-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2014; 4(1): 31-38
doi:10.5923/j.phr.20140401.06
Demographic Correlates of Survival in Adult HIV Patients Registered at ART Centers in Andhra Pradesh, India: A Retrospective Cohort Study
Ram C. Bajpai 1, P. Y. Raj 2, Ugra Mohan Jha 3, Himanshu K. Chaturvedi 4, Arvind Pandey 5
1Research scholar, National Institute of Medical Statistics, New Delhi, India
2National Programme Officer, National AIDS Control Organization, New Delhi, India
3Programme Officer (Statistics), National AIDS Control Organization, New Delhi, India
4Scientist ‘F’, National Institute of Medical Statistics, New Delhi, India
5Director, National Institute of Medical Statistics, New Delhi, India
Correspondence to: Ram C. Bajpai , Research scholar, National Institute of Medical Statistics, New Delhi, India.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Limited research has been published particularly focused on demographic and programme indicators associated with survival and mortality among HIV/AIDS-patients in Indian scenario. Therefore, this study is designed to estimate the survival and associated demographic correlates among HIV-patients who registered at 31 functional ART centers in the state of Andhra Pradesh (AP), India during 2005-09. A total of 56, 992 adult (≥15 years) HIV/AIDS cases (32, 869 men and 29, 123 women) were registered in AP. Mortality density per 1000 person-years of ART registration was estimated across the demographic and programmatic variables. Cox-proportional hazard model was used to determine the relative hazard of mortality. More than 50% of PLHIV were died within the 6 months of ART registration. The overall mortality density was estimated as 28 per 1000 person-years at registration. The life-time median survival was estimated around 12 years that was slight higher among females. The stratified Kaplan Meier survival analysis illustrated that the survival probability was significantly different (p < 0.001) across the age and gender. Multivariate Cox regression analysis indicated that survival was significantly associated with age, sex, education, occupation, delay in ART registration and mode of transmission. Such information is useful for institution of intervention measures to reduce risk of death among PLHIV.
Keywords: ART, Demographic correlates, India, PLHIV, Survival, Delay in ART registration
Cite this paper: Ram C. Bajpai , P. Y. Raj , Ugra Mohan Jha , Himanshu K. Chaturvedi , Arvind Pandey , Demographic Correlates of Survival in Adult HIV Patients Registered at ART Centers in Andhra Pradesh, India: A Retrospective Cohort Study, Public Health Research, Vol. 4 No. 1, 2014, pp. 31-38. doi: 10.5923/j.phr.20140401.06.
1. Introduction
- HIV/AIDS infection remains one of the important public health problem and main cause of morbidity and mortality worldwide. After almost 30 years since the first case was reported, approximately 34 million people (31.6-35.2 million) were living with HIV (PLHIV) worldwide in 2010 that increased 17% from 2001[1]. Demographically the second largest country in the world, India has also the third largest number of people living with HIV/AIDS. National adult (male and female together with age ≥15 years) HIV prevalence was estimated as 0.31% (C.I.: 0.25-0.39%) in 2009 with persons living with HIV/AIDS were 2.40 million (C.I.: 1.93-3.04 million)[2]. Andhra Pradesh has second highest HIV prevalence (0.90%) after Manipur among six high prevalent states with more than 1, 00,000 PLHIV at one point of time[3]. As in the absence of cure for HIV, the antiretroviral therapy (ART) improved survival of HIV infected individuals worldwide since its inception[4, 5]. The primary goal of ART is to prolong lives, making HIV/AIDS as a chronic disease rather than death sentence[6]. The ART program in India was launched in 2004 under national AIDS control programme (NACP) and free services are being provided across 230 ART centers across the country[7]. As of Jan 2012 in Andhra Pradesh, 45 antiretroviral therapy (ART) centers are functional[8]. Extensive research has been conducted worldwide to estimate survival among HIV/AIDS infected individuals and underlying associated factors with mortality that includes demographic characteristics, laboratory variables and clinical indicators[9,10,11,12,13, 14]. A large scale household survey suggested that only 17% and 25% currently married women have heard about STIs and HIV, respectively[15]. Moreover, empirical research in India have reported conflicting trends in mortality rates; few studies reported increasing mortality trends among HIV infected individuals while another set of studies reported a decline in mortality rates over the years[11,12,16,17]. This has prompted researchers and policy makers to questions on contributions of ART on survival status of HIV infected individuals[11]. Demography of an individual plays an important role in their day-to-day life activities in both developing and in developed countries. There is a little evidence regarding demographic correlates of survival probabilities in HIV-infected individuals in Andhra Pradesh and India by large due to the lack of prospective studies. This analysis investigated the associated demographic determinants of survival probability in HIV/AIDS-patients registered at various ART centers in Andhra Pradesh (AP), India.
2. Methodology
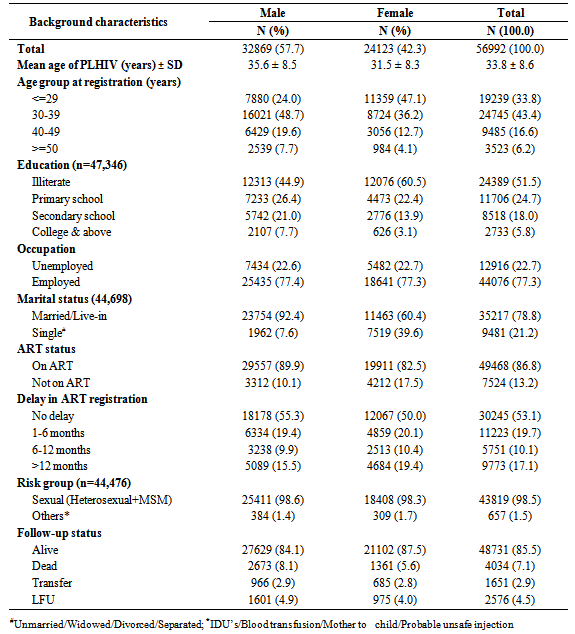
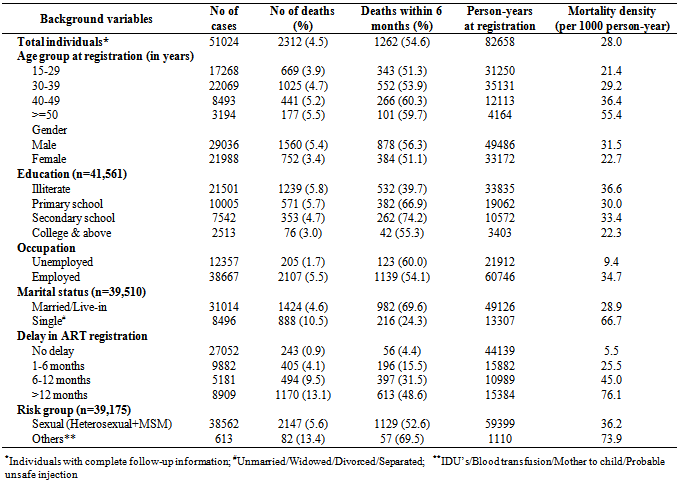
- Study settings and participantsThis article is based on individual level HIV-positive patient data registered at around 33 ART centers across the state AP from Jan 2005 to Dec 2009. A retrospective cohort of 63, 291 HIV-positive patients ware registered at different ART centers during 2005-09. Out of this, 56, 992 were adult (age ≥15 years; 32, 869 male and 24, 123 female) and remaining 6199 were registered as paediatric cases. Out of 32, 869 males 27,629 were alive, 2,673 died, 966 were transferred and 1,601 were lost to follow up. Similarly among 24,123 females 21,102 were alive, 1,361 were died, 685 were transferred and 975 lost to follow up during the period.All adult male and female were included in the present study. The baseline information on different demographic covariate includes: age, education, gender, marital status, occupation. It also includes important programme variables: year of HIV detection, year of ART registration, ART status, mode of transmission and the follow up status at the end of the study were taken (Table 1). Death of a HIV patient was taken as the primary end point. Individuals with missing date of death (n=1,722) were discarded from mortality density calculation as well as survival analysis and missing information within the variable is excluded during analysis (Table 2 & 3).
|
|
|
- Data description and analysisDemographic information on age, education, gender, marital status, occupation and vulnerability indicators: ART status, delay in ART registration, mode of transmission of HIV patients was categorized to assess any association with the survival probability. Age was categorized into four groups as ≤29, 30-39, 40-49 and ≥50 years. Education was categorized into illiterate, primary, secondary and college or above. Occupation was categorized as unemployed and employed. Marital status was categorized as single (unmarried, widow/widower, divorced/separate) and married/live-in. The ART status was categorized as on ART and not on ART. Delay in ART registration was sub-grouped into no delay (within month registration), 1-6 months, 6-12 months and >12 months. The mode of transmission was categorized as sexual (heterosexual+MSM) and others (injecting drug users/blood transfusion/mother to child). At the end, individual case in the database can be classified into the following four categories: alive, death, LFU/transferred and don’t know based on the status as on 31st Dec 2009.Pattern of death across the demographic variables was estimated using person-years of ART registration and mortality density. Survival time were measured as a duration between date of ART registration to date of death for patients who died or the date of the last recorded visit for patients who were censored (either alive till the end of the study period or lost to follow-up) and similar from date of HIV detection for life time survival (in years). For the comparison of unadjusted survival rates, Kaplan-Meier (K-M) methods were used and patients were stratified by different population sub-groups and it was plotted among different categories of demographic variables. We used the Wilcoxon log rank tests to assess statistical differences between the groups. To visually present the product limit estimates of the cumulative survival rate, Kaplan-Meier curves were generated to show the life time survival of the patients. Student’s‘t’ test was used for statistical difference between mean ages of male and female and Spearman’s rank correlation was applied for correlation between age and median survival.The widely accepted Cox proportional hazard regression model was applied to identify the associated demographic factors[12,13,14]. The proportional hazards assumption was tested using Schoenfeld residuals. Unadjusted hazard ratios (HR) and adjusted hazard ratios were estimated with 95% confidence intervals. The data were analyzed using IBM SPSS statistics for windows version 21.0 (Armonk, NY, USA). P value less than 0.05 was considered as statistical significance.Permission to use ART programme data for this study has been obtained from National AIDS Control Organization (NACO), Department of AIDS Control, Ministry of Health and Family Welfare, Government of India, New Delhi.
3. Results
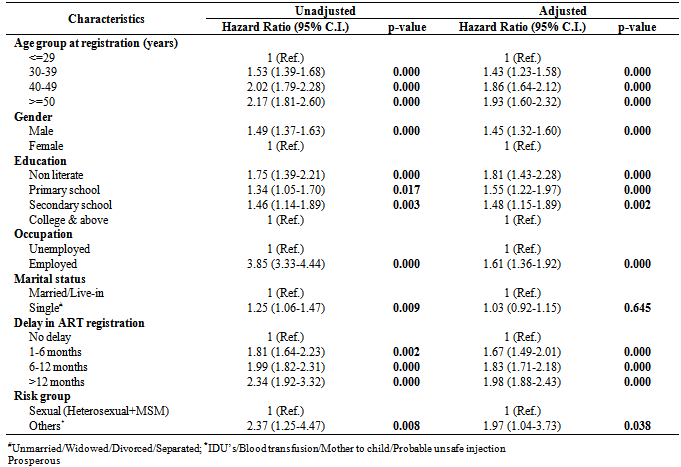
- A total of 56,992 adult HIV positive cases were registered at various ART centers across the state during 2005-09. The general profile of the respondents including demographics: education, occupation, marital status and ART status, delay in ART registration and their mode of transmission is presented in Table 1. The average age (±SD) at registration of PLHIV was recorded as 35.6 ± 8.5 years among male and 31.5 ± 8.3 years among female (t = 57.7; p < 0.001). More than 50% of HIV patients were acquired infection at their younger age (below 40 years), 51.5% were illiterate, 77.3% employed, 78.8% reported as married/Live-in, 86.8% were on ART, 53.1% were registered without delay, 98.5% of them were acquired HIV through sexual mode of transmission and 85.5% were alive at the end (Table 1). Complete follow-up information of 51,024 HIV patients and their mortality distribution during the study period was presented in Table 2. Around 7.1% PLHIV (n = 4,034) died during the follow-up period and 57.3% (n = 2,312) of them had registered with date in the database. 54.6% (n = 1,262) of them were died within 6 months of their registration. This confers an overall mortality density of 28 per 1000 person-years of registration for the state of AP for period 2005-09. The mortality density was higher in older age (≥40 years) and those who had low level of education (secondary and below). The mortality density was high among male, employed group and also in others risk groups. The mortality density increases as delay in ART registration increased (Table 2). The average delay (months) in ART registration was recorded as 6.0 months that increased till 2008 and then sharply decreased in 2009 (Fig. 1). Life-time survival was estimated to 12.1 (95% C.I.; 11.6-12.6) years that was slight higher among women 12.4 (95% C.I.; 12.0-12.8) years than men 11.6 (95% C.I.; 10.5-12.6) years. Further, the stratified Kaplan Meier survival analysis illustrated the survival probability was significantly different (p < 0.001) across the demographic groups except marital status (p < 0.645) as shown in Figure 2. The median survival after ART registration was estimated to 4.3 (95% C.I.; 4.2-4.7) years and it was also negatively correlated with age (r = -0.12; p < 0.001).
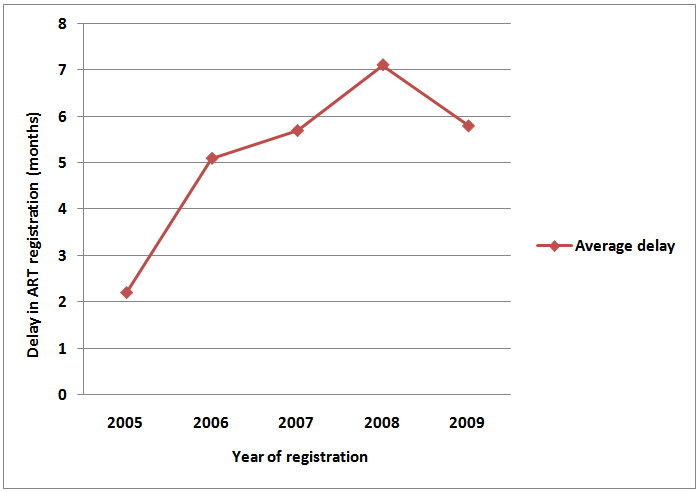 | Figure 1. Average delay in ART registration according to year registration |
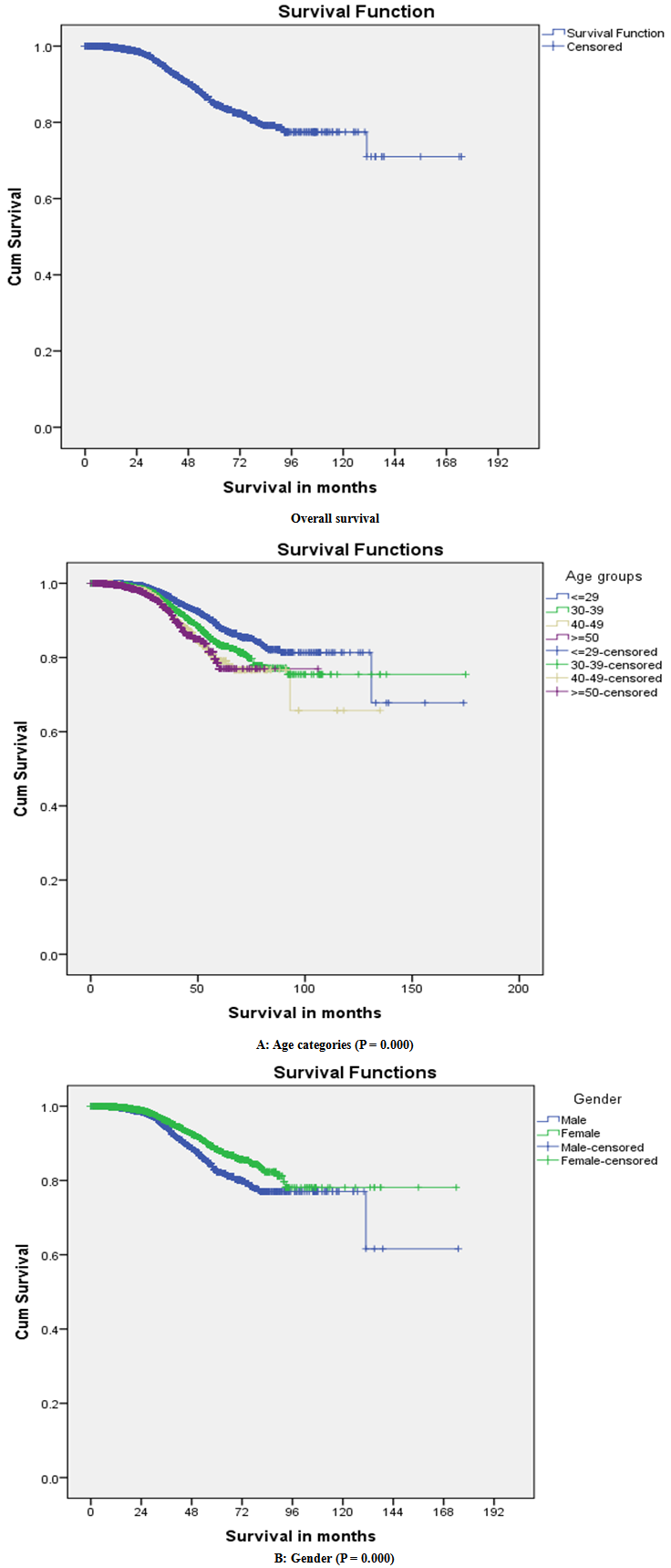 | Figure 2. Kaplan-Meier survival curves after HIV diagnosis stratified by demographic characteristics |
4. Discussion
- The present analysis is based on a retrospective cohort of HIV/AIDS patients registered at different ART centers during 2005-09 in Andhra Pradesh, India. At the end of follow-up, 84.1% of them were alive, 8.1% were dead, 4.9% were LFU and 2.9% were transferred. Sexual root (heterosexual+MSM) (98.5%) remains highest vulnerable mode of HIV transmission. Crude mortality rate of 28 per 1000 person-years which is higher than the adult mortality rate in general population. Out of the total deaths, 54.6% deaths occurred within 6 months of HIV registration. The higher mortality in the first six months estimated by this analysis corroborates the findings from several other studies[7,12,13,18]. The higher mortality in the first six months of HIV registration could be due to some other reasons like poor adherence to ART regimen combined with other co-morbid infections and low CD4 T cell count[12]. Furthermore, we found that the overall lifetime median survival time was around 12 years from the date of HIV detection and around 4.3 years from the date of ART registration with higher average survival among women as reported by others[13]. The analysis showed a strong association between survival probability and demographic variables as age, gender and education. The increasing risk of death in HIV-patients has significantly been high in higher age groups as previously reported[9,11,12,13,14,19,20,21]. This empirical analysis clearly revealed that higher mortality in older age. Therefore, survival was inversely correlated with age. This analysis also recorded the higher proportion of deaths among males (8.1%) as compared with females (5.6%). Around 4.9% in male and 4.0% in female were recorded as lost to follow up, however such differences were minimal in this study. The hazard of death among men was significantly higher than among women, as previously reported by others[12, 22,23,24]. Higher mortality among male may be due to high reporting by males or biological differences or drug response to ART[12]. However, in some studies it was not found statistically significant [9,11,19,20,21]. Mortality density increases according to delay in ART registration and it was highest with delay more than 12 months (76.1 per 1000 person-years). In case of mode of HIV transmission, it was higher in others mode (73.9 per 1000 person-years) as compared with sexual root. This empirical research provided evidence that risk of death was significantly higher in those individuals who acquired HIV infection through others (IDU/Blood transfusion/ Mother to child) root as it was a direct mode of HIV transmission. Therefore, it is obvious that the threat of mortality is high among others group. Association between levels of education among individuals, marital status with likelihood of death was found significant in the present analysis, however it was not in agreement with others[12, 13, 20]. Though plenty of research is available worldwide regarding survival of HIV/AIDS patients, however it still required further research in Indian context.The findings of the present study should be examined in light of certain limitations. The first limitation of this study was associated with its study design. We used a retrospective cohort with only demographic characteristics and hence we could not take into account all the potential confounders such as CD4 T cell count, HIV staging, viral load, co-morbid condition that could have influenced the survival of individuals. Another limitation was associated with the cause of death. We considered all cause mortality in the analysis. There is a possibility that a few of the deaths may have occurred due to causes not related to HIV/AIDS. The third limitation was related to the missing information in different covariates as well as date of death.
5. Conclusions
- Despite these study limitations, the study findings have important policy implications for ART programme in India. ART services in India are freely provided to all HIV infected persons. The higher survival rate among ART individuals suggests that country’s ART program has been successful in increasing longevity of life of HIV infected individuals. However, there are certain concerns regarding missing information in the database. Efforts are required at the management as well as at implementation level for constant and regular follow-up with all patients. In addition, the program should expand to cover more remote areas to provide services to some of the underserved population groups like women. Our study also demonstrated higher mortality among individuals within 6 months of HIV detection. This argues for the need to identify and treat eligible HIV infected individuals at an early stage. In addition, late appearance to ART centers is one of the main reasons for higher mortality in the first six months. Therefore, attention is needed to ensure early diagnosis and enrollment into ART for PLHIV’s.
ACKNOWLEDGEMENTS
- This paper was written as a part of PhD research, under GGS Indra Prastha University, New Delhi. The views expressed herein are those of the authors and do not necessarily reflect the official policy of AIDS control programme. We are thankful to the National AIDS Control Organization (NACO) for providing individual ART data of Andhra Pradesh.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML