unawareness to existing health facilities and lack of the use of preventive services may lead to accelerated mortality on people living with HIV. The results got here would be important in giving possible solutions of reducing mortality rates on people living with HIV. LimitationThe research paper will concentrate mainly on data from adult population (15-64 years) living out children who also die of HIV- related illnesses.
2. Literature Review
Since the start of the HIV epidemic an estimated 36 million people have died of AIDS related illnesses. [9]. The number of people dying of AIDS-related causes fell to 1.8 million [1.6 million–1.9 million] in 2010, down from a peak of 2.2 million [2.1 million–2.5 million] in the mid-2000s. A total of 2.5 million deaths have been averted in low- and middle-income countries since 1995 due to antiretroviral therapy being introduced, according to new calculations by UNAIDS. Much of that success has come in the past two years when rapid scale-up of access to treatment occurred; in 2010 alone, 700 000 AIDS-related deaths were averted. Almost half of the deaths from AIDS-related illnesses in 2010 occurred in southern Africa. AIDS has claimed at least one million lives annually in sub Saharan Africa since 1998. [13]. In 2010 regional estimates of Aids related deaths were 1.2 million in Sub-Saharan Africa, 35000 in Middle-East and North Africa and 250,000 in south and South-East Asia. [13].The part of the world most impacted by HIV, sub-Saharan Africa, has cut the number of people dying of AIDS-related causes by 32% between 2005 and 2011. The largest drop in AIDS-related deaths was in some of those countries where HIV has the strongest grip. In South Africa, 100 000 fewer deaths occurred, followed by nearly 90 000 in Zimbabwe, 71 000 in Kenya, 59 000 in Ethiopia and 48 000 in the United Republic of Tanzania. A number of the region’s countries with smaller populations but high HIV prevalence have also made significant gains in averting deaths related to AIDS. Botswana cut AIDS-related deaths by 71%, Rwanda by 68%, Namibia by 60%, Zambia by 56% and Burundi and Côte d’Ivoire by 51%. Benin, Burkina Faso, Eritrea, Guinea, Lesotho, Malawi and Mali all reduced AIDS-related deaths by one third. The countries of the Caribbean experienced a 48% decline in AIDS-related deaths while in Oceania the drop was 41%. [13] The high burden of HIV and AIDS in Kenya accounts for an estimated 29 percent of annual adult deaths, 20 percent of maternal mortality, and 15 percent of deaths of children under the age of five. The epidemic has also negatively affected the country’s economy by lowering per capita output by 4.1 percent. The approximate number of people dying of AIDS-related conditions in selected counties in Kenya include; Nairobi adults 3579 and children 448, Kisumu adults 2861 and children 1040, Narok adults 1341 and children 188, Kakamega adults 1605 and children 462, Bomet adults 1393 and children 195, Garissa adults 521 and children 69, Kilifi adults 1021 and children 179, Kiambu adults 1207 and children 180, Homabay adults 3395 and children 1234, Samburu adults 200 and children 50, [14].There were an estimated 9 million new cases of TB in 2013 (including 1.1 million cases among people with HIV) and estimated 1.5 million deaths (including 360,000 people with HIV), making this disease one of the world’s biggest infectious killers. [11]. Among People Living with HIV (PLHIV), TB is the most frequent serious opportunistic infection and a leading cause of death. HIV Infection increases the risk of TB-disease ten-fold; together with a higher risk of death, recurrence and re-infection. ART substantially decreases the risk of TB disease, but additional interventions are needed to reduce the risk burden of TB disease among PLHIV.Access to antiretroviral therapy in low–and middle income countries increased from 400 000 in 2003 to 6.65 million in 2010, 47% coverage of people eligible to treatment, resulting in substantial declines in the number of people dying from AIDS-related causes during the past decades. [15]. Lack of knowledge of serostatus (having or not having detectable antibodies against a specific antigen, measured by a blood test) by PLHIV is a major obstacle to realizing the goal of universal access to treatment and prevention. A significant proportion of PLHIV continue to present late for treatment because they are unaware that they are seropositive, including in high-income countries, thus reducing the effectiveness of ART on morbidity, survival and preventing HIV infection. In many circumstances, people informed of their HIV-positive status are not adequately linked with the appropriate services, thus preventing immediate enrolment in care. [1]. Studies suggest that people with HIV benefit from receiving nutritional and multivitamin supplements, as these may reduce morbidity and delay progression to advanced stages of disease. In Kenya, among HIV-infected adults who knew they were infected with HIV, only 7.3% reported taking one or more daily caloric supplements and only 4.6% reported taking immune boosters. The most common supplement taken was a daily multivitamin; 36.4% of HIV-infected persons who knew they were infected reported taking multivitamins on a daily basis. [5].The GOK recommends that in households affected by HIV, water from all sources, including piped systems, a public tap, dug wells, rainwater or surface water should be treated before drinking, with an exception only for bottled water. Drinking water treatment practices were collected at the household level, not at the individual level. [16].
3. Methodology
3.1. Study Population
The study was conducted in Kenya from October 2012 to February 2013. KAIS 2012 was a cross-sectional, population-based survey that sampled 9,300 households within nine of the 10 National AIDS and STI Control Programme (NASCOP) programmatic regions. These regions include urban and rural areas of Nairobi, Central, Coast, Eastern North, Eastern South, Nyanza, Upper Rift, Lower Rift, and Western regions. The sampling frame was not available for the North Eastern region at the time of the survey. The study concentrated to adults and adolescents aged 15 to 64 years. Adults of 15 years and above were interviewed. The study involved secondary analysis of data from the Kenya AIDS Indicator Survey (KAIS) conducted in Kenya in 2012. KAIS focuses on obtaining nationally representative estimates for HIV indicators which is critical for evaluating a country’s response to the HIV epidemic. This study will use descriptive analysis to draw conclusions from the KAIS 2012 data.
3.2. Sample Design
The survey used two stage stratified cluster sampling where the first stage selected 372 out of 1,800 clusters from the Kenya National Bureau of Statistics (KNBS) household-based sampling frame and the National Sample Survey and Evaluation Programme (NASSEP V). [17]. Using probability proportional to size (PPS) method. The second stage randomly selected a sample of 25 households in each cluster from a roster of households in the cluster using systematic random sampling. The sample size was calculated to provide representative national, regional, urban and rural estimates of HIV infection among adults and adolescents aged 15 to 64 years. The target sample size was 23,896 for women and men aged 15 to 64 years and 8,226 for children aged 18 months to14 years. Variable under considerationThe main response variables were the level of awareness, Knowledge and access to proper healthcare, healthcare facilities and preventive services amongst people living with HIV. In order to get the above variables, the respondents were asked the following questions; If they had ever been to TB clinic, if they slept under a treated net in the night before the survey, how they made water safe for drinking, if they have heard of ART that make people live longer, Have you seen a doctor health facility? If they had ever attended clinic or health centre, If they said yes they were again asked reasons for not visiting clinics, they were also asked if they were taking CTX or ART and if they were taking nutritional supplements, If not they were again asked the reason for not taking. Other response variable is the knowledge and level of awareness of HIV related illnesses amongst people living with HIV. The following questions were asked; if they ever heard of TB, they were also asked if TB could be cured in people living with HIV.The explanatory variables considered in this study are People living with HIV and age; ages between 15 to 64 years.Data AnalysisData from KAIS 2012 was analysed using STATA-software version 13 to draw the charts and graphics to show the effect of knowledge, awareness and access to healthcare facilities and preventive services and the knowledge and awareness of HIV related illnesses amongst people living with HIV. Descriptive analysis was used to illustrate the risk of lack of knowledge, awareness and access to healthcare facilities and preventive measures and the knowledge and awareness of HIV related illnesses amongst people living with HIV. Cross tabs and tables of knowledge, awareness and access to healthcare facilities and preventive measures and the knowledge and awareness of HIV related illnesses amongst people living with HIV was calculated and results of the frequencies shown below.
4. Results and Discussions
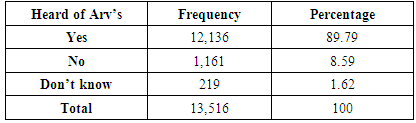
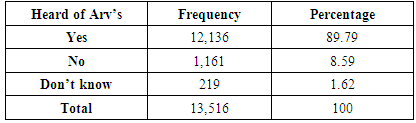
From the survey as indicated in table 1 above we found that approximately 89% were aware that ARVs could be used to people infected with HIV to improve their health. Despite the huge knowledge on existence of ARV and its importance there is still need to reach the remaining 8% and 1% who are not aware and do not know respectively.Table 1. The table below represents the knowledge about antiretroviral medication
 |
| |
|
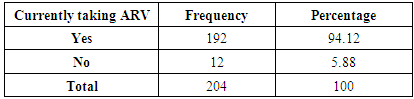
Table 2. The table below shows the number of people taking ARVs and those not taking
 |
| |
|
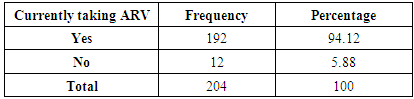
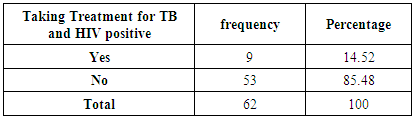
Table 2 above shows that approximately 94% of people infected with HIV reported that they were currently on ARV medication while on the contrary approximately 5% were not under medication which calls for more campaigns to increase knowledge and awareness on the importance of consistency in taking ARVs. Those not taking ARVs gave reasons as presented in figure 1 below.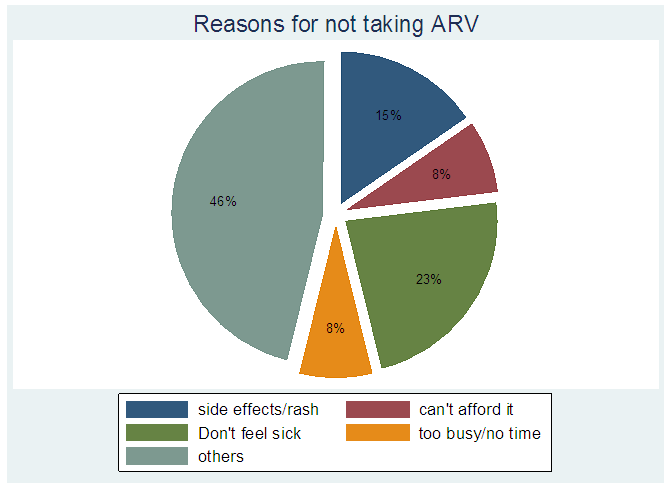 | Figure 1. The pie chart above represents reasons why people are not taking ARV medicines |
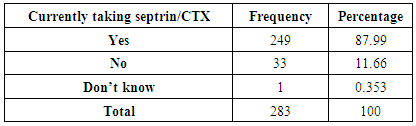
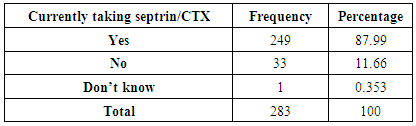
Clearly from the pie chart in figure 1 above 46% had other reasons for not taking ARVs. Interestingly 23% reported that they felt healthy hence no need for medication, this may be due to lack of proper knowledge on the importance of taking ARVs. It is also significantly evident that 8% of those having the virus cannot afford the medication thus need to put measures for easy access of the medication.Table 3. The table below shows the number of people taking CTX, those not taking and those who don’t know
 |
| |
|
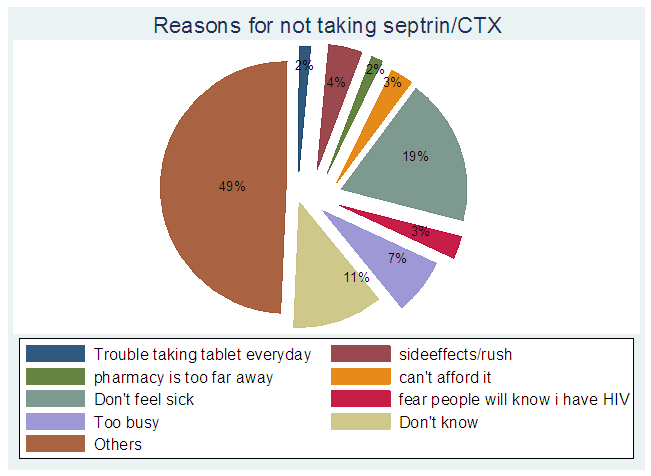
From the study, table 3 above depicts that approximately 88% of those people living with HIV are currently taking septrin/CTX while 33% of those people living with HIV are not taking the medication. This calls for sensitization on the importance of CTX and its use especially for those people living with the HIV virus.The 11% of those not taking septrin in table 3 above may be due to the reasons in figure 2 below. The pie chart in figure 2 below indicates that 19% felt that they were healthy hence did not see the need of taking medication. 2% indicated that the facilities were too far away while 3% said that they cannot afford the medication. Therefore there is a need to put up more facilities that can be centrally accessed by the people.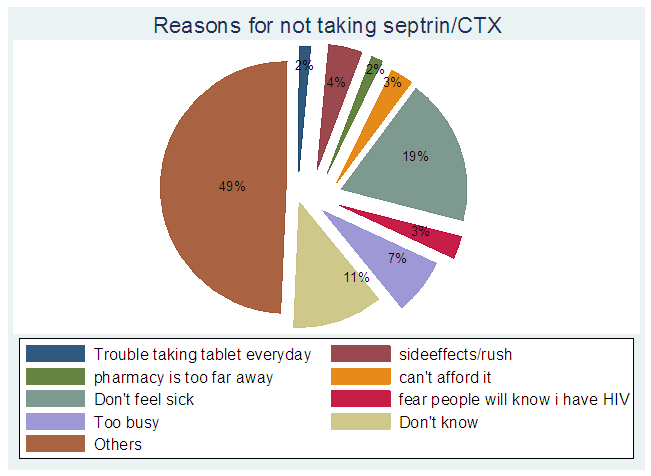 | Figure 2. The pie chart above represents reasons for not taking septrin or cotrimoxazole |
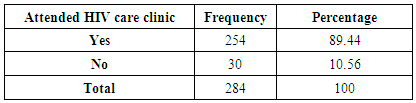
Table 4. The table below shows the number of people who attended HIV care clinic and those who did not attend
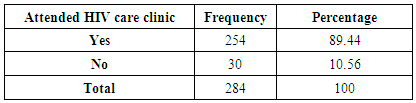 |
| |
|
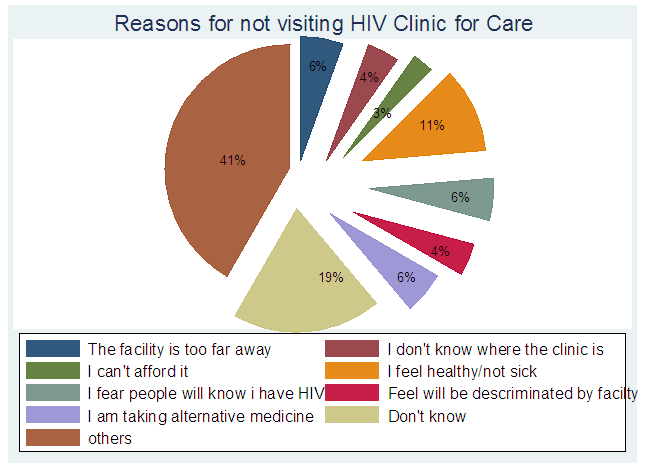
Table 4 above shows 254 of those infected a representative of approximately 89% attended HIV clinic while approximately 10% did not attend HIV clinic. This 10% not attending clinic is worrying and a lot still needs to be done to reduce the percentage. Those who did not attend clinic gave reasons for not attending as presented in figure 3 below.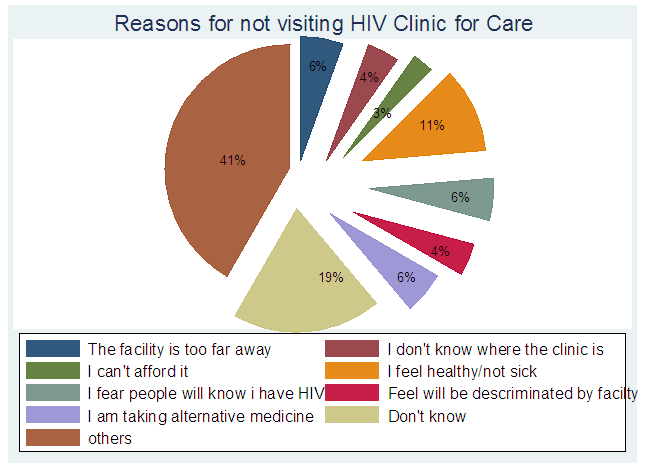 | Figure 3. The pie chart above represents the reasons for not visiting health clinic |
From figure 3 above we observe that 4% did not know where the clinic facility was, this implies that they did not have knowledge of health facilities. Some 6% as indicated in the above figure 3 showed that the facility was too far away meaning they did not have easy access to the health facilities while 3% could not afford services of the facilities. Table 5. Table showing people infected by HIV sleeping and not sleeping under mosquito net
 |
| |
|
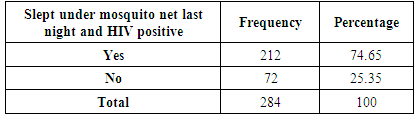
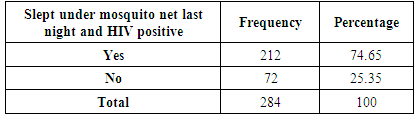
The study showed that out of people infected with HIV approximately 74% slept under a mosquito net. Approximately 25% indicated that they did not sleep under a mosquito net. This is clearly presented in table 5 above thus a need to increase urgency especially for those infected with HIV so as to boost their immune system by reducing chances of getting opportunistic diseases like malaria which is got from mosquito bites.Table 6. The table below shows the knowledge of Tuberculosis in people living with HIV
 |
| |
|
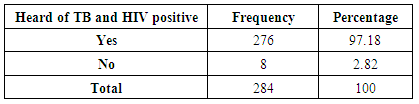
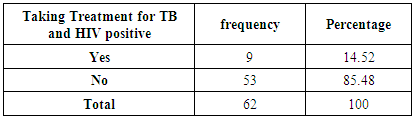
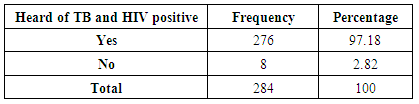
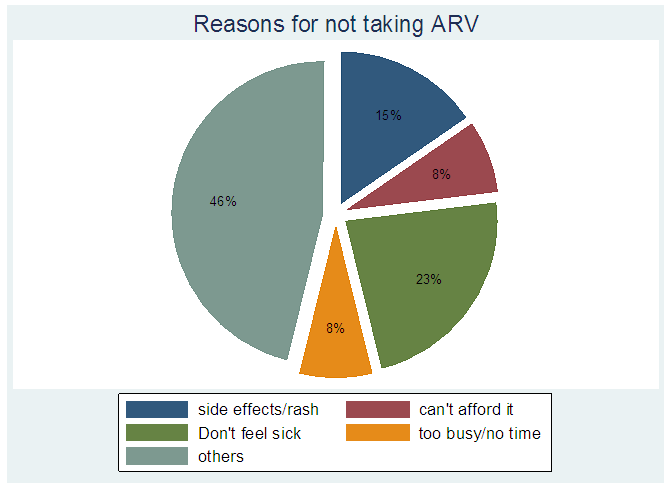
A large percentage (97%) of people infected with HIV virus are aware of tuberculosis which is one of the opportunistic diseases while approximately 2% are still on the dark side about the knowledge of such opportunistic diseases as indicated in table 6 above.Table 7 reports that even though a large percentage of people infected with HIV have knowledge on TB only 14% go for treatment. This is worrying since a large percentage, 85% do not go for treatment of TB hence a need for campaign on the advantage of getting treatment for TB especially for those infected with the HIV virus which may in turn reduce the mortality caused by TB among other HIV related illnesses. Table 7. The table below shows the number of people taking TB treatment and are HIV positive
 |
| |
|
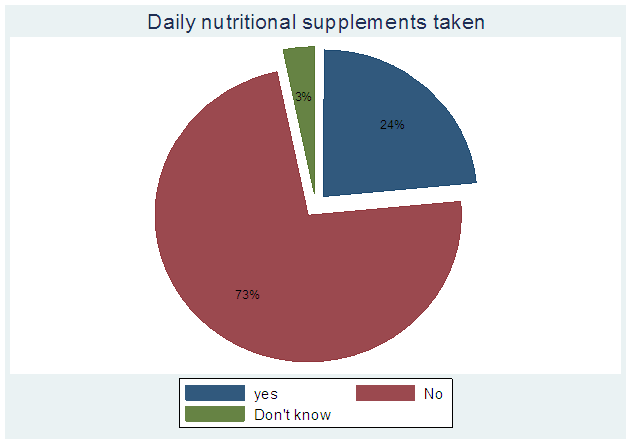
From the above graph of figure 4 a large percentage, 73% of people infected with HIV indicated that they are not taking daily nutritional supplements which are believed to help increase the body immune system. Only 24% are reported to be taking daily nutritional supplements. This large percentage of people not taking daily nutritional supplements attributes the continued increase in opportunistic diseases resulting from the weak immune system. 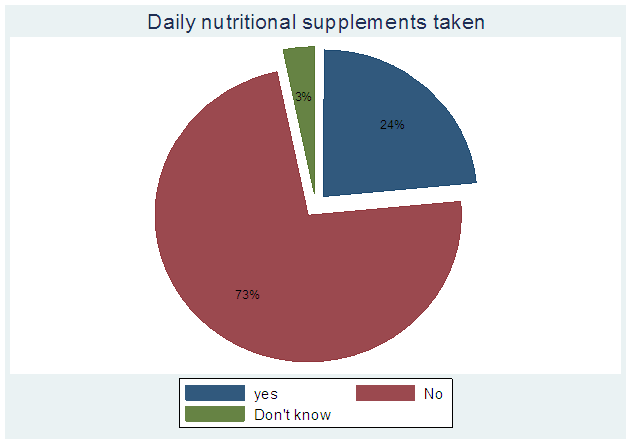 | Figure 4. The pie chart above represents the number of People taking daily nutritional supplements |
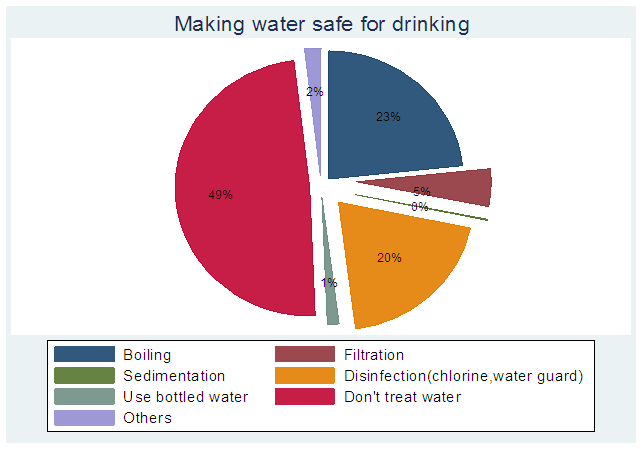
The study revealed in figure 5 that a large percentage, 49% of people infected with HIV do not treat their drinking water and thus increasing their chances of getting Chronic diarrhoea which is one of the HIV related opportunistic diseases resulting from weak immune system. This calls for sensitization on the importance of treating drinking water to help boost immune system especially for those infected with HIV virus.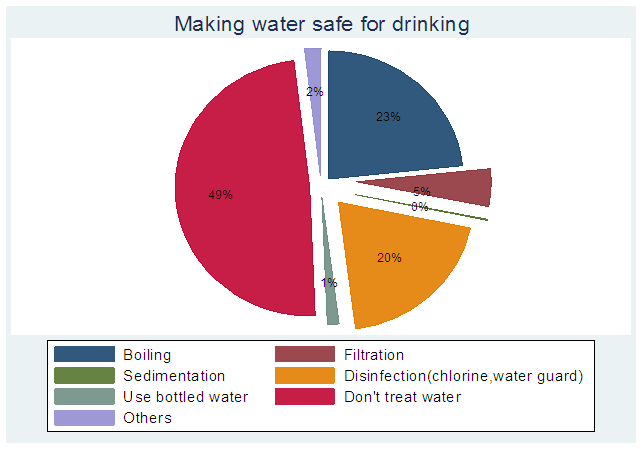 | Figure 5. The pie chart above shows the ways households make water safe for drinking |
5. Conclusions
The objectives for the study were met, since the study revealed little knowledge, awareness and access of existing health care facilities and prevention services amongst people infected with HIV.Majority of people infected with HIV and AIDs are not aware of the importance of sleeping under mosquito net i.e. approximately 25% indicated that they did not sleep under mosquito net. It was also found out that there is high knowledge and level of awareness, approximately 97% of HIV related illnesses amongst people infected with HIV, though there was little awareness i.e. approximately 10% on the importance of attending clinics; a case study of TB clinics.Similarly a large percentage, 49% do not treat their drinking water hence increasing their chance of getting chronic diarrhoea; an opportunistic disease. A large percentage(72%) were seen not to be taking nutritional supplements thus further weakening their immune system and herby increasing chances of OIs. The results from this study is therefore significant in that it will help the GOK and the health sector to concentrate on areas that need much improvement such as the high number of HIV infected individuals with TB not attending clinic, not sleeping under treated mosquito net, not taking daily nutritional supplements and those not making their water safe for drinking. Improvement on the above will help people infected with HIV and AIDs live a healthy life and therefore this will in turn reduce the mortality rate of people infected with HIV and AIDs.The future research needs to capture data on children as they too suffer from HIV and HIV related illnesses. There is also a need to evaluate and analyse “Others” as other reasons for HIV infected people; not taking ARV, not attending HIV clinics for care, not taking septrin/CTX so as to come up with better results to help improve their lives to reduce mortality rate due to HIV-related illnesses.There is also a need to investigate why a larger percentage of people infected with HIV and have TB are not taking treatment yet it is one of the major OI causing great mortality amongst people leaving with HIV.
6. Recommendations
i. Campaign and sensitization about the importance and ways of making water safe for drinking to avoid infection with diseases like chronic diarrhoea.ii. Create awareness on the different types of affordable nutritional supplements to people infected with HIV to help them boost their immune system. iii. VCTs should also incorporate test of opportunistic diseases like TB, Chronic diarrhoea and malaria for those tested positive with HIV virus.iv. Make awareness on the proper and consistent taking of medication like CTX and ARVs.v. Health facilities should be made easily accessible and affordable especially for those people infected with HIV.vi. The awareness campaigns about healthcare and preventive services should be extended to social media in order to reach a larger population especially the youth.
References
| [1] | Global Fact sheet, “AIDS 2014,” in 20TH International AIDS conference, Melbourne Australia, 20-25th July, 2014. |
| [2] | AVERT, “Averting HIV and AIDS in Kenya,” 2012. |
| [3] | NACC, “KENYA AIDS STARATEGIC FRAMEWORK,” NAIROBI, 2014-2019. |
| [4] | WHO, “Tuberculosis,” 2015. |
| [5] | KAIS, “Kenya AIDS Indicator Survey 2007,” KAIS, NAIROBI, 2007. |
| [6] | KNBS, “Kenya Demographic and Health Survey,” NAIROBI, 2014. |
| [7] | KAIS, “KENYA AIDS INDICATOR SURVEY,” NAIROBI, 2012. |
| [8] | WHO/UNAIDS/UNICEF, “Global Update on HIV treatment-2013,” 2013. |
| [9] | UNAIDS, “Global Report, 2013-fact sheet,” 2013. |
| [10] | M. CLINIC, “Diseases and Conditions HIV/AIDS,” p. HIV/AIDS Complication Mayor Clinic. |
| [11] | WHO, “MDG 6: Combat HIV/AIDS, malaria and other diseases,” 2014. |
| [12] | WHO, “HIV/AIDS-Fact Sheet No.360,” 2014. |
| [13] | UNAIDS WORLDS AIDS DAY REPORT , “Getting to zero,” 2011. |
| [14] | NACC, “KENYA HIV COUNTY PROFILES,” NAIROBI, 2014. |
| [15] | WHO,UNAIDS,UNICEF 2011, “GLOBAL HIV/AIDS RESPONCE, progressive report2011”. |
| [16] | MOH, “Kenya AIDS Indicator Survey,” NAIROBI, 2013. |
| [17] | Kenya National Bureau of Statistics (KNBS), “National Sample Survey and Evaluation Programme (NASSEP) Five,” NAIROBI,KENYA, 2012. |
| [18] | en.m.wikipedia.org/HIV/AIDS, “HIV/AIDS,” 28 May 2015. |
| [19] | UNAIDS, “GAP Report-2014,” 2014. |

 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML