-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2014; 4(1): 13-18
doi:10.5923/j.phr.20140401.03
Denial, Shame and Acceptance: Generating Base-line Knowledge and Understanding of Fecal Incontinence amongst Long-term Care Residents and Care Providers
D. Wayne Taylor1, Jacqueline J. Cahill2, Diaa E. E. Rizk2
1The Cameron Institute, Hamilton, Ontario L8S 4M4 Canada
2The Canadian Continence Foundation, Peterborough, Ontario K9J 2R8 Canada
Correspondence to: D. Wayne Taylor, The Cameron Institute, Hamilton, Ontario L8S 4M4 Canada.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
The study aimed to determine the prevalence and understanding of fecal incontinence amongst a sample of long-term care residents and care providers in Ontario, Canada. A pilot qualitative study was conducted of 16 patients living with fecal incontinence and 9 of their healthcare providers in 2 long term care facilities. Subjects were selected equally from both genders. Focus group discussion with study participants used both thematic and deductive approaches; sessions were audio-taped and transcribed for qualitative analysis. Amongst care providers there was a bimodal distribution in the self-reported levels of confidence and competence in dealing with fecal incontinence: some were very confident and competent in dealing with incontinence; others much less so. Although all the residents interviewed, whose average age was 79, were identified by staff as experiencing fecal incontinence, less than 1 in 5 considered themselves incontinent to feces. More than half of residents did not seek care for their fecal incontinence because of embarrassment or low expectations of what could be done; those who did seek care waited for 6 months. This pilot study stresses the importance of public education, provider training, and understanding elder denial to improve the delivery of fecal incontinence services to long-term care residents.
Keywords: Caregivers, Elderly, Fecal incontinence, Knowledge, Long term care
Cite this paper: D. Wayne Taylor, Jacqueline J. Cahill, Diaa E. E. Rizk, Denial, Shame and Acceptance: Generating Base-line Knowledge and Understanding of Fecal Incontinence amongst Long-term Care Residents and Care Providers, Public Health Research, Vol. 4 No. 1, 2014, pp. 13-18. doi: 10.5923/j.phr.20140401.03.
Article Outline
1. Introduction
- In terms of academic study, interest and understanding, fecal incontinence (FI) is the poor cousin of the incontinence twins – fecal and urinary. A rudimentary search of the electronic academic search engine, Google Scholar, identifies over 337,000 articles written about urinary incontinence (UI) compared to only 74,000 that studied FI[1]. This is a gross underrepresentation given that the prevalence rate for UI has been estimated at 28% in the non-institutionalized population overall[2]; the prevalence of FI at 18%[3]; and the prevalence of FI presenting concurrent with UI (double incontinence) at 55%[4].Although the epidemiology, and the socio-economic consequences, of UI have been well-defined in the incontinence literature, the community prevalence and adverse impact of FI remain incompletely understood. The main reason is the use of different interview questions in highly selected and hospital-based populations that has resulted in widely varying reported prevalence rates and impacts[5].In Canada, the prevalence rate of FI ranged from 2% in a community-based sample of middle-age subjects and 3% in the nulligravid secondary school female teenage population, to 8% in post-partum women following obstetrical anal sphincter injury, and 46 % amongst the elderly in long-term hospitals[5-8]. With a double incontinence rate of 44% in the latter study, the mean nursing time spent each day to deal with incontinence and the total annual cost of incontinence were 52.5 minutes and $9771 per patient, respectively[8]. Qualitative studies and epidemiological data have repeatedly shown that patients do not understand the actual meaning of the word “incontinence”, whether this is urinary or fecal, thus both conditions have been often under-reported [9-13]. According to other patient surveys several years will pass beyond onset before urinary incontinent women will present their symptoms to a physician or other health care provider and/or be referred to a specialist[9, 14-16] because they: think that the condition is not treatable; feel embarrassed; and/or think that UI is a “normal” part of ageing. Most incontinent patients in Canada are treated by their family physician. These general practitioners have reported that they are not adequately trained to provide proper care for their urinary incontinent patients; they are hesitant to discuss or manage the condition during consultation, and; they often do not arrange follow-up care including timely specialist referral[17]. Although the situation with understanding and care of FI is expected to be the same or even worse, there is limited information to guide public health policy in Canada. There is a dearth of reliable data about FI as well as studies covering the perception, knowledge and health-care seeking behavior of Canadians with FI. The “real” prevalence of this condition in the long-term care residential community is also not known.Increasingly, patient advocacy groups are playing an important role in improving health care and services through knowledge transfer, patient-focused care guidelines and government lobbying[18]. Incontinence advocacy groups like The Canadian Continence Foundation (TCCF) strive to ensure that all fecal incontinent Canadian consumers have access to evidence-based medical therapy of FI, and that their quality of life is given serious consideration by health policy makers, because FI is still a stigmatized and taboo condition amongst Canadians. As such, FI is often suffered in silence without seeking health care. One can only guess why the imbalance noted above in incontinence scholarship exists. FI is an embarrassing and debilitating symptom. To begin to remedy this situation the authors interviewed both long-term care residents and their long-term care providers as a means to establish base-line knowledge upon which to build further studies to investigate the types of information products, treatments and care guidelines required to optimize the health and quality-of-life of those afflicted with FI and/or double incontinence.This long-term care residential-based, qualitative study is important for projecting the need for more appropriate and timely health services and therapeutic intervention with respect to FI. With the ongoing efforts of patient groups, such as TCCF, in encouraging patient and family education, it is also crucial that formal long-term caregivers (physicians, nurses, personal service workers, and healthy aides) improve their understanding of patient perceptions of the condition, identify the biomedical knowledge gaps in general knowledge about FI, and recognize the potential barriers to care-seeking for FI patients. The objectives of the study were to: 1- Determine the self-reported prevalence of FI in a sample of long term care residents, both male and female; 2- Identify the meaning of the term “fecal incontinence” in this group and assess their background knowledge about the causes and treatment outcomes for FI;3- Study the patient-specific reasons for delaying or not choosing to seek FI care;4- Generate base-line knowledge of formal long term care providers with respect to FI and their experiences in FI care.
2. Materials and Methods
- A pilot qualitative study was conducted of 16 patients living with FI and 9 of their healthcare providers in 2 long term care facilities in Ontario. Subjects were selected equally from both genders (8 males and 8 females) and both facilities (n= 8 each). The caregiver was identified by the patient as the staff member primarily responsible for his/her care. Fecal incontinence was defined as involuntary loss of liquid or solid stools only, and not of flatus. Patients with significant cognitive impairment were excluded. The nursing manager in each facility recruited study subjects consecutively according to the inclusion criteria. Focus group discussion with study participants used both thematic and deductive approaches as an integrated template for the interview. The sessions were audio-taped and transcribed for qualitative analysis. All data were kept anonymous and confidential. Subjects gave informed consent to participate and the research ethics committee of the Peterborough Regional Health Centre approved the study. The focus group discussions were conducted in the offices of the participating long term care facilities. The study was conducted over an 8 week period from March-April 2013.Data were collected by two investigators[JJC & DEER] using a structured interview questionnaire. For patients with FI, this consisted of 30 items that included a number of demographic, reproductive, medical and lifestyle variables with closed and open responses. Parity amongst women was the number of previous pregnancies delivered after 7 months. The study definition of FI was any self-reported episode of involuntary solid or liquid fecal leakage within the previous 12 months. The patient-specific questions were generated from responses to a previous study conducted by The Cameron Institute and the TCCF which assessed women’s knowledge about UI and their attitude to care-seeking[19]. For care providers, the questionnaire measured the confidence and competence levels to deal with FI on a 10-point Likert-type scale in which 10=extremely and 0=not at all. On a 5-point Likert-type scale, providers were also asked to rate their current knowledge and training (at the time of being interviewed) to deal with residents with FI with 1=strongly disagree and 5=strongly agree.Copies of the patient and provider questionnaires are available from the authors on request.
3. Results
3.1. Personal Data
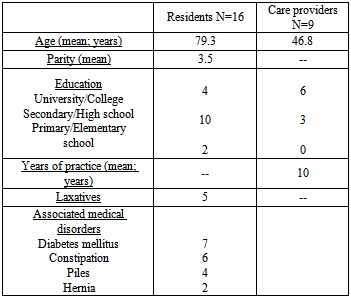
3.1.1. Residents
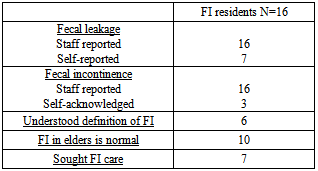
- The average age of long term care resident interviewed was 79.3 with a range of ages 30-94. All had completed high school except 2; 4 had a university education. Parity for women ranged 0-7 with a mean of 3.5. None had diabetes, a hernia, constipation or piles – the most common co-morbidities associated with FI – but 5 did take laxatives presumably negating constipation. Of the 16 residents, 7 self-reported experiencing fecal leakage, even though all had been identified as fecally incontinent by staff before the commencement of the study. With respect to FI “being a bother”: 1 reported “not at all”, 2 “somewhat”, and 1 “a lot”. Only 3 residents reported experiencing an abnormally strong feeling of urgency to de- fecate; the same 3 reported experiencing fecal leakage associated with the feeling of urgency. Two reported experiencing moderate difficulty or discomfort in passing stools, and both of these residents were on laxatives.
3.1.2. Care Providers
- The age of the long term care providers that were interviewed ranged 32-57 with an average age of 46.8 years, all of whom were female. All were formally educated and qualified personal service workers (PSWs) except 1 who was a nursing student; 1 of the PSWs was also a foreign trained registered nurse. Their years of practice varied from less than 1 year to 21 years with an average of 10 years.
|
3.2. Resident Knowledge about Incontinence - Denial
- Of the 16 residents interviewed, 6 did not know what incontinence or FI meant whereas another 6 did, although often expressed colloquially. (This was low given the response re defining UI in other research[19].) Others thought it was constipation or an urgency to void. Most considered an excessive amount of involuntary leakage was required to be FI but did not really have an opinion what frequency of involuntary leakage determined FI. Of particular interest was the answer to the question: “do you consider yourself incontinent to feces? Only 3 residents did even though 7 had reported fecal leakage and all 16 had been identified as FI by residence staff. With respect to the age of FI onset, 7 residents thought of it as a condition of “old age”, 1 realized that it could strike at any age, and the rest were not sure. None of the residents had a clear idea of what caused FI (blaming the laxatives they were administered, going to bed early) nor did they have any knowledge of preventive measures that could be taken. Of the 16 residents studied, 10 thought that FI in older people was normal and 9 thought it could be improved and/or cured.
3.3. Resident Attitude to FI Care Seeking – Shame and Acceptance
- FI care was not something that all long term care residents sought – only 7 had done so, and then after waiting as long as 6 months to do so, with all of then seeking help from their family physician. The most common reasons given for this avoidance behavior were: a low expectation from medical staff because there was nothing to be done (5); shame (4); and, that FI was just normal at their age (2).
|
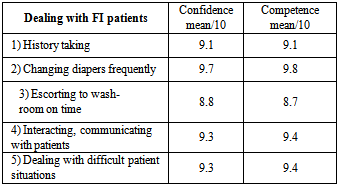
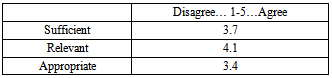
3.4. Care Provider Self-reported Confidence, Competence, Knowledge and Training
- Amongst care providers there was a bimodal distribution in the self-reported levels of confidence and competence in dealing with FI: some felt that they were very confident and competent in dealing with FI; other providers much less so (see Table 3). The 2 care providers with nursing training and the oldest PSW self-scored quite low (3,5,7) on some of the variables in Table 3 whereas the others were almost always consistently scoring themselves as 9 or 10.
|
|
3.5. Caregiver Needs and Suggestions
- When asked what were the most important needs that they had in dealing confidently with FI patients the long term care providers that were interviewed for this study responded with the following (multiple responses):• Respect for and dignity of patient (6)• Patient privacy (4)• Better absorbent products with liners (4)• Education on the causes of FI (2)• Protective provider clothing • Night size product • Proper fitting gloves • Switching products without physician orders • Good team work• Patience• Frequent monitoring of patientsAs a terminal, open-ended question care providers were asked what suggestions they may have on how to improve the long-term care of FI in Ontario (multiple responses):§ Increase staffing levels to 1:7 patients (3)§ Patient education about FI to reduce patient stress (2)§ More hands-on training at the college level (2)§ More resident-centred care (2)§ Better washroom signage§ Family education about FI§ Increase care hours per patient from 2.2 to 3.5 hours/day§ Management listen to staff§ Permanent staff-patient pairing to improve staff knowledge of patients§ Reduce use of laxatives
4. Discussion
- This survey has generated based-line data from a Canadian long term care residential population perspective which supplements the scant literature on the epidemiology and social awareness of FI. Although all the residents interviewed in long-term care, whose average age was 79, had been identified by staff as experiencing FI, less than 1 in 5 considered themselves incontinent to feces and self-reported having FI. Most residents thought that FI was a normal part of aging and had no idea what caused it or how to prevent it. More than half of residents did not seek care for their FI because of embarrassment or low expectations of what could be done; those who did seek care waited for 6 months. Most of those who self-reported that they were incontinent to feces believed that their FI had been caused by the food and the laxatives they received. Patients’ knowledge regarding FI and their health care seeking behavior in our study, therefore, are not different from those reported elsewhere[4, 6, 15].Many respondents were unsure about the definition, causes or treatment outcome of FI and yet aware of the adverse effects. This finding underscores the importance of promotion of public awareness about FI, as well as the more formal education and training of long term care providers, the knowledge component part of which can be shared with residents and their.As in a previous study[19] a disappointing finding families[11].was that some patients in the study believed that FI was a normal part of aging. The knowledge barrier to seeking timely help for FI emphasizes the responsibility of long term care providers as key informants to correct patient misconceptions. The contribution of chronic constipation to the prevalence of FI was expected because this is a potential risk factor although the mechanism for incontinence remains obscure[20]. It has been suggested that excessive expulsive efforts during defecation causes perineal descent that leads to traction on the pudendal nerves at their relatively fixed point of exit from Alcock’s canal and progressive pudendal de-nervation and subsequent ineffective re-innervation and in turn FI in later years. In addition, fecal impaction may cause decreased anal sensation in constipated patients which leads to difficulty in contracting the external sphincter appropriately to prevent leakage when the internal sphincter normally relaxes in response to rectal distension. On the other hand, long-standing FI may cause chronic constipation because patients tend to avoid eating or use a constipating diet or treatment in an attempt to improve FI. It was unclear when the onset of FI occurred in this sample population; research into whether or not FI first presents after admission to long-term care would be beneficial. The association of FI and UI - double incontinence - in the elderly population, as seen in our study, is well known and can be explained by the same underlying risk factors[4, 8, 15].Long term care providers interviewed generally felt confident and competent in caring for residents with FI but wished that more on-hands training had been given them both in college and on-the-job. Providers also did not think that the environment for resident FI care was all that it could be in terms of being respectful and dignified for the patient. An in-service training module for FI would be welcomed.The cost of managing FI in residential long term facilities was unknown at the time of this study. We plan to investigate this topic further as the financial burden of FI in institutionalized patients is expected to be considerable similar to UI[6]. The economic factor is important in planning the need for health services and in deciding on the care priorities of the fecal incontinent population.Surveys are subject to sampling, detection and response biases. Results cannot be generalized to the entire long term care residential population of Canada given the study’s sample size, which was limited by available funding. Our data collection technique of personal interviews contains less detection bias of the presence and self-reporting of FI than standard epidemiological studies based on telephone surveys, mailed questionnaires or medical chart review since most patients with FI do not report this symptom[3]. Our definition of FI was based on the assumption that it would detect stool incontinence of a frequency or a severity to be an important problem to the individual concerned because any involuntary loss of faeces is abnormal[20]. This definition is also easy to use because it is comprehensible to the target population[3]. Response bias was minimized in our cohort because the interviewer approached both residents and providers as an independent researcher and not as a service provider or residential administrator. Study results, however, can be used as a base-line for a province-wide or nationwide study.
5. Conclusions
- This pilot study stresses the importance of public education, provider training and health planning to improve the delivery of FI services to long-term residents in Canada. Larger province-based studies should be conducted to further examine these issues.Given that over 80% of those residents who were incontinent to feces did not think of themselves as being incontinent, studies should be conducted to understand the underpinnings of this denial to better able residents, care providers and families of residents to communicate and problem solve around the care needs of the elderly with FI.
ACKNOWLEDGEMENTS
- The study was funded by an unconditional research grant from SCA Americas, Personal Care, Canada; thank you to the management and staff of Schlegel Villages for their support and participation in this study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML