-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2014; 4(2): 51-61
doi:10.5923/j.phr.20140402.02
Effect of Health Education on Knowledge, Attitude and Uptake of Voluntary Counselling and Testing among Corps Members in Osun State, Nigeria
Eyitope Oluseyi Amu1, Foluke Adenike Olatona2
1Department of Community Medicine, Ekiti State University Teaching Hospital, Ado- Ekiti, Nigeria
2Department of Community Health and Primary Care, College of Medicine, University of Lagos, Lagos, Nigeria
Correspondence to: Eyitope Oluseyi Amu, Department of Community Medicine, Ekiti State University Teaching Hospital, Ado- Ekiti, Nigeria.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
TheHuman Immunodeficiency Virus (HIV) infection remains a significant public health problem especially in Nigeria where knowledge about HIV and Voluntary Counselling and Testing (VCT) is low and attitude to VCT and its uptake is poor. This study determined the effect of health education programme on the knowledge and attitudes to HIV and VCT and VCT uptake among unmarried National Youth Service Corps (NYSC) members in Osun State, Nigeria. It was a quasi-experimental study. Multistage sampling technique was used to determine 155 respondents in the intervention and 165 in the control groups. Baseline information was followed by health education programme on HIV and VCT for the intervention group. VCT services were provided weekly for three consecutive months for both groups. Three months later, post intervention data using the same questionnaire was collected from both groups. At baseline, there was no difference between the intervention and control groups in the proportion of respondents who had good level of knowledge of HIV (0.060); good knowledge of VCT (0.390), positive attitude to VCT (0.359) and uptake of VCT (0.618). Post-intervention, however, the proportion of respondents with these characteristic increased significantly only in the intervention group: good level of knowledge of HIV (p< 0.001); good level of knowledge of VCT (p< 001); positive attitude to VCT (p< 0.001) and VCT uptake (p< 0.001). There were also significant differences between the intervention and control groups in the proportion of respondents with each of these characteristics (p <0.001). Health education of youth corps members was significantly effective in improving their level of knowledge about HIV and VCT, attitude to VCT and VCT uptake. On-going health education and VCT services should be made available to corps members throughout their one year of compulsory service to the nation.
Keywords: VCT knowledge, Attitude to VCT, Health education
Cite this paper: Eyitope Oluseyi Amu, Foluke Adenike Olatona, Effect of Health Education on Knowledge, Attitude and Uptake of Voluntary Counselling and Testing among Corps Members in Osun State, Nigeria, Public Health Research, Vol. 4 No. 2, 2014, pp. 51-61. doi: 10.5923/j.phr.20140402.02.
Article Outline
1. Introduction
- HIV/AIDS is a significant public health problem in Nigeria. Its prevalence increased from 1.8 percent in 1991 to 4.6 percent in 2008. [1] Even though the average prevalence is lower than in some other sub-Saharan countries such as South Africa and Zambia, the large size of Nigeria’s population meant that as at the end of 2011, about 3.5 million people were infected with HIV [2].Voluntary counselling and testing (VCT) is one of the key strategies in the HIV/AIDS prevention and control programmes. VCT helps to change HIV-related sexual risk behaviours and serves as a gateway to most HIV/AIDS -related services. [3, 4] As a result of its central role in HIV prevention, treatment, care and support, the World Health Organization has advocated an accelerated scale up of access to VCT services in resource poor counties [5].VCT knowledge, attitude and uptake is not high enough in Nigeria. According to the 2008 Nigerian Demographic and Health Survey (NDHS), only 7 percent of women and 7 percent of men were tested for HIV and received their test results in the 12 months preceding the survey [6].The youth are the most vulnerable group affected by the HIV pandemic. About half of new infections occur among them, their HIV prevalence is higher than the national average of 4.6%, yet the VCT uptake among them is equally poor. [7, 8, 9, 10] Some undergraduates who are the educated youths even disapprove of VCT [11].Studies have shown that health education intervention is effective in increasing knowledge, improving attitudes and reducing students' sexual risk behaviour. [12] Young people who are at increased risk of being infected by HIV/AIDS and spreading the disease are most suitable for such health education. Such can be found among new graduates of higher institutions. The National Youth Service Corps provides opportunities to have access to a rich mixture of youth from diverse ethnic and cultural backgrounds in Nigeria. Little is known about the effect of health education on VCT knowledge, attitude and uptake among this group of people. This study determined the effectiveness of health education programme and provision of free HIV voluntary counselling and testing on its knowledge, attitude and uptake among National Youth Service Corps members in Osun State, Nigeria. The results would be useful in identifying areas where health education is effective or otherwise in the prevention of HIV.
2. Materials and Methods
- The study was conducted in Osun State, one of the six states in the Southwest geo-political zone of Nigeria. The National Youth Service Corps (NYSC) members are usually posted yearly to all the states in the country in two or three batches. They are usually between the ages of 20 and 30 years, mostly unmarried and represent different ethnic, socio-economic, cultural and religious groups in Nigeria. These new graduates first undergo a three-week orientation at the various NYSC orientation camps in the states, from where they are posted to institutions in all local government areas (LGAs) in the states. Osun State consists of thirty LGAs zoned into four NYSC Inspectorates. The two batches of corps members in the same LGA meet every Thursday of the week for Community Development (CD) work. They are usually divided into different CD groups depending on their areas of interest. Apart from the weekly CDs, all the corps members in each LGA also meet on the first Thursday of every month for compulsory general CD meetings. The local government Inspectors (LGIs) monitor the corps members and signs their attendance cards on such days.The study employed a quasi-experimental design (one that involved randomization at the group but not at the individual level, manipulation by the researcher and blinding. of the study participants). The study population consisted of unmarried corps members posted to Ife and Ilesa LGAs of Osun State. Assuming a 95% level of confidence, an estimate of VCT uptake of 17.8% among the control group respondents, an estimate of VCT uptake of 32.8% among the intervention group respondents, a statistical power of 80% and a level of significance of 5%, the formula for comparing independent proportions was used to obtain the minimum estimated sample size of 132 per study group. [13, 14] In order to compensate for non-responses, misplaced or improperly completed questionnaires and attrition, the calculated sample size was increased by 20%. The adjusted sample size became 158 per study group and a total of 316 respondents in all. A total of 330 participants were eventually interviewed.Respondents were recruited into the study by using multistage sampling technique. Osun State is divided into four NYSC Zonal Inspectorates each consisting of six or seven LGAs. Two of these, Ife and Ilesa Inspectorates, were selected by balloting. Out of the seven LGAs in Ife Inspectorate, Ife Central was chosen by simple balloting while Ilesa West was chosen in a similar manner out of the six LGAs in Ilesa Inspectorate. Through the process of simple balloting, Ilesa West was chosen as the intervention group while Ife Central emerged as the control group. The two LGAs were far apart enough to minimize information drift from the intervention to the control group. All eligible corps members, 155 in the intervention group and 165 in the control group were recruited into the study. The remaining corps members were married and so were not eligible. However, since the 155 study participants in the intervention group were still more than the minimum calculated sample size (132), the study continued.A pre-tested, semi-structured, self-administered questionnaire was used to obtain data. The questionnaire elicited information on respondents’ socio-demographic characteristics, their knowledge of HIV/AIDS, their knowledge and attitude to VCT and their uptake of VCT.The pre-test was carried out among corps members in Ede LGA, an entirely different LGA from the two that were used in this study. The results were analyzed and necessary corrections were made in the questionnaire before being administered to the study participants. This was done to ensure that the questions were clear and acceptable; there was willingness to answer them and that they were appropriate in eliciting responses that were consistent with study objectives. Ambiguous questions were re-phrased. Using the semi-structured, self-administered questionnaire, data was collected by the researcher, a resident doctor and two research assistants with the assistance of the field / zonal inspectors on one general ‘Community Development’ (CD) day when all corps members in the LGA assembled at the secretariat for ‘Community Development’. Data collection which took place in April 2009 was followed by health education programmes on HIV and VCT for three consecutive Thursdays at the intervention site. At the control site, health education on childhood illnesses and sickle cell disease was also given for three consecutive Thursdays. The research provided stand-by mobile VCT services free of charge for the corps members on site in both the intervention and control LGAs, for a period of three months after the last health educational intervention. The rapid HIV test kits Unigold®, and Determine® were used to test while Stat-Pak® was reserved for confirmatory tests. Trained VCT counsellors provided the services. All corps members that indicated willingness to be tested filled informed consent forms and had pre-test and post-test counselling. Their results were given to them in a confidential manner.The effect of the intervention was evaluated three months after the last health education interaction with the corps members. Information was collected using essentially the same questionnaire that was used during the pre-intervention phase. The questionnaires were administered to both groups of corps members on a general CD day, as was done during the pre-intervention phase. They were also retrieved on the same day. Knowledge of each respondent about HIV/AIDS was determined using 23 questions, each scored one point. Each correct response was scored one mark while non-response or wrong response was scored zero mark. Those who scored 11 points or less were considered as having poor knowledge; those who scored between 12-17 points were considered as having fair knowledge, while those who scored between 18-23 points were considered as having good knowledge of HIV. In determining the knowledge of each respondent about VCT, 5 questions, each scored one point, were used. Each correct response was scored one mark while non-response or wrong response was scored zero mark. Those who scored 0-1 points were considered as having poor knowledge; those who scored 2-3 points were considered as having fair knowledge, while those who scored 4-5 were considered as having good knowledge of VCT. In determining the attitude to VCT, 5 questions, each scored one point, were used. Respondents with correct attitude to three or less of the questions were considered as having negative attitude; while those with correct attitude to four or more of the questions were considered as having positive attitude to VCT. The data were analysed using the Statistical Package for the Social Sciences (SPSS) Version 15. Four-stage analyses were done: the comparison of the study and control populations pre-intervention to demonstrate similarities, the comparison of the control group data before and after intervention to show if there was any difference; the comparison of the study group before and after intervention, and comparison of the study and control groups post-intervention to show difference in each pair. Appropriate statistical tests of significance (chi square for comparison of proportions) between the two groups and within each group pre-and post-intervention were used. A p value < 0.05 was considered statistically significant. Analysed data was presented in the form of frequency tables.Ethical approval was obtained from the Ethical Committee of Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife prior to the commencement of the study. Permission to carry out the study among the corps members was obtained from the State Coordinator of the NYSC, Osun State and the respective LGIs. Written consents were also obtained from the respondents before being recruited into the study. The questionnaires were completed privately and anonymously and all records and relevant materials were stored in locked cabinets and accessed only by authorized personnel. Trained counsellors delivered the VCT services in order to further ensure confidentiality. Pre-test counselling was given before performing the test. Post-test counselling was also given to all clients irrespective of their results. The VCT results were given in a confidential manner. After collecting the post-intervention data, corps members in the control LGA were also exposed to the health educational messages delivered to the intervention group and vice versa.Three sessions of health education on HIV and VCT were given. A longer period of intervention could have resulted in greater increase in VCT uptake.
3. Results
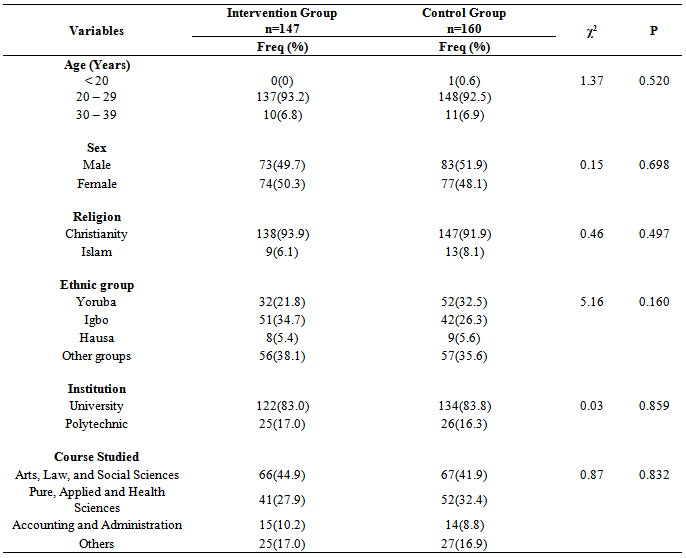
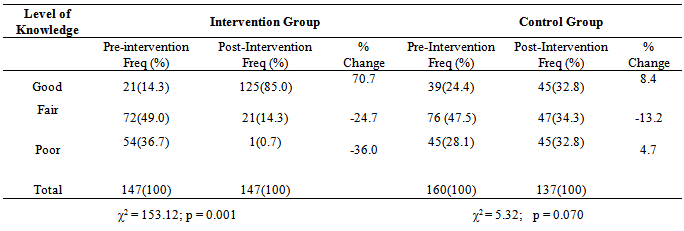
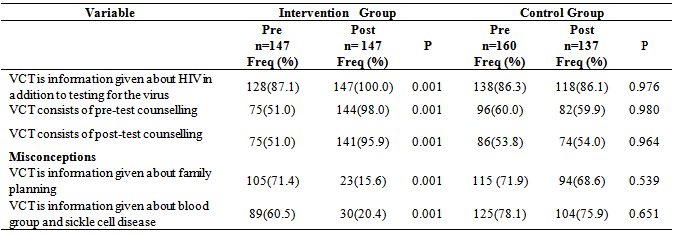
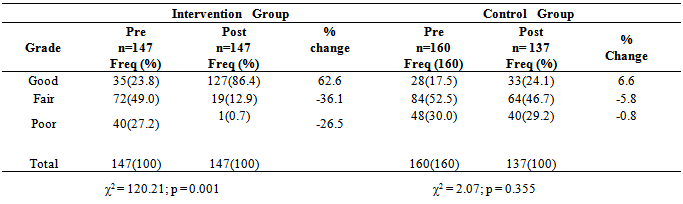
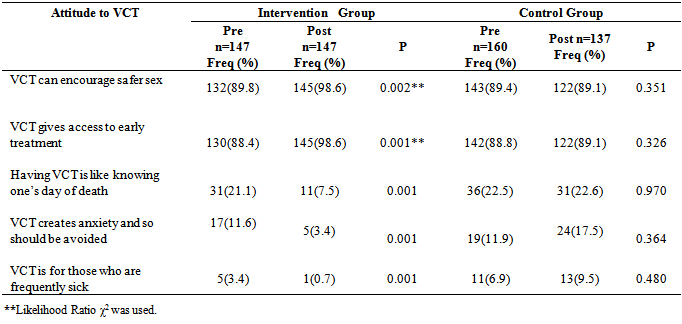
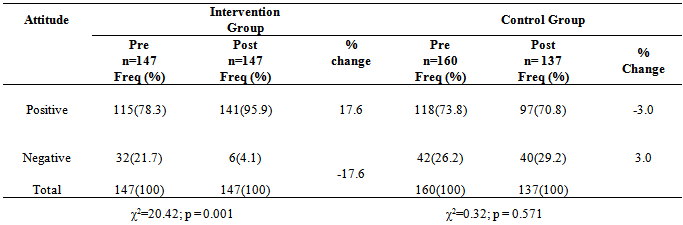
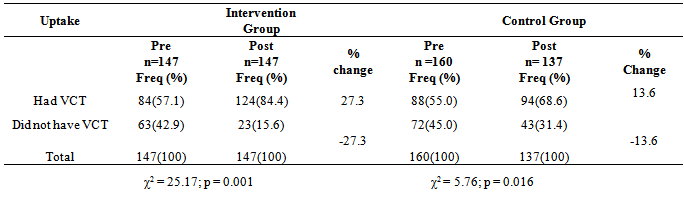
- Table 1 shows the socio-demographic characteristics of intervention and control group respondents. The mean (SD) age of the intervention and control group respondents were 26.08 (2.15) and 25.95 (2.25) years respectively. The mean age of the two groups were comparable (t = 1.94, p = 0.054). Although there were more males among the control group compared to the intervention group, the difference in the proportions was not statistically significant (χ2 = 0.15, p = 0.698). This was also true of other socio-demographic characteristics. Post intervention, the proportion of respondents with good HIV knowledge increased from 14.3% to 85.0% in the intervention group which was statistically significant (p=0.001). There was no such increase in the control group. There was also a statistically significant difference in the proportion of respondents with good knowledge of HIV between the two groups (Likelihood Ratio χ2 =103.16; p = 0.001) (Table 2). Post intervention, there was a statistically significant increase in the proportion of respondents who had correct knowledge about VCT in the intervention (p=0.001), but not in the control group (p>0.05). Similarly, there was a statistically significant decrease in proportion of respondents with misconceptions about VCT in the intervention (p=0.001), but not in the control group (p>0.05) (Table 3). Post intervention, there was a statistically significant increase in the proportion of respondents that had good knowledge of VCT in the intervention (p= 0.001), but not in the control group (p=0.355). There was also a significant difference in the proportion of those who had good knowledge of VCT between the intervention and control groups (LR χ2 = 131.79; p=0.001) (Table 4). Post intervention, there was a significant decrease in the proportion of respondents that agreed with the statements that having VCT is like knowing one’s day of death (p< 0.001); and VCT should be avoided because it creates anxiety (p<0.001) in the intervention group. There was no such decrease in the control group (p>0.05). Except for the respondents who agreed with the statement that VCT is for those who are frequently sick (p=0.095), there was a statistically significant difference in the proportion of those who agreed with all other statements about VCT between the intervention and control group (p=0.001) (Table 5). Post intervention, there was a statistically significant increase in the proportion of respondents that had positive attitude to VCT (p = 0.001) but there was none in the control group (p = 0.571). There was a significant difference in proportion of respondents with positive attitude to VCT between the intervention and control groups (χ2 = 32.95; p = 0.001) (Table 6). Post intervention, the proportion of respondents who had VCT increased significantly by 27.3% in the intervention group (p = 0.001); but only by 13.6% in the control group (p = 0.016). There was also a statistically significant difference in VCT uptake between the intervention and control groups (χ2= 9.85; p =0.002) (Table 7).
4. Discussion
- This study was conducted to evaluate the effect of health education intervention on knowledge and attitudes to HIV/AIDS and VCT; and VCT uptake among corps members in Osun State. The mean age of the respondents was 26.08 (2.15) years in the intervention group and 25.95 (2.25) years in the control group (Table 1). This is expected since most people would not have graduated from higher institution until they are about twenty years old and the age limit for compulsory service in the NYSC is 30 years. The NYSC members in the two local government areas were similar because there was no statistically significant difference between their socio-demographic characteristics.
|
|
|
|
|
|
|
5. Conclusions
- The health education intervention caused a significant increase in the level of knowledge about HIV and VCT among respondents in the intervention group. It also effectively improved their attitude to VCT and increased their uptake of VCT services (p<0.05). The policy implication of this study to the government, health planners, and policy makers in the National Youth Service Corps is that sustained skill-based health education and on-site VCT services should be provided for corps members throughout their one year of compulsory service to the nation. The health education should not only be targeted at improving their knowledge and correcting misconceptions about HIV/AIDS and VCT, but also at changing their risk perception for HIV/AIDS, encouraging safer sexual behaviours and motivating them to access VCT.
ACKNOWLEDGEMENTS
- The authors wish to acknowledge the corps members who were interviewed, the Osun State NYSC Director and the Zonal Inspectors.
Appendix

 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML