-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2014; 4(4): 117-119
doi:10.5923/j.phr.20140404.02
Prevalence of Pernicious Anaemia among Voluntarily Consenting Healthy Adults - A Report from North-west India
Sunil Kumar Raina1, Jagjit Singh Chahal2, Krishan Kumar Sharma2, Navjot Kaur3, Satyabushan Sharma2
1Department of Community Medicine, Dr. RP Govt. Medical College, Tanda (Himachal Pradesh), India
2Department of Biochemistry, Dr. RP Govt. Medical College, Tanda (Himachal Pradesh), India
3Department of Pathology, Dr. RP Govt. Medical College, Tanda (Himachal Pradesh), India
Correspondence to: Sunil Kumar Raina, Department of Community Medicine, Dr. RP Govt. Medical College, Tanda (Himachal Pradesh), India.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
Introduction: Pernicious anaemia is an autoimmune atrophic gastritis that causes a deficiency in vitamin B12 due to its malabsorption. Presence of intrinsic factor antibodies (AIFAb) is viewed as a diagnostic marker for pernicious anaemia. Materials and methods: This was an observational study carried out among healthy adults (students and employees) of in a medical college setting in north-west India. Results: By using reference range given by the manufacturer of the diagnostic kit, none of the participants enrolled for study was found to be positive for anti intrinsic factor antibodies (AIFAb) because all had serum level less than 25 EU/ml. Discussion: The study emphasises the need for further research in understanding the cause for vitamin b12 deficiency.
Keywords: Prevalence, Pernicious, Healthy adults
Cite this paper: Sunil Kumar Raina, Jagjit Singh Chahal, Krishan Kumar Sharma, Navjot Kaur, Satyabushan Sharma, Prevalence of Pernicious Anaemia among Voluntarily Consenting Healthy Adults - A Report from North-west India, Public Health Research, Vol. 4 No. 4, 2014, pp. 117-119. doi: 10.5923/j.phr.20140404.02.
1. Introduction
- Serum vitamin B12, has usually been seen to be lower among Indian toddlers and in adults, indicating hypovitaminosis. [1, 2] Chronic vitamin B12 depletion (i.e prolonged low intake or intestinal malabsorption) results in a state of negative vitamin B12 balance. Although the depletion process may take years to become clinically evident, early and reliable diagnosis of deficiency is crucial, owing to the latent nature of the disorder and the resulting possible irreversible neurologic damage. [3, 4] Megaloblastic anaemia is the usual culmination of deficiency of vitamin B12 or folate. Intrinsic factor (IF), a 60kD glycoprotein produced by the parietal cells of the stomach lining is required for the absorption of vitamin B12. [5, 6] Pernicious anemia is an autoimmune atrophic gastritis that causes a deficiency in vitamin B12 due to its malabsorption. Presence of intrinsic factor antibodies (AIFAb) is viewed as a diagnostic marker for pernicious anaemia. These are basically of Ig G isotype and occur in about 70% of patients of pernicious anaemia. [7] The study was planned with the aim to assess the prevalence of pernicious anemia among voluntarily consenting healthy adults using intrinsic factor antibodies (AIFAb) as a marker.
2. Material and Methods
- This was an observational study carried out among healthy adults (students and employees) of in a medical college setting in north-west India. The protocol and plan of study was approved by the institutional Ethics Committee. Voluntarily willing students and employees were recruited for the study after obtaining informed written consent. A total of 153 study units were picked by stratified random sampling method from the sampling frame that comprised of all students and employees of the medical college. Study plan and procedure was explained to the recruited participants. Blood sample was collected by following standardized procedure for the collection of blood sample. Inclusion Criteria: i) Any adult voluntarily consenting student or employee, aged 18 to 62 Years of the medical college. Exclusion Criteria i) Subject’s refusal. ii) Subjects who were taking methylcobalamin or vitamin B12 or folic acid or IFA or have taken the same for more than 15 days during last 3 months. iii) Subjects who had received vitamin B12 or iron formulations as injectables during last one year. iv) Subjects on medication for hypertension or diabetes or on lipid lowering drugs. v) Those with chronic illness like tuberculosis, cancer or immunocompromised subjects. vi) Pregnant or lactating mothers. vii) Anyone who had either donated or received blood in last three months. General Procedure for assay of AIFAb: 1:101 dilution of patient sample was prepared by mixing 10 μl sample and 1000 μl serum diluents.100 μl each of diluted sample, calibrator and control was pipetted into each microwell and microplate was incubated for 30 minutes. Plate was washed four times with wash buffer and 100 μl of conjugate was pipetted into each microwell. Plate incubated for 30 minutes at room temperature followed by washing for four times with wash buffer. 100 μl of enzyme substrate was pipetted into each microwell and microplate was again incubated for 30 minutes at room temperature. Reading was taken at 450 nm on BIO-RAD micro plate reader 550 after adding 100 μl of stop solution into each microwell.
3. Results
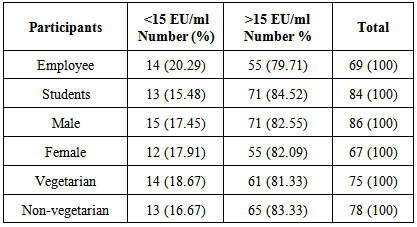
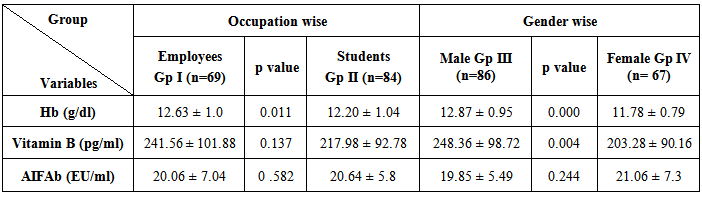
- We analyzed the serum samples of participants for the estimation of anti intrinsic factor antibodies (AIFAb). More than 80% of all participants enrolled for study had serum AIFAb level higher than 15 EU/ml (table 1). This analyte (AIFAb) in serum showed even distribution across all groups of study population and did not show any significant inter-group variation based upon occupation, gender or dietary habits. By using reference range given by the manufacturer of the diagnostic kit [8], none of the participants enrolled for study was found to be positive for anti intrinsic factor antibodies (AIFAb) because all had serum level less than 25 EU/ml. However, the test result was indeterminate for 126 participants who had a bit higher titre of AIFAb (more than 15 EU/ml but less than 25 EU/ml). Remaining participants (N=27) were tested to be negative for this analyte (<15 EU/ml). Though not significant, same pattern of inverse relationship existed between vitamin B12 and serum AIFAb. We observed some degree of age associated increase in the serum level of AIFAb. Interestingly though mean serum vitamin B12 in both the groups of employees as well as students, was low (group I N 69: 241.56 ± 101.88 pg/ml; group II N 84: 217.98 ± 92.78 pg/ml)(table 2). Using 200 pg/ml as threshold, 53.6% of total participants had low vitamin B12 concentration (66.6% of female students and 70.6% of female employees), while 16.3% of study population was severely deficient having serum vitamin B12 level below150 pg/ml.
|
|
4. Discussion
- Hypovitaminosis B12 is common among adults and elderly with a prevalence ranging from 15%–40% used. [9] . Hypovitaminosis B12 is represented by classic pernicious anemia (PA). [10] It accounts for 20%–50% of the documented causes of vitamin B12 (cobalamin) deficiency in adults according to a recent series. [11] In the general population, the prevalence of PA is 0.1%; in subjects over the age of 60, it reaches 1.9%. [12, 13].However, none of our enrolled volunteers showed a positive test result (>25EU/ml) for AIFAb. Of particular note was the occurrence of indeterminate test result for AIFAb in vast majority (N=126, 82.4%) of our study participants who had AIFAb titer between 15-20 EU/ml, whereas remaining participants (N=27, 17.6%) turned out to be negative for this test (AIFAb <15 EU/ml). Interestingly, though the results of our study showed a high frequency of suboptimal serum vitamin B12 in our study population. A total of 82 participants which makes 53.60% of the enrolled subjects, were having suboptimal level of vitamin B12. Of note was an observation that mean serum vitamin B12 level in younger age group (students) was lower than that in older group (employees). More of younger age group (58.34%) was in the suboptimal group, compared to older ones (47.82%). The study emphasises the need for further research in understanding the cause for vitamin b12 deficiency.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML