-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2014; 4(4): 120-128
doi:10.5923/j.phr.20140404.03
‘Falling on the Battlefield in the Line of Duty’ is not an Option: Knowledge as a Resource for the Prevention of Pregnancy Complication in Rural Ghana
Adadow Yidana1, Robert Kuganab-Lem2
1University for Development Studies, Department of Community Health and Family Medicine, School of Medicine and Health Sciences, Tamale, Ghana
2University for Development Studies, Department of Allied Health Science, School of Medicine and Health Sciences, Tamale, Ghana
Correspondence to: Adadow Yidana, University for Development Studies, Department of Community Health and Family Medicine, School of Medicine and Health Sciences, Tamale, Ghana.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
In many countries around the world especially in developing nations, pregnant women faces the risk of sudden, unpredictable complications, many of which end in death or injury to the expectant mothers’ or to their unborn babies. The unpredictability of such complications makes it imperative for countries and agencies around the world, especially the developing nations, to wage a war against needless and avoidable maternal mortality. In keeping with this, this study sought to establish women’s level of knowledge about danger signs and complications during pregnancy. Field data collected was gathered from two sub-districts (an intervention and a comparison) in the East Mamprusi District of the Northern Region of Ghana, using structured questionnaire. The study revealed that women in general are very conscious of antenatal visits. The majority of them (52.9% and 47.1% at the intervention and comparison communities) exhibited poor knowledge about the danger signs and complications associated with pregnancy. Aside from this is the fact that elderly women (over 50% in the age range 35-45years) in these communities are less likely to give birth at health facilities as compared to the young women. This paper thus concludes that health education should be stepped up for women in these communities and other communities alike if the war against maternal mortality is to be achieved.
Keywords: Pregnancy, Complication, Knowledge, Delivery, Mortality
Cite this paper: Adadow Yidana, Robert Kuganab-Lem, ‘Falling on the Battlefield in the Line of Duty’ is not an Option: Knowledge as a Resource for the Prevention of Pregnancy Complication in Rural Ghana, Public Health Research, Vol. 4 No. 4, 2014, pp. 120-128. doi: 10.5923/j.phr.20140404.03.
Article Outline
1. Introduction
- Enjoying the highest attainable standard of health is one of the fundamental rights of every woman of child bearing age irrespective of tribe, religion, economic or social class. Often time, different social-actors especially gender activist try to draw attention from the public, governments and stakeholders towards ensuring that the good health and wellbeing of mothers is achieved. A worrying situation however is that, despite these efforts, there has been less than satisfactory progress, especially in sub-Saharan Africa, towards achieving an acceptable maternal mortality rate if not eliminated altogether. In Ghana like other developing nations, maternal mortality rate remains unacceptably high at 451 per 100,000 live births [9]. One way of improving maternal health is to provide care through skilled professionals during pregnancy and childbirth. It is worth noting that many developing countries have taken maternal and child health with some level of seriousness. In view of the role mothers play in society, studies on this area have generated quite a number of useful data. It is however important to indicate that majority of these data are related to undesirable outcome of home delivery [22]. While we ponder over this issue, we must bear in mind that the rate at which women receive antenatal care and its quality is very important in predicting delivery outcome [1].According to [28], the increasing rate of maternal mortality in Sub-Saharan Africa remains one of history’s puzzling on-going tragedies, and reducing it continues to be a major challenge. It is important to note that women in the developing countries have a higher chance of dying during pregnancy or childbirth than women in developed countries. In this regard, the current situation as found in Ghana needs concerted effort from all stake holders. The 2008 Ghana Demographic and Health Survey showed that in almost 6 out of 10 births in Ghana, fifty-seven per cent (57%) of them occur in health facilities and forty-two per cent (42%) of births occur at home. Unfortunately, when one looks at the situation in the rural communities, home birth was noted to be higher, with fifty-eight per cent (58%). As [13; 16] has indicated, pregnancy related complications are sometimes very difficult to predict, and differences in gender role has created a situation where people are of the opinion that maternal mortality is akin to ‘Women falling on the battlefield in the line of duty’ [17]. Though it is the biological right to reproduce, it must not be viewed in that light. In traditionally oriented societies, newborns are often delivered at home without any expert supervision [12]. As part of the cosmological structure of the local people, the idea is that the moral status of a woman is raised when she delivers successfully at home [5]. A woman’s ability to deliver at home presupposes that she is faithful, whereas those who deliver outside their matrimonial homes are claimed to be unfaithful to their partners. Individual adherence to normative practices within societies generates both ‘rewards’ and ‘punishments’ as social actors continue to interact. Available data from the East Mamprusi District in the Northern Region of Ghana showed that low patronage of available health services, including supervised deliveries and post natal care continue to persist even where financial and geographic access is deemed adequate [8; 26], suggesting that the existing traditional practices serve as key barriers to the up-take of maternal and newborn health services [25; 27; 11]. In Ghana like other African countries, maternal deaths are thought to occur due to three delays: delay in deciding to seek appropriate care; delay in reaching an appropriate health facility; and delay in receiving adequate emergency care once at a facility [2; 19]. Obstetric complications during pregnancy greatly add its quota to maternal mortality in many countries around the world. These complications, it must be noted, can sometimes be prevented if women have access to obstetric care (26); especially with regard to receiving proper antenatal education. Women who are educated about when to seek care from medical professionals are more likely to seek care in a timely manner during complications (7). The objective of this paper is to explore the current level of knowledge about danger signs that could occur during pregnancy.
2. Methodology
- The study was conducted in the East Mamprusi District, located in the Northern Region of Ghana. The District has an estimated total population of 129,000. Average household size is 7.7 and almost half of married women (48%) are in polygamous unions. Educational status of women and girls is very low with 78% of them being illiterate, and one in 6 pregnancies occurs in girls 15-19 years old [10]. Approval for the conduct of this study was given by authorities of the Ghana Health Service. Verbal informed consent was also sought from all study participants before the commencement of any interviews or study activity. Study participants were free to refuse or withdraw from the study at any time without any penalty. The study’s purpose and objectives were explained to each participant prior to interview.Two sub-districts were selected out of five sub-districts in the East Mamprusi District. One of them served as an intervention district and the other a comparison district. However, the intervention and comparison communities were far apart with similar health outcomes, health infrastructure and health staff. The aim for this was to find out where there were similarities or differences in behaviour. The Intervention Group received an innovative intervention in addition to standard maternal health services available to women in Ghana. The Comparison Group received only the standard maternal health services. A sample size of 1,020 (510 per study arm) study participants was estimated in order to have a 90% chance of detecting a significant difference (at 95% confidence interval) in the primary outcome measure and assuming a correction factor of 2 (the “design effect”) for cluster sampling. A non-response rate of 10% was also considered in the sample size calculation. The sampling frame of the communities in both the intervention and comparison study areas was constructed using population data projected by the Ghana Health Service (GHS) from the 2010 population census. The primary sampling unit (PSUs) was the cluster. A total of 30 clusters were selected from the intervention study area and another 30 clusters from the control study area. In each cluster, 17 households representing 17 study participants were randomly selected and interviewed. Households with at least one woman who had delivered in the past 24 months were eligible for selection. In each cluster, a complete list of all households was compiled serially and systematic random sampling used in selecting study participants. In the first step, the total number of households in a cluster was divided by the expected sample size of 17 to give the sampling interval. The first household was randomly selected by picking any number from 1 to the calculated sampling interval. Subsequent selections were made by adding the sampling interval to the selected number in order to locate the next household to visit. If the selected household did not have a target respondent, then the next household was selected using the systematic sampling procedure. This was done until the sample size was obtained. In order to ensure reliability and validity of data collected, all field assistants were given training. The final stage in the training of data collectors was used to field-test the data collection tools. The main aim here was to refine the tools and to ensure the competence of the data collectors. Face to face interviews were conducted using pre-designed structured questionnaires to collect representative data. The research language was Mampruli and Moar, and English.
3. Data Analysis
- Data cleaning, range and consistency checks were done before the analysis was carried out using the Statistical Package for Social Sciences (SPSS) version18. Key outcome variables were compared between intervention and control arms. Categorical variables were compared on descriptive statistics using chi-square test to measure the significance of difference between proportions. For quantitative outcome variables, analysis of variance (ANOVA) was used to compare differences. Simple tabulations and cross tabulations were done for the data to look at frequencies of responses. Statistical significance of difference was considered at 5% significance level (p-value <0.05). Independent variables found to be significant at the 0.1 level based upon the results of the bivariate tests, were entered as potential variables to be included in multivariable regression analyses.
4. Results
- Below are the results of the data generated from the comparison and the intervention sub-districts in the study communities.
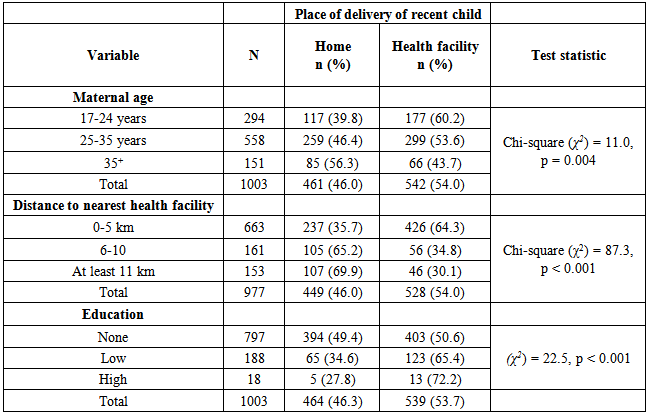
5. Socio-Demographic Characteristics of Sample
- A total of 1003 respondents were interviewed; 510 from Sakogu sub-district (Intervention Sub-District) and 493 from Langbinsi (Comparison Sub-District). The mean age of the respondents was 28.5 ± 6.6 years with the minimum and maximum ages of 17 and 49 years respectively. In all, majority of them were in the age group of 25-35 years. The mean parity was 3.6 ± 2.1 with a range of 1-10. Almost 52% (51.8%) of the respondents were from Mamprusi ethnic group. Amazingly, 79.4% had no formal education. Table 1 below displays the socio-demographic characteristics in the intervention and comparison communities.
 | Table 1. Comparison of socio-demographic characteristics of respondents |
6. Utilization of Antennal Care Services
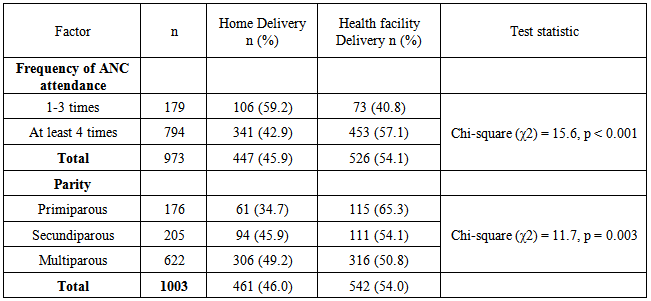
- Of all the women interviewed, 98.7% had attended antenatal clinic (ANC) at least once during the last pregnancy. For those who attended, the minimum number of antenatal care (ANC) visits was 1 whilst the maximum number was 12. Additionally, 997 of the women who could recollect the date of the first ANC visit showed almost all of them (99.9%) initiated ANC during the first trimester of pregnancy and only one started in the third trimester. Majority of the ANC attendees (81.6%) made at least four prenatal visits during the last pregnancy as recommended by the World Health Organization. In terms of adequacy of ANC attendance, 81.4% initiated ANC in the first trimester and also attended prenatal care at least four times during the last pregnancy. Table 2 shows the trimesters respondents initiated ANC and frequency of attendance. Between the study and comparison groups, there was no significant difference in the uptake of ANC services.
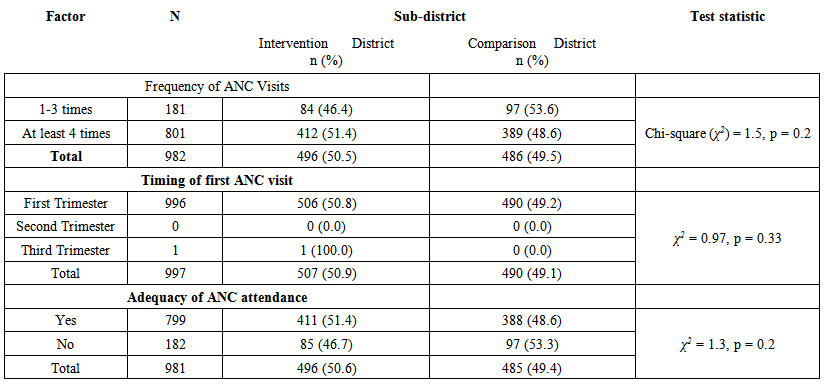 | Table 2. Uptake of Antennal Care Services and Practices |
7. Maternal Knowledge of Danger Signs and Symptoms during Pregnancy
- The research participants were asked about their knowledge of any signs and symptoms during pregnancy which demanded seeking immediate care from the health facility or from health workers. Generally, most of the participants, 78.5% recognized the fact that there are risks associated with getting frequent pregnancies and most, 88.2% felt the ideal birth interval should be 2-5 years. The types of risks of getting pregnant too soon after the birth of a child (Multiple Response) are shown in Table 3.
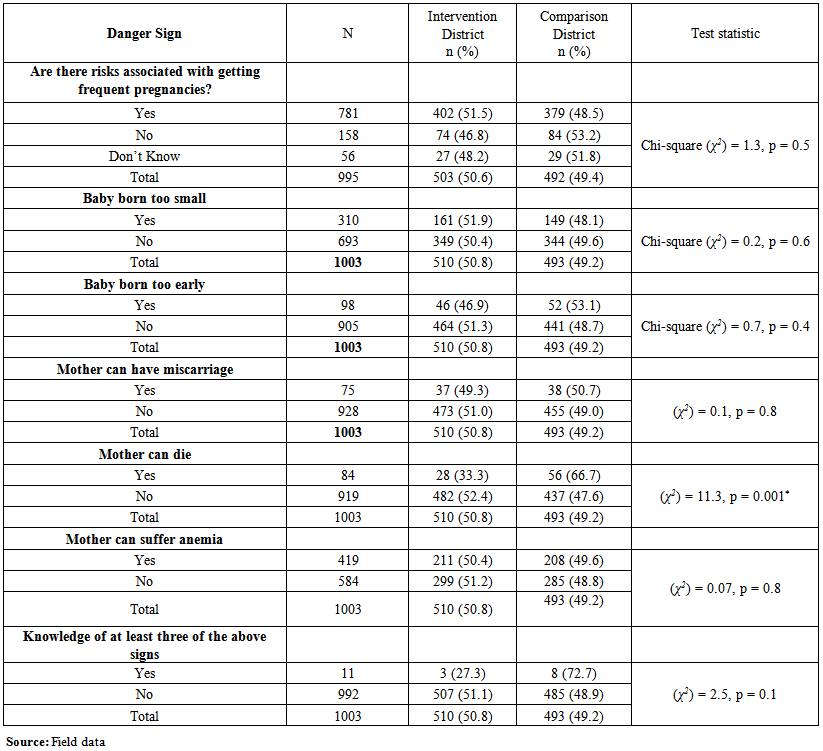 | Table 3. Maternal Knowledge on risks of getting pregnant too soon after the birth of a child |
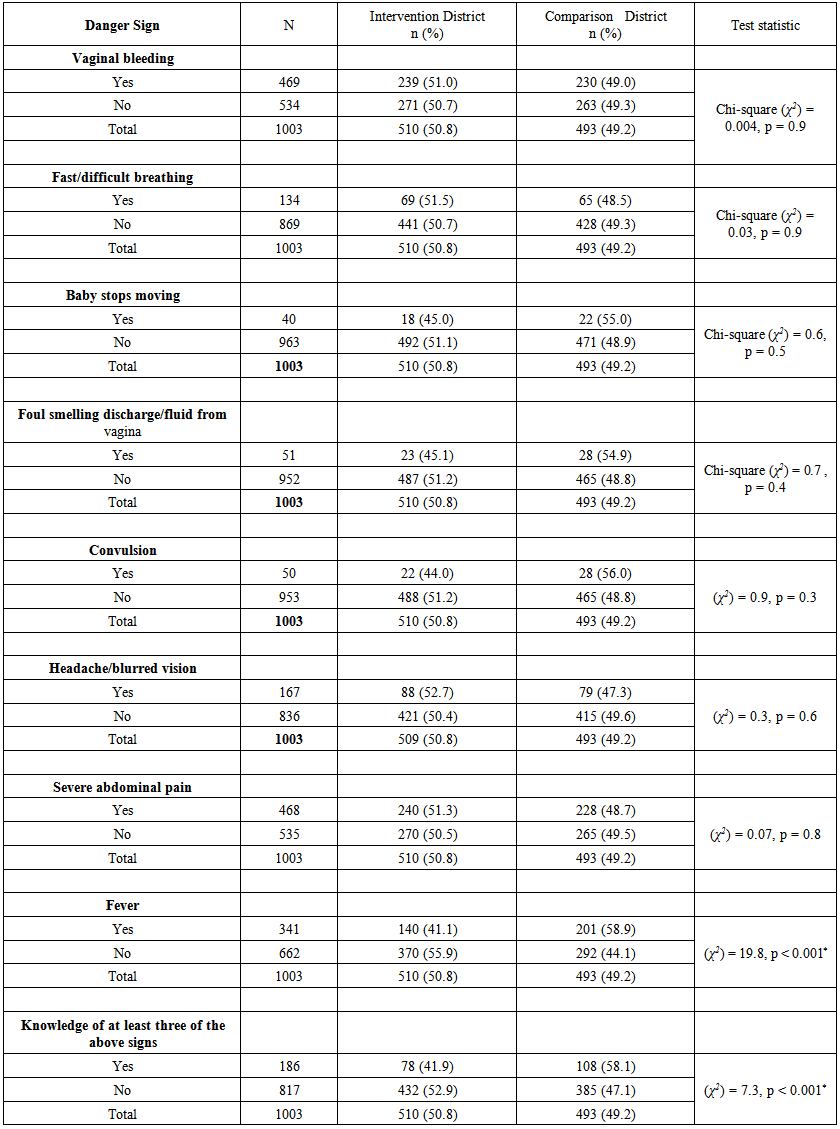 | Table 4. Maternal Knowledge of danger signs and symptoms during pregnancy |
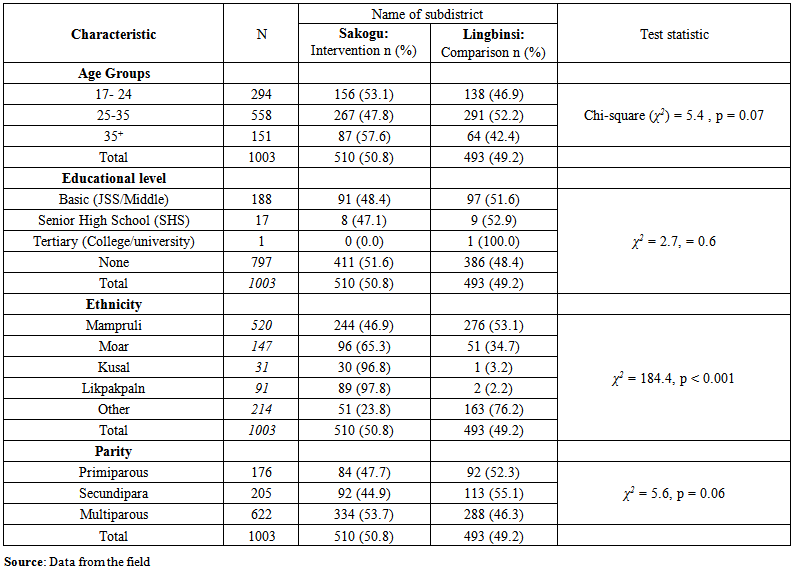
8. Predictors of Institutional Delivery
- Below are tables 5 and 6 showing bivariate analyses (differentials) of some predictors of place of delivery of the recent child. The use of health facility for delivery was significantly higher among Kusal tribe, young women, primiparous women, literate, frequent ANC attendees, women of high educational attainment and women living within 0-5 km of a health facility. Elderly women were less likely to have facility delivery compared to young women and the middle aged women (Chi-square (χ2) = 11.0, p = 0.004). This trend of old women not delivering in health institutions is a dangerous one that needs to be addressed. Women who attended ANC at least 4 times were more likely to deliver in a health facility. As ANC attendance increases, the proportion of institutional delivery also increases [Chi-square (χ2) = 15.6, p < 0.001]. Women who delivered in a health facility had mean ANC attendance which was significantly higher than those who delivered at home (5.3±1.7 versus 4.7±1.7), F (1, 976) =27.9, p <0.001. The kind of occupation of household head was also a significant predictor of place of delivery. For example, women from households headed by farmers were less likely to deliver in a health facility than those whose husbands engage in business activities.
|
|
9. Discussion
- As the statistics above show, factors in the study communities that have implications for maternal and child health have been identified. Out of a total of 1003 study participants who took part in the interview in the two sub districts, 51.8% of them belonged to the Mamprusi ethnic group with the remaining 48.2% belonging to other tribes. The study also revealed that of the total number of women interviewed, 79.5% of them had no formal education. The implication for this on maternal and child health is very high since much information would be missed out especially information on leaflets and brochures. This confirms results from the study that those with higher educational qualification attend ANC more than those with low or no education. In terms of parity, a total of 176 of the study participants had experience of first time pregnancy with 205 experiencing it for the second time pregnancy. However, 622 were in their third pregnancy and above. This outcome suggests that people would show different levels of experience regarding pregnancy related complications. This probably explains why ANC was higher among both the comparison and intervention districts. it is also likely that the absence of past complication could also have accounted for elderly women not likely to deliver at health facility. Irrespective of one’s place of abode, clients of antenatal clinics are supposed to be empowered with information about danger signs in pregnancy, child birth as well as during the post partum period. Knowledge of the danger signs of obstetric complications is an essential step in the recognition of complications and enables women to take appropriate action to access emergency care [23]. To ensure safe and complication free pregnancy, women are entreated to undertake early antenatal care within the first trimester. This is crucial because it allows for early detection and management of complications, as well as detection of existing diseases and treatment, promotion of health and prevention of disease [23; 4]. From the data, almost all participating respondents initiated ANC during the first trimester, as majority of the research participants, (78.5%) could recognize the existence of risks associated with getting frequent pregnancies. However, 88.2% express their opinion that the ideal birth interval should be 2-5 years. Knowledge is a vehicle to behavioural change [18], sadly, women in the two study areas (intervention and comparison communities) had poor knowledge of the danger signs of complications during pregnancy with only 1.1% [12] of the study participants being able to mention at least three of the risks associated with frequent pregnancies. Quite apart from this, only 186 out of the total of the 1003 study participants could mention at least three of the danger signs associated with pregnancy. This development is worrying if the war on eliminating maternal deaths is to be achieved. This could be the reason why maternal mortality continues to be high. This is because expectant mothers lack knowledge of danger signs of complications and so when they manifest, they do not take any concrete action, not because they do not want to, but because they do not know. It is however important to note that about 99.9% of women who initiated early ANC, did so during the first trimester of their pregnancies with only one attempting her first ANC visit during the last trimester. This is contrary to other studies that suggest that most women start their antenatal clinic during the second or third trimester [21]. The utilization of antenatal clinic was very high, with 98.7% of the study participants attending antenatal clinic at least once during the last pregnancy. Generally, 81% of them were able to pay at least four visits during the last pregnancy. This is encouraging in view of the public education on the need for ANC. Indeed, one of the most important functions of antenatal care is to provide the expectant mothers advice and information regarding birth preparedness, danger signs of obstetric complication and emergency preparedness [20]. Preparing and taking care of complications is a fundamental component of antenatal care whose aim is to reduce any unnecessary delays to seek emergency obstetric care hence improve maternal foetal outcomes [24]. It is worth noting that the most frequently cited risks associated with frequent pregnancies were, mother can suffer anemia and baby born too small. Other indefinable risk according to some of the study participants include; baby born too early, mother can have miscarriage, mother can die and were less obvious to the respondents. One other dimension worth mentioning is the fact that there are a number of complications in pregnancy that are associated with advanced maternal age. Despite that fact that older or elderly women are prone to complications during pregnancy, it is important to point out that elderly women in the study areas were less likely to have facility delivery compared to young women and the middle aged women (Chi-square (χ2) = 11.0, p = 0.004). This trend of old women not likely to deliver in a health facility is a dangerous practice that needs to be addressed. Vaginal bleeding, severe abdominal pain and fever were frequently mentioned but the rest were not cited by majority of the respondents. Only 18.5% of respondents could mention at least three of the danger signs and symptoms during pregnancy. Vaginal bleeding which is a danger sign of antepartum haemorrhage was not known by 50.7% and 49.3% in both the intervention and comparison districts. This is a worrying situation given that haemorrhage is the leading cause of maternal mortality worldwide responsible for 33% of all maternal deaths [14]. Equally more important worrying situation was the inability of most of the study participants to identify danger signs which indicate severe pre-eclampsia and eclampsia such as severe headache, blurred vision, among others. It is important to inform expectant mothers where they can seek emergency obstetric care when complication(s) occur in order to avoid unnecessary delays. Usually, the three identifiable delays (delay in deciding to seek appropriate care; delay in reaching an appropriate health facility; and delay in receiving adequate emergency care once at a facility [2]. These delays are attributable to the worldview of people, which seems to play a crucial role in the action they take in seeking health. As experts have indicated, what people consider to be plausible explanations in their day to day interactions informs the actions they embark upon in seeking health related solutions [6]. Indeed, many women turn to attribute the complications they face to all manner of forces, the primary one being witchcraft and sorcery [17]. Practices such as the use of Peligibu, Kalogutiim, Waligu, tidugukoom, and nangbantuom are among the traditional practices, serving as key barriers to uptake of ANC [27; 25; 3] This probably explain why many of the women have poor knowledge regarding danger signs during pregnancy. Many obstetric complications are unpredictable and can arise suddenly without warning [24]. Planning for emergencies like what transport to use during the day and at night when labour sets it, how much it would cost and availability of funds can help reduce delays in getting to hospital. It is ideal that every pregnant woman put down a written plan for emergencies. Though many of the study participants are aware of these dangers, transportation arrangement and distance to the nearest health post often poses as an obstacle. In the study, about 314 of the study participants travel over 6km to the nearest health facility. This situation, coupled with unavailability of funds for emergencies may be due to poverty or ignorance [19].
10. Conclusions
- As governments and stakeholders in Africa as a whole and Ghana in particular strive to reduce maternal mortality by 75% by 2015, health workers (midwives) need to provide comprehensive client friendly education and care to all women, especially expectant mothers when they visit health facilities, or when health workers visits communities as part of their outreach programs. This will guarantee provision of essential neonatal care to babies at birth as well as improve women knowledge of danger signs and symptoms of complications. Poor knowledge of danger signs, older women less likely to deliver at health facilities were significant issues identified that needs urgent action from policies makers within the health sector. Many of the participants, 76.7% are illiterates; suggesting why their knowledge of danger signs was very low. Many of them did not know about birth preparedness, thus, a large proportion of clients were not prepared for obstetric emergencies. If a well structured educational plan is put in place, the effects of the three delays that often lead to needless deaths of expectant mothers would be reduced. Other measure includes medication of cultural norms to be consistent with best practices, a strategy that would make the education acceptable. Based on this, it is crucial for antenatal care to place emphasis on birth preparedness and complication readiness to improve access to skilled and emergency obstetric care which has been shown to be critical in reducing maternal and/or perinatal mortality.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML