-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2015; 5(4): 103-108
doi:10.5923/j.phr.20150504.04
Integration of Family Planning in HIV/AIDS Program in Solwezi District, Northwestern Zambia: Status and Perspectives
Tharcisse Mulindwa Nsiyi 1, Harrison N’guni 2, Ernest Phiri 3, Andrea Brezovsek 4, Berthollet Bwira Kaboru 5
1Former Senior HIV Clinical Care Officer, Family Health International, ZPCTII Project, Solwezi, Zambia
2Ministry of Community Development, Mother and Child Health, Solwezi, Zambia
3Family Health International, ZPCTII Project, Solwezi, Zambia
4School of Public Health, University of Lorraine, Nancy, France
5School of Health and Medical Sciences, Örebro University, Sweden
Correspondence to: Berthollet Bwira Kaboru , School of Health and Medical Sciences, Örebro University, Sweden.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
The aim of this study was to assess the status of Family Planning (FP) service uptake through its integration in HIV program for identification of determinants of its low use in Solwezi district of Zambia. Comparative quantitative FP/HIV data was gathered during quality improvement process from database at Zambia Prevention Care and Treatment Partnership (ZPCT) Consortium for 2012 and 2013. Qualitative data was collected using semi-structured interviews with 29 professionals, at the main urban clinic in the district, from January to June 2013. Two key indicators were assessed: HIV/FP referrals at facility level and male partners’ involvement in seeking HIV/FP services. Referrals between HIV and FP services during the first semester of 2013 increased by 1.0% compared to 2012, whilst male involvement in integrated FP/HIV services remained stagnant at 11%. Low male involvement in FP/HIV service was linked to busy spouses’ work schedules (74%), and lack of knowledge (16%). FP/HIV couple counseling was offered on selected clinic days in 74%, whilst lack of policy implementation encouraging male involvement was noted in 58% of responses. Fear of FP side effects (89%), long distances to the clinic (74%), lack of adequate health information on FP (17%) and unavailability of the preferred FP method (11%) were essential obstacles to service accessibility. Internal systems improvement indicated slight progress in cross-referrals reported. Interventions on the demand side are required, such as in strengthening male involvement in FP/HIV service. FP services in the district would also benefit from increased variety of accessible FP methods.
Keywords: Family planning, HIV, Integrated services, Solwezi, Zambia
Cite this paper: Tharcisse Mulindwa Nsiyi , Harrison N’guni , Ernest Phiri , Andrea Brezovsek , Berthollet Bwira Kaboru , Integration of Family Planning in HIV/AIDS Program in Solwezi District, Northwestern Zambia: Status and Perspectives, Public Health Research, Vol. 5 No. 4, 2015, pp. 103-108. doi: 10.5923/j.phr.20150504.04.
1. Introduction
- Zambia is one the countries in the Southern African region were maternal mortality is still high. According to the country’s demographic and health survey, maternal mortality ratio is estimated at 591 maternal deaths per 100,000 live births, with lack of adequate family planning access being one of the contributing factors to this high mortality ratio. Therefore, the obstetrical risk of pregnancy and childbearing is emphasized [1].Family planning service provision is one of the pillars for strengthening safe motherhood; however the country is still recording low levels of use of contraceptive methods, though there has been an increase over the years from 12% in 1992 to 30% in 2007 [1].In Zambia, although knowledge of family planning is relatively high in most of the urban areas, uptake and use of services is still very low, especially in peri-urban and rural areas. According to the 2007 Zambia Demographic and Health Survey (ZDHS), 70% of women do not use any form of contraceptives. Contraceptive use varies by province, with Eastern province having the highest proportion (53%), whilst Northwestern province stands among the lowest at 32%. [1]. In addition, despite the trend of increasing contraceptive prevalence, there is considerable unmet need for Family Planning services; thus efforts are needed for identification and mitigation of determinants and challenges. Reportedly, 27 % of married women have unmet needs for Family Planning services, 19% for birth spacing, and 8% for birth limiting [1].Sexual and reproductive health and HIV are intricately linked. According to the Joint United Nations Program on HIV and AIDS (UNAIDS) data, Zambia’s HIV prevalence is 14.3%, with the majority of HIV infections resulting from unprotected sex, followed by mother to child transmission either during pregnancy, delivery or during breast feeding [2].Women of child bearing age who are at risk of unintended pregnancy are also at risk of HIV infection. Voluntary family planning is an indispensable component of HIV prevention and treatment, as it increases access and uptake of HIV prevention information and services, constitutes a key entry point addressing HIV risk factors, safe sex negotiation, voluntary counseling and testing for HIV, prevention of vertical transmission of HIV, and other prevention interventions.Linking HIV services to family planning enhances support for dual protection, improves access to quality reproductive health services, reduces HIV-related stigma and discrimination, extends programs to underserved populations, promotes human rights and improves the quality of life for vulnerable and key populations, women, adolescent and youth living with HIV [3].Across the world there is consensus that establishing effective linkages and integration of sexual and reproductive health (SRH) and HIV services will not only increase access to and utilization of Sexual and Reproductive Health and HIV services, but will contribute towards people’s enjoyment of their sexual rights and significantly back the achievement of Millennium Development Goals, especially goal 3 (promoting gender equality), goal 4 (reducing child mortality), goal 5 (improving maternal health), and goal 6 (combatting HIV and AIDS).The government of Zambia recognizes that, in order to overcome sexual and reproductive health and HIV challenges, there is need to link and integrate and HIV services, in addition to tackling other social determinants of health [4]. Furthermore, the 2007 country’s demographic and health survey report noted that access to contraceptive methods is still a challenge due to inadequate information on FP methods, myths and misconceptions existing in the majority of the clients, combined with the low literacy level; with most of clients accessing selected contraceptive methods like implants and intra-uterine devices originating basically from the peri-urban setup. Efforts have been put in place in order to strengthen accessibility of FP service at health facility level, by coupling it to antenatal care (ANC) and prevention of mother to child HIV transmission (PMTCT) activities at maternal and child health (MCH) clinics.In Northwestern Zambia, a project on integration of family planning and reproductive health services into HIV/AIDS program was set and implemented by the Ministry of Health through the district medical office and health facilities, in conjunction with cooperating organizations and partners. This project, which this study is based on, was funded by the U.S. President's Emergency Plan for AIDS Relief (PEPFAR) through USAID, and managed by Family Health International FHI360 to support the Zambia Ministry of Health through provincial health offices and district health offices for the implementation of HIV program in selected provinces of the country. It focuses on providing technical support to Ministry of Health for quality implementation of HIV Prevention and Care strategies, including integration of reproductive health and family planning services into HIV program, preventyion of mother to child HIV transmission (PMTCT) and antiretroviral therapy (ART) service delivery. The Zambia HIV/AIDS Prevention, Care and Treatment Program (ZPCT) provides capacity building to health care workers by training staff in HIV service provision at health facility level.Based on the performance gaps identified by the quality assurance / quality improvement (QA/QI) team, a number of internal systems improvements strategies were adopted, including better data management and synchronization of activities by the HIV and FP programs. A number of supply side interventions were also selected to strengthen FP services uptake in the district and mitigate the challenges for its linkage to HIV/AIDS program. It is against this background that the present study was conducted to assess the current status of FP services uptake after initial (and essentially internal) efforts to improve its integration with HIV/AIDS program.The main goal of the study was to assess the prevailing situation of family planning service uptake through its integration into HIV/AIDS program. In this regard, the study specific objectives were:1. To determine the status of clients’ referrals between HIV and family planning services in the district2. To assess the level of male partners’ involvement in accessing integrated HIV/Family planning services at health facility level3. To assess determinants of non-compliance to family planning services at health facility level in the district.
2. Methods
- SettingsThe study was carried out in Solwezi district, the provincial headquarters of Northwestern Zambia, which records 65,876 women of child bearing age out of a total population of 299,436. The birth rate is at 32/1000; with a fertility rate of 146/1000 women in child bearing age. The district level data shows that the district strived to improve the family planning acceptor rate from 2010 to 2011 with an increase of 20/1000, compared to the current national target of 30/1000 clients. The Solwezi health district partners with various stakeholders for delivery of reproductive health and HIV services.Design and sampling strategyThis study applied both quantitative and qualitative methods, with a descriptive approach. For the purpose of achieving our study’s objectives, comparative quantitative data was collected from Zambia HIV/AIDS Prevention, Care and Treatment - Strategic Information and FP/HIV statistical database at the beginning of our the study in January 2013 to capture year 2012 data as baseline, then 6 months later in June 2013 to assess the impact of implemented strategies after a full semester.The information was compiled, based on selected indicators agreed upon by the QA/QI team. These indicators describing the level of FP/HIV service integration for both male and female adults and adolescents included the number of clients who were counseled and tested for HIV, the number of clients tested with their partners, the number of CT/PMTCT clients referred for FP services, the number of clients initiating ART and the number of new ART clients referred for FP services.Qualitative data was collected from professionals through key informant interview technique with aim to ascertain FP accessibility and HIV service integration at health facility level. For the purpose of this study, a survey random sample calculator was used to determine the sample size. Out of a total number of 31 professionals at Solwezi urban clinic which is the district referral health facility, 29 were individually interviewed to achieve 5% margin error at 95% confidence.Data collection and analysisQuantitative data was collected for FP and HIV program indicators from the health information aggregate reports at the district health office by health information officers of the QA/QI team. Comparative data was gathered from the strategic information system and FP/HIV statistical database at Zambia HIV/AIDS Prevention, Care and Treatment (ZPCT).Qualitative data was collected from professionals through key informant interviews. A semi-structured questionnaire was critically designed and validated by the quality improvement team to accurately gather the target information from health professionals to include respondent’s background, availability of integrated HIV/family planning services at health facility level, as well as accessibility and types of available family planning methods. The data was entered into SPSS 10 software for processing. Descriptive statistics with frequencies and proportions were used to analyze the data.Ethical considerations and study approvalFor the quantitative data, no details on patients were seen or available, only aggregate numbers as reported on patients’ movements were dealt with. As to qualitative data, confidentiality of all professional respondents was observed, and a voluntarily informed consent was obtained from all the participants prior to the interviews.Authority to conduct this study under the quality improvement project was duly granted by the Ministry of Community Development, Mother and Child Health through the District Medical Office and Health Management Team in Solwezi.
3. Results
- The fundamental task of our work in the QA/QI project was to assess the prevailing situation of family planning service uptake through its integration into HIV/AIDS program.Clients’ referrals between HIV and family planning servicesOut of a total number of 16,114 adults and adolescents clients counseled and tested for HIV, only 1,703 (10.5%) clients were referred to family planning services during the year 2012 in the district same year. Additionally, the district recorded 801 new adolescents and adults ART clients during the same year, out of which only 14 (1.7%) were referred for FP services. This trend persisted throughout the year 2012.
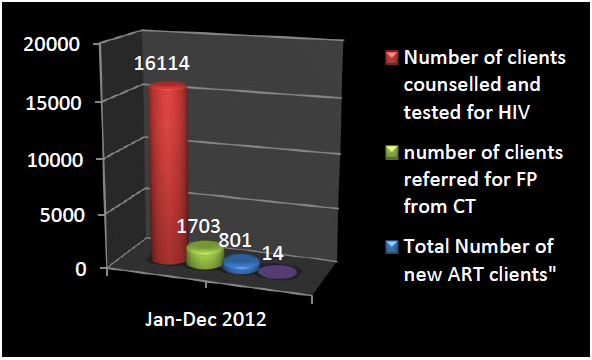 | Figure 1. Referrals from CT/PMTCT and ART at HIV clinics to Family Planning services in 2012 (Source: ZPCT database - analysis by authors) |
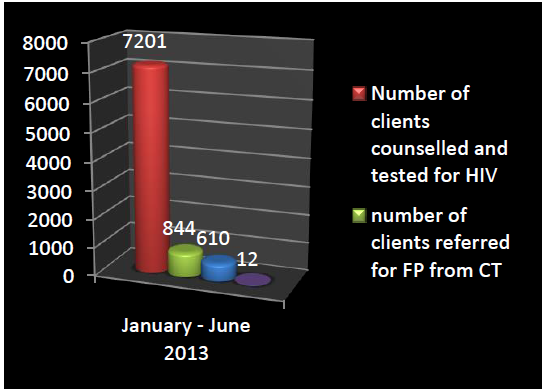 | Figure 2. Referrals from PMTCT and ART at HIV clinics to FP by the second quarter of 2013 (Source: ZPCT database - analysis by authors) |
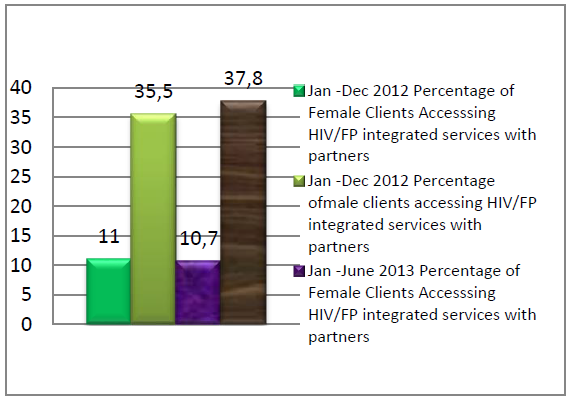 | Figure 3. Percentages female and male clients who accessed integrated HIV/FP services accompanied with their partners (Source: ZPCT database - analysis by authors) |
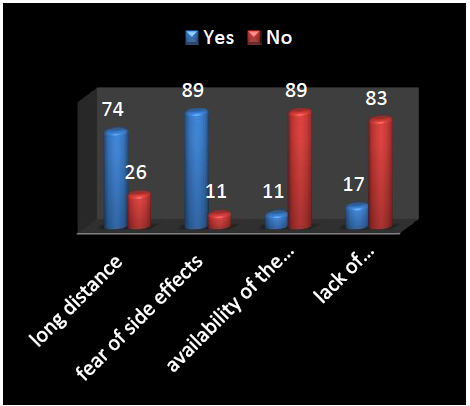 | Figure 4. Reasons for non-compliance to FP services at health facility level (Source: ZPCT database - analysis by authors) |
4. Discussion
- This study presented the portrait of the current prevailing stand of integrated HIV/FP uptake in Solwezi district of Northwestern Zambia, and provided appreciations of male partner’s involvement in couple response to FP service from the perspective of health professionals. The study follows a number of internal restructurings of the FP and HIV services in order to promote service provision in an integrated fashion.It was observed a slight numerical increase of approximately 1% in documented referrals from HIV clinics to FP services by Mid-2013. This was attributed to various factors which enabled strengthening of internal referral systems at health facility level, with improved documentation and updated referral registers, record keeping and feedback. Integration of FP/HIV services is however still very low in this district. FP/HIV services suffer from recurring obstacles reported in relation to increasing FP services. These barriers for implementation of FP/HIV service integration are many. This study noted from professionals’ respondents that fear of side effects from FP methods (89%), long distances to reach the clinic (74%), as well as lack of adequate health information regarding FP (17%) and unavailability of the preferred FP methods (11%) constitute important obstacles to FP service accessibility at health facility level in Solwezi district.Visibly, men involvement in accompanying their partners when seeking FP/HIV services is still unsatisfactory. Male involvement in FP services is an old challenge in reproductive health services uptake in several African settings. One study from Senegal found that preventing unwanted pregnancy was hindered by lack of dialogue on FP issues [5]. Another from Ethiopia, found similar challenges including lack of information, inaccessibility to the services and the desire to have more children were found to be the reasons for low male involvement in family planning services utilization [6]. There are situations where men involvement in HIV/FP has been reported positive. In Kenya, men's positive attitudes towards FP being provided at HIV care clinics demonstrated support for the programmatic push towards integrated delivery models for FP and HIV services. But this study was conducted among HIV positive men [7]. It is unlikely that HIV negative men would be equally supportive. Similar findings were reported from Nigeria, where actually men referred from HIV clinics increasingly attended family planning sessions at FP clinics [8]. This seems to be an indication that HIV/FP service integration is more than critical for specific groups that are particularly at risk for both HIV infection (or exposing other persons to infection) and for reproductive health problems such as unwanted pregnancies; for instance one study from Cote d’Ivoire called for such service integration in favor of female sex workers [9].The existence of a policy on service integration does not mean that integrated services are in fact provided [10]. These are two different things needing careful and constant analysis and monitoring. In Zambia, policy advocating for integrated services exist but the level to which it is applied might differ from a district or health facility to another.In Swaziland, a study noted that the proportion of patients’ visits in which HIV/STI and maternal/reproductive health services are received varied considerably from a health facility to another from 9% to 49% [11]. Among the obstacles, there’s lack of sufficient training of health providers to provide both types of services, as found in a district in Tanzania where only one out of four providers were prepared to provide integrated services [10].Overall, the picture that this study presents is similar to the national standing reported in a study by investigators from the Population Council regarding provision and use of FP in the context of HIV/AIDS in the region for Zambia, Uganda and Kenya. The document reported major issues in prioritization of FP as an entry point for PMTCT service within the four strategies of the UN Framework to reduce HIV vertical transmission [12]. The report emphasized that availability of FP services at PMTCT sites does not ensure integration of HIV and FP messages; whereby PMTCT sites missed opportunities to provide clients with FP counseling. As a result, lack of adequate health education negatively impacted on community and individuals’ opinions about HIV positive and childbearing women [12].Based on our study’s findings, more interventions on the demand side are critical to foster substantial change in uptake of FP/HIV services in the district. In addition, comprehensive and separate population survey should be conducted to evaluate the determinants of low male partner’s involvement and non-compliance to integrated HIV/FP services in the district. Such a study would shed light on the root causes of the phenomenon by exploring the perspectives of the beneficiaries of services in the community.In the same vein, an inclusive functional multidisciplinary QA/QI team at district and health facility levels, comprising of representatives from residents and community-based health activists organized in various neighborhood committees would continue working towards sustainability of this particular health program in its scope of HIV/FP service integration at health facility and community levels. The inclusion of a sociologist or an anthropologist in this team would be of a great value, in order to design strategies best-tailored to socio-anthropologic and demographic contexts of the district. Baseline results and inputs from the community-based health activists and community health workers could therefore be used to develop communication strategies that address social norms and barriers to FP use in Solwezi district context, where distance to reach clinics is listed from this study to be one of the major barriers to FP access and use.Such demand side interventions should be coupled with operational research to determine the effects of community- informed behavior change communication strategies on FP uptake. One component of this research program would aim at investigating how social norms influence FP/HIV acceptance in view to designing the best ways for reaching HIV-infected individuals with FP information, and would be appropriate in this scenario of Solwezi district.Provision of adequate trainings to clinic staff and community health workers on integrated FP/HIV service delivery, as well as building facilitation and dialogue capacities at community level would be a key component of the follow-on project. An independent previous study conducted in the region by a research group under Policy Project in Lusaka, Livingstone, Kitwe, and Kabwe towns in Zambia in 2003 also stressed on the need to integrate community health workers in addressing barriers to HIV health care and FP services [13].Lastly, the district health team would strengthen its partnership with community leaders and other local stakeholders who have got potential to assist these efforts with inputs on the leverage topics to promote healthy behaviors for program sustainability.
5. Conclusions
- This study indicated that HIV/FP service integration can benefit from internal systems improvement especially in terms of reported cross-referrals between the programs. However, in order to reach optimal integration levels, more efforts are needed including harmonizing integrated FP/HIV clinic days at health facility level, as well as major interventions on the demand side such as male involvement strengthening in FP/HIV service. FP services in the district would also benefit from increased variety of accessible FP methods.
ACKNOWLEDGEMENTS
- The successful production of this article would not have been possible without the dedication of a number of institutions and individuals. Our sincere gratitude goes to the Academic team of the school of public health and epidemiology at the University of Lorraine in France, the Solwezi District Medical Office and Solwezi Urban Clinic QA/QI team, and the Family Health International’s Zambia HIV/AIDS Prevention, Care and Treatment Program (FHI360/ZPCT) in Northwestern Zambia.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML