-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2015; 5(4): 95-102
doi:10.5923/j.phr.20150504.03
Contribution of Socio-Demographic Factors on Antenatal Care in Bangladesh: Modeling Approach
Md. Kamal Hossain1, Md. Rafiqul Islam2, Md. Nuruzzaman Khan3, Md. Raihan Ali3
1Department of Population Science and Human Resource Development, University of Rajshahi
2Department of Population Science and Human Resource Development, University of Rajshahi, Bangladesh
3Department of Population Science and Human Resource Development, University of Rajshahi, Rajshahi, Bangladesh
Correspondence to: Md. Rafiqul Islam, Department of Population Science and Human Resource Development, University of Rajshahi, Bangladesh.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
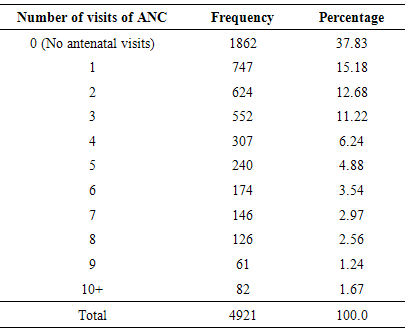
Background: Antenatal care (ANC) is essential for both mother and child health well-being. The risk of maternal mortality and morbidity as well as neonatal deaths can be reduced substantially through regular and proper antenatal care taken and delivery under safe and hygienic conditions. An attempt has been made to disclose how many times antenatal care (ANC) was taken by the pregnant mother and to find out the contribution of socio-demographic factors on ANC. Moreover, an effort is concentrated to find out a functional relationship between number of visits of ANC and the respondents.Data and methods: Data and necessary information of 4,921 reproductive women were obtained from the Bangladesh Demographic and Health Survey (BDHS) 2007. Multiple classification analysis (MCA) was used to identify the most important determinants of number of antenatal visit. Furthermore, negative exponential model was also employed here.Results: The results reveal that majority (37.83%) women have not taken any ANC during pregnancy and 15.18%, 12.68%, 11.22% and 6.24%, pregnant women have taken 1, 2, 3 and 4 times of ANC respectively. The result also reveal that only 1.67% pregnant women have taken 10 and above times ANC. MCA results showed that living condition, living place during pregnancy and TT injection before birth have been found to be the first, second and third contributing factors on number of ANC of pregnant mother. The grand mean of MCA result is 3.59 which indicate insufficient dose of ANC of pregnant mothers. Moreover, it is found that distribution of the respondents due to number of visits of ANC follows modified negative exponential model.Conclusions: This study demonstrates the low ANC service utilization. The utilization of the ANC service was influenced by various socio-demographic and health related factors. Hence there is a need to increase the availability and accessibility of health services to all women. Women’s overall status (education, living condition, living place during pregnancy and preceding birth interval) need to be considered.
Keywords: Antenatal care, Pregnant women, Multiple classification analysis (MCA), Modified negative exponential model, Cross validity prediction power (CVPP), F-test
Cite this paper: Md. Kamal Hossain, Md. Rafiqul Islam, Md. Nuruzzaman Khan, Md. Raihan Ali, Contribution of Socio-Demographic Factors on Antenatal Care in Bangladesh: Modeling Approach, Public Health Research, Vol. 5 No. 4, 2015, pp. 95-102. doi: 10.5923/j.phr.20150504.03.
Article Outline
1. Introduction
- Antenatal care (ANC) is the significant determinants of maternal health and vital for the health of mothers and their infants (AbouZahr, 2003). Lack of such care is commonly associated with the premature delivery, maternal and neonatal mortality (Rahman et al., 2007). Also, ANC has a positive impact on the utilization of postnatal healthcare (PNC) services which can significantly help to reduce maternal mortality because most maternal deaths occur in the first week after delivery (Hurt et al., 2008). Bangladesh has strengthened its ANC under the Directorate General of Health Services, through national and international collaborations (Islam et al., 2006). But the utilization of these services is very poor. It is reported that 55% of the pregnant women in Bangladesh make one ANC visit and about one-fourth (21%) of the pregnant women in Bangladesh make four ANC visit against four visits recommended by the World Health Organization (WHO) (NIPROT, 2009). About 63% of the pregnant women were not informed about the sign of pregnancy complication and only 10% of births are assisted by medically trained personnel (NIPROT, 2012). Again about 55% of the mothers received care from a medically trained provider, such as doctor, nurse, midwife, family welfare visitor, community skill birth attendant and medical assistant (Shahjaha et al., 2012). Efforts to address these issues have recently gained considerable attention with the formulation of the National Strategy for Maternal Health (MOHFW, 2011). This strategy emphasizes the provision of ANC and is predicated the framework of factors that affect safe motherhood service utilization (Carroli et al., 2004). These factors are related to decision to seek care, in reaching a medical facility and in receiving adequate treatment (Michael et al., 2007 and Dickstein et al., 2008). Improvement of these factors shows the positive association to reduction of the maternal mortality (Sunil et al., 2010). Despite improvements, pregnancy related complications remain the leading cause of death and disability among women during pregnancy (Gill and Ahmed, 2004). Available information suggests that about 12,000 women in Bangladesh die due to pregnancy-related complications (Anwar et al., 2009). So that, developing the ANC is importance which require the actual determinates of ANC services. There exists many studies into the determinants of ANC. Pervin et al. (2012) indicated the delivery facility as the important determinant of ANC. Nafisa et al. (2011) identified that maternal education was the significant determinants of ANC and paternal education played a more important role in the use of routine antenatal care than the conventional wisdom suggests. Islam and Odland (2011) identify that urban rural differences, level of education and distance of service centre are significantly associated with the total number of ANC during pregnancy. Rahman et al. (2008) explained that urban rural differentials were significant in receiving antenatal care. Abedin et al. (2008) observed that respondent’s education, husband’s education and occupation, place of residence, current use of contraception, frequently visit of health workers to the respondents have been statistically significantly associated with the utilization of antenatal care received during pregnancy. Rahman et al. (2010) found that demographic and socio-economic factors were associated with ANC seeking behaviour among slum mothers in Bangladesh. Similar results were also found in case of Azerbaijan (Habibov, 2011). Michael et al. (2007) identified that socio economic disparities is the major causes of variation of antenatal care and antenatal care services that was more improved high social class. But, the studies by covering the broad range of socio economic and demographic factors associated with ANC services received are scanty.The purpose of this study was to determine the socio-demographic factors associated with ANC in Bangladesh. Moreover, an effort was given to find out a mathematical relationship between number of visits of ANC and the respondents. This can be helpful for the policy makers to initiate strategies in the aspect of improvement of ANC services.
2. Methods
2.1. Sources of Data
- The study utilized a representative set of cross-sectional data extracted from the Bangladesh Demographic and Health Survey (BDHS) 2007 was the fifth national level Demographic and Health Survey. The surveys maintained all the protocols prescribed by the World Health Organization and written consent were taken individually from all respondents. The surveys were carried out to provide up-to-date information on fertility and childhood mortality levels; fertility preferences; awareness, approval, and use of family planning methods; maternal and child health; knowledge and attitudes toward sexually transmitted infections; community-level data on accessibility and availability of health and family planning services; and prevalence of non-communicable diseases. These were designed to produce representative results for the country as a whole, for urban and rural areas separately, and for each of the seven administrative divisions. All ever-married women 12-49 years who were usual members of the selected households and those who spent the night before the survey in the selected households were eligible to interview. The details of the sampling survey design, survey instruments and quality control are reported elsewhere (NIPORT, 2009). However, a brief description is given in the following subsections.
2.2. Sampling and Sample Size Selection
- The sample for the survey was the nationally representative survey and covered the entire population residing in non-institutional dwelling units in the country. The survey used the lists of enumeration areas (EAs) prepared for the 2001 Population and Housing Censuses provided by the Bangladesh Bureau of Statistics as the sampling frames. An EA can include a group of small villages, or a village, or a part of large village. The primary sampling units for the surveys were the EAs that were created to have the average of about 100. The surveys contained location information, type of residences, the number of residential households, and number of males and females in the population. Administratively, Bangladesh has six administrative divisions: Barisal, Chittagong, Dhaka, Khulna, Rajshahi and Sylhet. Each division was subdivided into zilas (districts), and each zila into upazilas (sub-districts). Each urban area in an upazila was divided into wards, and into mohallas (an area of a town or village; a community) within a ward. A rural area in the upazila was divided into Union Parishads (UP) (the smallest rural administrative and local government units) and mouzas (a specific land area within which there may be one or more settlements) within a UP. These divisions allowed the country as a whole to be easily separated into rural and urban areas. The samples were stratified and selected in two stages. Each division was stratified into urban and rural areas. For analytical purposes, the data were restricted to ever-married women who were given birth within five year preceding the survey. So, non-pregnant women were excluded from this study to increase the specificity of the indicator because ANC services related to pregnant women. After excluding the women with missing information, finally data of 4,921 women were extracted from BDHS 2007.
2.3. Outcome and Explanatory Variables
- Number of antenatal care taken by the mother during pregnancy was considered the outcome variable of this study. Living condition of the respondents, antenatal care taken by the doctor or nurse/midwife, living place during pregnancy, antental: CS: family welfare visitor, respondents education, respondents husband occupation, preceding birth interval, age at marriage and TT injection before birth were considered the explanatory variable.
2.4. Statistical Analysis
2.4.1. Multiple Classification Analysis (MCA)
- In this study, multiple classification analysis (MCA) was used as statistical tool to evaluate the contribution of socio-demographic and health related variables. In this section, numbers of ANC of mothers have taken during pregnancy considered as dependent variable. Others variable were considered as explanatory variables. The Statistical Package for Social Sciences version 16.0 (SPSS Inc, Chicago, IL, USA) was used for statistical analysis.
2.4.2. Model Fitting
- Using the scattered plot (Fig.1) of the respondents due to number of visits of ANC, it seems that the data can be fitted by modified negative exponential model. Therefore, a modified negative exponential model is considered and the form of the model is
 y = c + exp(a-b*x) + u.where, x is the number of visits of ANC; y is the respondents; a. b. c are parameters but c is the modified term of the model and u is the disturbance term of the model. The software STATISTICA was used to fit the mathematical model.
y = c + exp(a-b*x) + u.where, x is the number of visits of ANC; y is the respondents; a. b. c are parameters but c is the modified term of the model and u is the disturbance term of the model. The software STATISTICA was used to fit the mathematical model.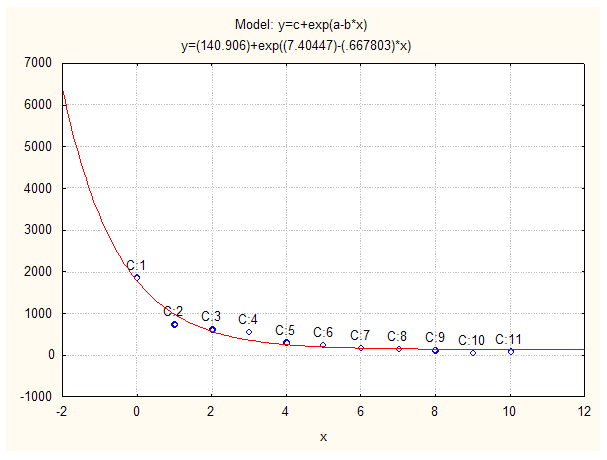 | Figure 1. The graph of observed and fitted distribution of respondents due to number of visits of ANC |
2.4.3. Model Validation Technique
- To check how much the model is stable over population, the cross validity prediction power (CVPP),
 , is applied. Here
, is applied. Here 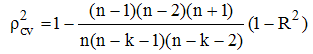 (Stevens, 1996)where, n is the number of cases, k is the number of predictors in the model and the cross validated R is the correlation between observed and predicted values of the dependent variable. The shrinkage coefficient of the model is the positive value of (
(Stevens, 1996)where, n is the number of cases, k is the number of predictors in the model and the cross validated R is the correlation between observed and predicted values of the dependent variable. The shrinkage coefficient of the model is the positive value of ( - R2); where
- R2); where  is CVPP and R2 is the coefficient of determination of the model. 1-shrinkage is the stability of R2 of the model. The information on model fittings and estimated CVPP have been demonstrated in the result section. This technique was also used as model validation technique (Islam et al., 2004; Islam, 2004, 2005a; 2005b; 2007a, 2007b; 2008; 2011, 2012a; 2012b; 2013; Islam & Hossain, 2013a; 2013b, 2014a, 2014b; Hossain & Islam, 2013; Islam et al., 2013; 2014; Islam & Hoque, 2015).
is CVPP and R2 is the coefficient of determination of the model. 1-shrinkage is the stability of R2 of the model. The information on model fittings and estimated CVPP have been demonstrated in the result section. This technique was also used as model validation technique (Islam et al., 2004; Islam, 2004, 2005a; 2005b; 2007a, 2007b; 2008; 2011, 2012a; 2012b; 2013; Islam & Hossain, 2013a; 2013b, 2014a, 2014b; Hossain & Islam, 2013; Islam et al., 2013; 2014; Islam & Hoque, 2015).2.4.4. F-test
- To verify the measure of overall significance of the model as well as the significance of R2, the F-test is employed here. The formula for F-test is given below:

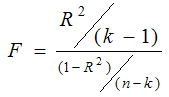 With (k-1, n-k) degrees of freedom and k = the number of parameters is to be estimated, n = the number of cases and R2 is the coefficient of determination of the model.
With (k-1, n-k) degrees of freedom and k = the number of parameters is to be estimated, n = the number of cases and R2 is the coefficient of determination of the model.3. Results
- A total of 4,921 women who were given birth preceding five years of survey were included in this study. The study showed that majority (37.83%) women had not taken any ANC during pregnancy and only 1.67% women received ANC more than 10 times (Table 1).
|
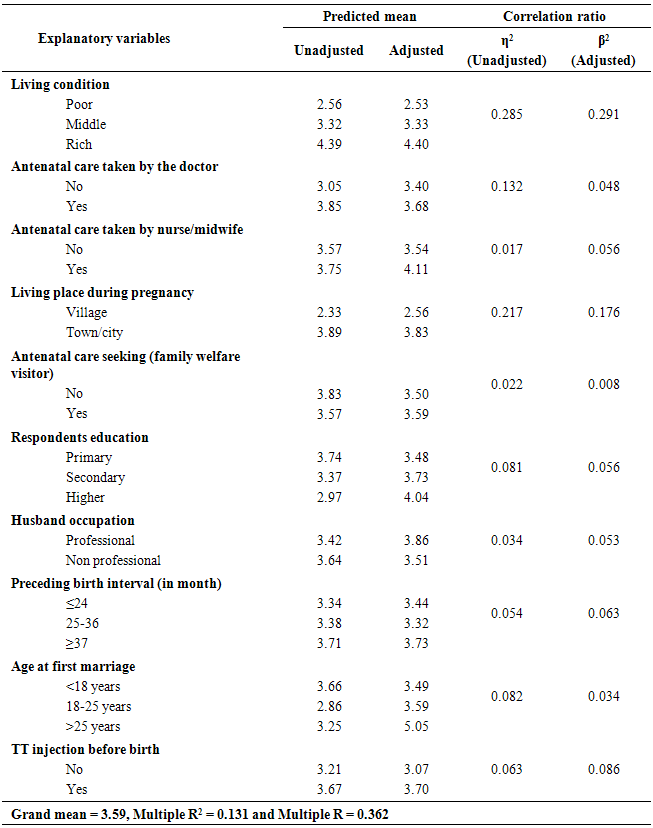
 ) have also presented in this table. About 13.1% (
) have also presented in this table. About 13.1% ( = 0.131) variation is explained by this model. The grand mean is 3.59. Associated factors of the number of visits of ANC services were determined through the MCA presented in Table 2. According to this table respondents living condition, living place during pregnancy, taken TT injection before birth, preceding birth interval, respondent education, antenatal care taken by the nurse/midwife, husband occupation, antenatal care taken by the doctor, respondent’s age at first marriage, antenatal care taken by the family welfare visitor have strongest influential factor successively for explaining the variation on number of antenatal care taken during pregnancy.
= 0.131) variation is explained by this model. The grand mean is 3.59. Associated factors of the number of visits of ANC services were determined through the MCA presented in Table 2. According to this table respondents living condition, living place during pregnancy, taken TT injection before birth, preceding birth interval, respondent education, antenatal care taken by the nurse/midwife, husband occupation, antenatal care taken by the doctor, respondent’s age at first marriage, antenatal care taken by the family welfare visitor have strongest influential factor successively for explaining the variation on number of antenatal care taken during pregnancy.
|
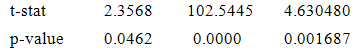 with coefficient of determination (R2) = 0.95765, CVPP = 0.94225, shrinkage coefficient = 0.0154 and stability of R2 = 0.9846.From these statistics it is found that the fitted model is highly cross validated and the shrinkage is also very small. Moreover, it is observed that all the parameters of the fitted model are statistically significant with large proportion of variation explained and the proportion of variation is more than 95%. And the stability of the model is more than 94%. The stability of
with coefficient of determination (R2) = 0.95765, CVPP = 0.94225, shrinkage coefficient = 0.0154 and stability of R2 = 0.9846.From these statistics it is found that the fitted model is highly cross validated and the shrinkage is also very small. Moreover, it is observed that all the parameters of the fitted model are statistically significant with large proportion of variation explained and the proportion of variation is more than 95%. And the stability of the model is more than 94%. The stability of  of this model is also more than 99%. Moreover, calculated F-test is 90.45 with (2, 8) degrees of freedom but its tabulated value is only 8.65 at 1% level of significance. Therefore, from these statistics it is found that fitted model is highly statistically significant. Hence, the fit of the model is very well.
of this model is also more than 99%. Moreover, calculated F-test is 90.45 with (2, 8) degrees of freedom but its tabulated value is only 8.65 at 1% level of significance. Therefore, from these statistics it is found that fitted model is highly statistically significant. Hence, the fit of the model is very well.4. Discussions
- The antenatal period is important for the health of mother and her up-coming baby. It is considered an important factor for improving infant survival. By considering this fact every region has initiated the program and policies and extends antenatal care coverage. However due to many factors women poorly recognize child bearing is problematic and therefore seek care (Chandhiok et al., 2006). The result of the present study showed that 37.83% mothers not received ANC services and only 6.24% mothers received ANC services four times. About 15.18% mothers received ANC services at least one times and about 12% received ANC service at least two (12.68%) and three (11.22%) times during the entire period of pregnancy. These findings are consistent with the recent study of India (Agrawal, 2010) and North Godar zone in Ethiopia (Nigussie et al., 2004) where about 60% and 45.7% mothers had antennal visit. The result of our study showed that living condition of the mothers was the most important strongest influential factor for the ANC service received. Mothers in poor live setting is less likely to received ANC services than that of rich. This finding is consistent with the others findings in Ghana (Arthur, 2012). Difference also observed among the mothers in rural and urban area. This is due to the improved medical facilities in urban area with good transportation system (Arthur, 2012). The findings of present study is consistent with the others findings in Vietnam (Tran et al., 2011; Tran et al., 2012) and Haiti (Alexander et al., 2005). Again mothers with the higher education had the highest percentage of adequate ANC use compared to those with primary education. The average number of ANC visit was higher in higher educated mothers (4.04) than the primary (3.48) and secondary educated mothers (3.73). The higher educated mother was higher than the four times minimum visits prior to delivery recommended by WHO, while that of the primary and secondary educated mothers was lower than the recommended average by WHO. This findings is consistent with others findings of Indonesia (Erlindawati et al., 2008), Bangladesh (Shahjahan et al., 2012), Vietnam (Tran et al., 2011), Haiti (Alexander et al., 2005) and Ghana (Arthur, 2012). Husband occupation is also considered importance influential factors for the ANC service received. The living standard of the mothers is mainly depended upon the husband occupation in the traditional families setting (Islam and Odland, 2011). This result is also consistent with findings of Ethiopia (Gedefaw et al., 2014), Nigeria (Onasoga et al., 2012) and Bangladesh (Islam and Odland, 2011). Age at first marriage is another strongest influential factor of ANC services. The present study shows that the mothers with low age at first marriage (<18 years) have the higher mean value of ANC service received. The possible reasons may be mothers with the low age at first marriage have faced greatest pregnancy complication (Sumon, 2014). This facts contribute to the higher mean value of ANC visit and consistent with the findings of Nepal (Pradhan et al., 2013) and the cross sectional study of South Asia (Godha et al., 2013). Similar result was also observed among the mother with highest birth interval. Mothers whose duration of childbearing at least 3 years has the highest mean value of ANC service received (3.73) than the mothers having at least two years birth interval (3.34). The findings of the present study is consistent with the others findings of Nigeria (Uthman et al., 2013) and Bangladesh (Islam and Odland, 2011).
5. Conclusions
- The present study highlights the relationship with ANC and some socio-demographic and health related factors. Living condition of the respondents, living place during pregnancy, taken TT injection before birth, preceding birth interval, respondent education, antenatal care taken by the nurse/midwife, husband occupation, antenatal care taken by the doctor, respondent’s age at first marriage, antenatal care taken by the family welfare visitor are the most strongest influential factors for the ANC services. It is also investigated that distribution of subjects due to ANC visit follows the modified exponential model. Therefore, improvement of the socio economic status of the mothers must be intensified in order to increasing ANC services. In a long run, informal education to raise the awareness about necessary of ANC services and involvement of husband in this process are recommended. Furthermore, it is also recommended that this negative exponential model should convert to positive exponential model for better health of the mothers and their child.
ACKNOWLEDGEMENTS
- The Ministry of Health and Family Welfare (MOHFW), Bangladesh has supported data and reports to perform this study. The authors are very grateful to MOHFW, Bangladesh for this support. The authors gratefully acknowledge to the Department of Population Science and Human Resource Development, Rajshahi University; Bangladesh where the study has been conducted.
Abbreviations
- ANC: Antenatal care, PNC: Postnatal care, WHO: World Health organization, MCA: Multiple classification analysis, BDHS: Bangladesh Demographic and Health Survey.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML