-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2015; 5(1): 1-6
doi:10.5923/j.phr.20150501.01
Determinants of Delivery by Skilled Birth Attendants among Pregnant Women in Makueni County, Kenya
Harun Kimani1, 2, Carey Farquhar3, Peter Wanzala4, Zipporah Ng’ang’a5
1Lecturer Kenyatta University School of Public Health and Afya Bora Fellow with the University of Washington, Seattle, USA
2PhD candidate with Jomo Kenyatta University of Agriculture and Technology, Kenya
3Departments of Medicine, Epidemiology, and Global Health, University of Washington, Seattle, USA
4Centre of Public Health Research (CPHR), Kenya Medical Research Institute, Nairobi, Kenya
5College of Health Sciences, Jomo Kenyatta University of Agriculture and Technology, Nairobi, Kenya
Correspondence to: Harun Kimani, Lecturer Kenyatta University School of Public Health and Afya Bora Fellow with the University of Washington, Seattle, USA.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
Background: Skilled birth attendants (SBAs) can improve outcomes during delivery and postpartum by detecting and managing early complications of pregnancy and labor. The objective of this study was to determine factors associated with SBA utilization among women seeking antenatal care at rural community health units in Makueni, Kenya where less than 37% of women deliver with SBAs. Methods: Pregnant mothers were recruited at antenatal care clinics, enrolled and interviewed at baseline, then followed until delivery and for six weeks post-partum. Sociodemographic characteristics, knowledge and attitudes were compared using Chi square test and independent t tests among those who utilized SBA services and those who did not. Results:From January 2012 to January 2013, 324 pregnant women were interviewed at baseline and again at 6 weeks postpartum, of whom 172 (54%) reported delivery with an SBA. Women with secondary school education and above were 1.8 times more likely to choose skilled attendance at delivery compared to those with less education (Odds ratio [OR] 1.8, 95% confidence interval [CI]: 1.02 – 2.60), and women with previous pregnancies were 40% less likely to utilize skilled attendance during delivery compared to nulliparous women (OR 0.6, CI: 0.40 – 0.95). Women with male partners who had greater than a secondary school education were more likely to delivery with an SBA present (OR), and there was a trend for pregnant mothers accompanied by their spouses to the delivery to be more likely to deliver in a health facility when compared to those accompanied by other birth companions (OR 1.4, CI: 0.73 – 2.78). Access to a vehicle as a mode of transport to the place of delivery was strongly associated with increased likelihood of delivery with an SBA (OR 24.1, CI: 14.82 – 42.64). At the postpartum visit, women stated that the amount of money they had spent for skilled delivery was $67 which was significantly higher than the $30 USD reported for unskilled delivery (p = 0.001). Conclusions: Several factors were identified as independently associated with mothers not utilizing skilled care during delivery (education level, parity, transport availability) and the cost of delivery with an SBA was found to be more than double the cost without an SBA Interventions targeting these factors could increase uptake of delivery by SBAs and improve maternal and infant health in rural Kenya and other parts of sub-Saharan Africa.
Keywords: Pregnant women, Skilled birth attendants, Facility delivery, Kenya, Sub-Saharan Africa
Cite this paper: Harun Kimani, Carey Farquhar, Peter Wanzala, Zipporah Ng’ang’a, Determinants of Delivery by Skilled Birth Attendants among Pregnant Women in Makueni County, Kenya, Public Health Research, Vol. 5 No. 1, 2015, pp. 1-6. doi: 10.5923/j.phr.20150501.01.
Article Outline
1. Introduction
- The World Health Organization (WHO) defines skilled birth attendants (SBA) as health workers trained to manage normal, uncomplicated pregnancies, childbirth and the immediate postnatal period, and to identify, manage and refer women and newborns with complications (1). This cadre of health workers is made up of nurses, midwives, doctors and clinical officers found in different levels of the health care system. At all levels, they should have access to an enabling environment of equipments, supplies, drugs and transportation for referrals (2). WHO recommends that women be attended by a skilled birth attendant (SBA) during delivery to improve maternal and newborn health and survival, and the rate of deliveries by skilled birth attendance is considered a measure of progress towards achieving the millennium development goal of reducing maternal and neonatal mortality. The current target is that 80% of mothers receive skilled birth care by 2015. Various factors determine whether a pregnant mother will seek services of a SBA, including socio-cultural factors, access to health services, cost of both transport and services, mode of transport, friendliness of service providers, and access to alternative traditional attendants (3). Interventions such as referral to the facilities by opinion leaders, community health workers (CHWs), and traditional attendants, as well as offering a mode of transport, increase access to SBAs, and these efforts have been associated with improved maternal and neonatal health outcomes (4). Consequently, local efforts have increasingly addressed uptake of SBAs in an effort to reduce maternal mortality and improve maternal and child outcomes. Currently, Kenya has a maternal mortality ratio of 488 per 100,000 live births and neonatal mortality is 77 per 1000 (5). It is estimated that 37% of women deliver with an SBA in rural areas compared to 75% in urban areas. The purpose of this longitudinal study among pregnant and postpartum women in rural Kenya was to evaluate perceptions, barriers and acceptance of delivery by SBAs. The main objective of the study was to identify the determinants of delivery by SBAs among mothers in rural southeastern Kenya where rates of delivery by SBAs has historically been below the national average (6).
2. Methods
2.1. Study Design and Setting
- This longitudinal cohort study was conducted between January 2012 and January 2013 in Makueni County, Kenya. Pregnant women were recruited during routine antenatal clinic attendance in community health units and provided their written informed consent to study procedures and being followed until 6 weeks after delivery. The outcome of delivery by a SBA was ascertained at the 6-week postnatal visit.
2.2. Study Population, Recruitment and Follow-up Procedures
- Pregnant women were eligible for enrollment if they were > 18 years of age, less than 36 weeks gestation, presenting for their first antenatal visit, and planning to reside in the study area. At enrolment participants were interviewed and offered focused antenatal care (FANC). Routine care included education on danger signs in pregnancy, childbirth and the postnatal period; the need for delivery by SBAs; birth preparedness; nutrition and hygiene; and HIV prevention measures. Makueni County was purposively sampled due to low utilization of SBAs for deliveries. Tawa, Kisau and Kikima divisions were purposively sampled and equal numbers of mothers were followed up at each of the three sites. Baseline socio-demographic and pregnancy related characteristics were collected during the first visit, and health promotion sessions that the mother received were captured in subsequent questionnaires along with the number of ANC visits attended by each mother. An exit questionnaire was administered during the 6-week post-partum clinic visit to determine knowledge and attitudes concerning delivery by SBAs and traditional attendants, danger signs in pregnancy, child birth and the postnatal period, and knowledge about HIV in pregnancy. Delivery outcomes and place of delivery were cross checked in the mothers’ records. Questions on the attitudes towards SBAs and traditional attendants used a validated method of measurement of attitudes, the Likerts scale.
3. Statistical Methods
- Data analyses were performed using SPSS version 17 and STATA (StataCorp, College Station). Characteristics of those delivered by SBAs were compared to those who did not using Chi square tests; independent t-tests and logistic regression analyses were performed to identify the likelihood of delivery with skilled attendants for continuous and categorical variables. The Kenya Medical Research Institute (KEMRI) Ethical Review Committee reviewed and approved the research protocol.
4. Results
4.1. Socio-demographic Characteristics of the Study Population
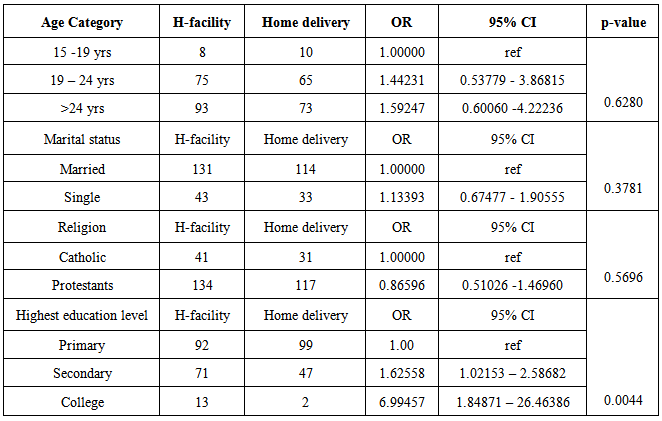
- A total of 324 pregnant women were enrolled to participate in the study, of which 245 (75.6%) were married. Median age of the participants was 25 years (interquartile range [IQR] 22 - 29). The majority of women were peasant farmers [234 (72.2%)] and of protestant religion [251 (77.5%)]. Parity ranged from 0 to 5 with [144 (44.4%)] women pregnant for the first time and [94 (29%)] having at least 2 prior pregnancies. A quarter of women [76 (23.5%)] were not married, and most had primary school education [191 (59%)] or had secondary education [118 (36.4%)]. Few women had college or higher education [15 (4.6%)]. Partners of female participants were mostly casual workers [170 (52.5%)] with primary education [125 (38.6%)] who resided in the study area [228 (70.4%)]. One hundred forty eight (46%) women enrolled in the study delivered at home while [172 (54%)] delivered at a health facility. Age, marital status and occupation, as well as religious affiliation, were not statistical different in terms of place of delivery (Table 1). Women who were more educated chose to deliver in a health facility more often compared to those who had primary education. Those who had secondary education were 1.8 times more likely to deliver in health facility (odds ratio [OR] 1.8, confidence interval [CI] 1.02 - 2.56, p < 0.01). The education level of the spouse was also significantly associated with place of delivery; women whose spouses had greater than primary level education were twice as likely to deliver under skilled care (OR 2.04, CI: 1.23 - 3.38, p = 0.01). In addition, nulliparous women were more likely to deliver with SBAs compared to multiparous women (OR 0.6, CI: 0.40 – 0.95, p = 0.03).
|
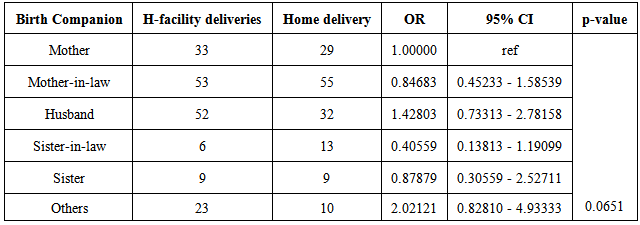
4.2. Birth Companions during Delivery
- The most common birth companions were mothers-in-law [108 (33.3%)], husbands [84 (25.9%)], and mothers [62 (19.1%)]; approximately 10% of women were accompanied by friends, neighbors, grandmothers, house help, brothers, and brothers-in-law (Figure 1). There was a trend for women accompanied by the mother-in-law to be less likely to deliver with an SBA (OR [0.84], 95% CI 0.45 - 1.58, p = 0.06). There was also a trend for women accompanied by their husbands to be more likely to have a skilled delivery (OR [1.42], 95% CI 0.73 - 2.78, p = 0.06) (Table 2).
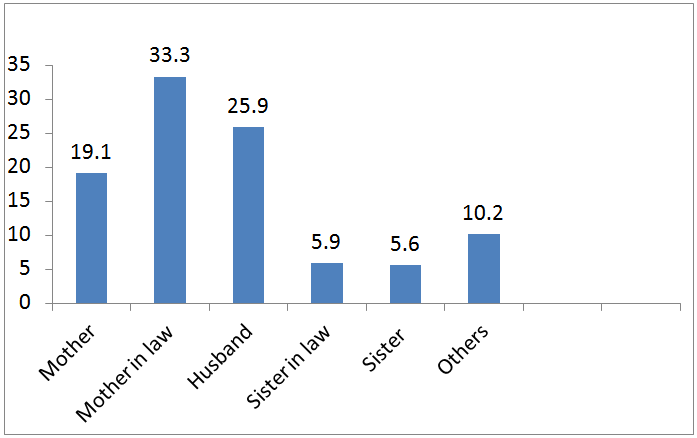 | Figure 1. Birth companions to the delivery |
|
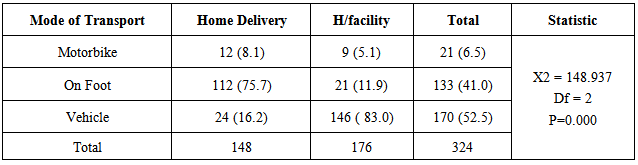
4.3. Mode of Transport Used by the Pregnant Women
- During delivery, [170 (52.5%)] pregnant women used a vehicle (car or truck) to go to the place of delivery while [133 (41.0%)] travelled on foot and [21 (6.5%)] on motorbike (Table 3). The type of transport used to the place of delivery was associated with place of delivery. Access to a vehicle for transport at the onset of labor was associated with a 24-fold increase in utilization of a health care facility for delivery compared to other modes of transportation (OR 24.14, CI: 14.83 - 42.64, p=0.01).
|
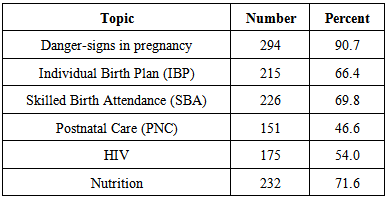
4.4. Knowledge and Attitude regarding HIV and Danger Signs in Pregnancy
- A total of 322 (99.4%) of mothers knew their HIV status and believed that mothers should be tested for HIV during pregnancy. More than 90% of women knew that a mother can transmit HIV to the fetus during labor, in utero and through breast milk. Most women were able to identify the following danger signs in pregnancy, childbirth and postnatal period: vaginal bleeding [316 (97.5%)], arm presentation [296 (91.4%)]; and cord presentation [291 (89.8%).] The least recognized danger signs were high fever for the mother [200 (61.7%)], and maternal convulsions [209 (64,5%)]. The level of knowledge on danger signs in pregnancy, child birth and the postnatal period was not associated with the choice of place of delivery.Most mothers had a favorable opinion of traditional birth attendants (TBAs) compared to SBAs, irrespective of the place they delivered [273 (84.3%) vs. 182 (56.2%)]. Knowledge of family planning (FP) was widespread and a total of 316 (97.5%) mothers knew of at least one family planning method, and 246 (75.9%) participants had used a FP method in the past. The most recognized FP method was oral contraceptive pills and Depo-provera at 95.7% and 95.4, respectively. Knowledge on contraceptives and their use had no association with the place of delivery. Whether the pregnancy was wanted or not had no statistical significant association with the place of delivery and whether a mother knew somebody who died due to pregnancy complications or not had no association with choice of place of delivery. In total, 101 (31.1%) women did not want any more children after the current pregnancy or wanted to delay having another child. Health promotion topics taught during antenatal period were reported as 1) danger signs in pregnancy [294 (90.7%)], 2) nutrition [232 (71.6%)], 3) skilled birth attendance [226 (69.8%)], 4) individual birth plan [215 (66.4%)], 5) HIV [175 (54.0%)] and 6) postnatal care [151 (46.6%)] (Table 4). A total of 58 (17.9%) women had heard of a mother who died due to pregnancy complications. The reasons for home deliveries for 148 mothers ranged from expense [138 (93.2%)] to onset of labor being too fast [134 (90.5%)]. A very high proportion of mothers [314 (96.9%)] strongly agreed that it is essential to deliver in a health facility. A total of 304 (93.8%) recommended making delivery cheaper and 288 (88.8%) recommended improved referral.
|
4.5. Cost and Payment for Delivery
- There was statistically significant difference between the mean amount of money spent on home deliveries and health facility deliveries ($30 USD vs. $67 USD, respectively, p < 0.01). The husband met costs of delivery for 236 (72.8%) participants, while the woman’s mother or the woman herself paid for the delivery in other cases [38 (11.7%) and 40 (12.3%), respectively].
5. Discussion
- In this study conducted in rural Kenya, delivery by SBAs was higher than expected at 54%, which is above the national average which is 46% (5). These results differ from those reported in other studies, which found SBA delivery rates of 37% in another rural part of Kenya and 7.4% in coastal Kenya (7). Many logistical barriers were identified in these two studies, including availability and cost of transportation. One explanation for higher rates in our study is that an unrelated program had been implemented shortly before the study started, this program was testing the “community referral model” and provided referral of expectant women by community midwifes.An important finding in this study was that both the woman’s and her husband’s education level were significantly associated with choice of an SBA. We saw a nearly 2-foldincrease in use of SBA when a woman had been schooled beyond the primary level, emphasizing the importance of education in utilization of SBAs in rural areas of Kenya. This finding was similar to that of Mpembeni et al. who in a Tanzanian study found that more years spent in school was positively associated with utilizing an SBA (8). We also found that male education above secondary school level was associated with a two-fold increase in the delivery by SBAs. This was similar to the findings of Nekesa et al. in a study on male involvement in maternal health in Bungoma in Western Kenya, where there was two-fold increase in delivery by SBAs when males were involved in antenatal care; the spouses level of education and employment were also significantly associated with SBA uptake (9). This suggests that there is a role for men in improving maternal and reproductive health outcomes and that promoting male involvement may be an important intervention. In this study we also found that nulliparous women were more likely to utilize SBAs which was comparable to what Manuela et al. found in Burkina Faso (10). There were also trends suggesting that the choice of birth companion was associated with utilization of SBA. Women accompanied by their mother-in-law were less likely to deliver at a health facility compared to women accompanied by their spouse. This finding is similar to that of Nekesa et al who also showed that male involvement was associated with delivery by skilled attendants (9). Reasons for these associations are not known, however, it is possible that men control the resources and their involvement results in the financial support necessary for facility delivery. These results also support the recommendation that potential birth companions be involved in the individual birth plan during the antenatal period and be educated about the benefits of skilled care at delivery. Furthermore, women should be encouraged to invite their spouse to be the birth companion based on what has been shown about the importance of male involvement. In addition, we found that access to a means of transportation determined delivery by skilled attendants: those who had access to a vehicle were 25 times more likely to deliver in health facilities compared to the other modes of transport. The magnitude of the effect size was surprising as was the finding that 93% of those who delivered at home cited transport and expense as the cause. This was similar to findings by Ngigi et al. who did a study in Western Kenya and found that 72.8% considered transport as the major problem. In that study only 29.3% of deliveries had skilled attendants (11). Preparing before delivery to cover costs of transport to a health facility has the potential to make a major difference to improve access to skilled care, as would a community ambulance. In this study, knowledge about some of the warning signs in pregnancy, child-birth and neonatal period was low. For example, only 61.7% knew fever and only 64.5& knew that convulsions were a warning sign. However, bleeding which is the main cause of maternal death was recognized by the majority of women (97.5%) as a danger sign. While most women knew the conditions that resulted in the demise of babies and women, knowledge was not significantly associated with delivery by SBAs. This is unlike findings by Mpembeni et al. in Tanzania where the knowledge of pregnancy risk factors was associated with an increased use of SBAs (8). The difference may be due to the fact that danger signs in pregnancy were taught to >90% of pregnant women during antenatal care in the current study. Possibly this education contributed to the >50% uptake of SBAs in this study, although, it was not designed to assess this.There were various potentially modifiable determinants for delivery by a skilled birth attendantin rural Makueni, Kenya, including education and. Raising the status of women through provision of education beyond primary school level may enable them to make better choices and deliver under skilled care. Additionally, intensifying counseling on the need for hospital delivery and making individual birth plans may enable more pregnant mothers to utilize skilled care at delivery. In addition, women of higher parity should be specifically targeted for counseling on the need for delivery in health facilities because they are less likely to deliver in a facility, perhaps because they believe the risk of delivery after already undergoing childbirth is reduced. Health workers should emphasize to the women of higher parity that every pregnancy has risks despite previous pregnancies having been uneventful. In conclusion focused antenatal care (FANC) should be intensified with emphasis on preparing a comprehensive birth plan that involves pregnant mothers, their spouse and other relevant family members, including mothers-in-law. For women to deliver in the presence of a skilled birth attendant, they may need support with transport and cost of services. Modifying health systems and training health workers on the importance of these determinants may increase the uptake of SBAs and hasten progress towards achieving millennium development goal number 5 and reducing maternal mortality.
ACKNOWLEDGEMENTS
- HK was a fellow in the Afya Bora Consortium Fellowship in Global Health Leadership supported by National Institutes of Health (NIH) Office of AIDS Research and PEPFAR, grant # U91HA06801B. CF received support from NIH award number K24 AI087399. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Text word count: 3700. Abstract word count: 322.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML