-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2014; 4(1): 7-12
doi:10.5923/j.phr.20140401.02
Investigation of Cholera Outbreak in an Urban North Central Nigerian Community-The Akwanga Experience
Akyala Ishaku A.1, 2, Bright Esyine Shadrack1, Olufemi Ajumobi1, Adebola Olayinka1, Patrick Nguku1
1Nigeria Field Laboratory Epidemiology Training Program, Abuja- Nigeria
2Microbiology Unit, Department of Biological Sciences, Nasarawa State University, Keffi, Nigeria
Correspondence to: Akyala Ishaku A., Nigeria Field Laboratory Epidemiology Training Program, Abuja- Nigeria.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Introduction. Diarrheal disease outbreaks are cause of major Public health emergencies in Nigeria. From September 12th to 14th, 2013 an outbreak of cholera began among a sub-urban area of Akwanga L.G.A of Nasarawa State, North Central. We investigate to verify diagnosis, identify risk factors and recommend control measures. Method. We conducted a descriptive description, active case search and un-matched case control study. Cholera case-patent was a person with acute watery diarrhea, with or without vomiting in Akwanga from 12th to 13 September 2013, stool from case patients and water samples were taken for laboratory analysis. We performed Univariate and bivariate analysis using Epi-Info version 3.3. Results.Out of 18 cases patients, 10(55.6%) were male while 8(44.4% were female, of which 40% are from a sub-urban community of Kurmi tagwaye attack rate was 2/1000 population with two case fatality. Age ranged from 1-84 years: mean (34+18) years, age group of 20-29 years were mostly affected vibrio cholera serotype Ogawa was isolated from stool. The main water source, Rafin Kumin Tagwaye River was polluted by resident defecation, post-defecation bath and car washing compared to controls, case patients were likely to have drank from Kumin Tagwaye rivers (OR 4.56, 95% CL.2.75-18). Conclusion. Vibrio cholera sero-type ogawa caused the Akwanga cholera outbreak affecting many young adult males; drinking water from contaminated community Wide River was the major risk factor. Boiling or chlorinating the water was initiated based on our recommendation and this controlled the outbreak.
Keywords: Cholera Akwanga Water Sero Types
Cite this paper: Akyala Ishaku A., Bright Esyine Shadrack, Olufemi Ajumobi, Adebola Olayinka, Patrick Nguku, Investigation of Cholera Outbreak in an Urban North Central Nigerian Community-The Akwanga Experience, Public Health Research, Vol. 4 No. 1, 2014, pp. 7-12. doi: 10.5923/j.phr.20140401.02.
Article Outline
1. Introduction
- Cholera caused by Vibrio cholera continues to be a global threat to public health and a key indicator of lack of social development. Once common throughout the world, the infection is now largely confined to developing countries in the tropics and subtropics. It is endemic in Africa, parts of Asia, the Middle East, and South and Central America. In endemic areas, outbreaks usually occur when war or civil unrest disrupts public sanitation services. Natural disasters like earthquake, tsunami, volcanic eruptions, landslides and floods also contribute to outbreak by disrupting the normal balance of nature[1]. This creates many health problems, food and water supplies can become contaminated by parasites and bacteria when essential systems like those for water and sewage are destroyed. Developing countries are disproportionately affected because of their lack of resources, infrastructure and disaster preparedness systems. In newly affected areas, outbreaks may occur during any season and affect all ages equally. The organism normally lives in aquatic environments along the coast. People acquire its infection by consuming contaminated water, seafood, or other foods. Once infected, they excrete the bacteria in stool. Thus, the infection can spread rapidly, particularly in areas where human waste is untreated.In Nigeria, the infection is endemic and outbreaks are not unusual. In the last quarter of 2009, it was speculated that more than 260 people died of cholera in four Northern states with over 96 people in Maiduguri, Biu, Gwoza, Dikwa and Jere council areas of Bauchi state[4]. Most of the Northern states of Nigeria rely on hand dug wells and contaminated ponds as source of drinking water. Usually, the source of the contamination is other cholera patients when their untreated diarrhoea discharge is allowed to get into water supplies. The 2010 outbreak of cholera and gastroenteritis and the attendant deaths in some regions in Nigeria brought to the forefront the vulnerability of poor communities and most especially children to the infection. The outbreak was attributed to rain which washed sewage into open wells and ponds, where people obtain water for drinking and household needs. The regions ravaged by the scourge include Jigawa, Bauchi, Gombe, Yobe, Borno, Adamawa, Taraba, FCT, Cross River, Kaduna, Osun and Rivers, depicts major outbreak locations. Even though the epidemic was recorded in these areas, epidemiological evidence indicated that the entire country was at risk, with the postulation that the outbreak was due to hyper-virulent strains of the organism. In Nigeria, the first series of cholera outbreak was reported between 1970-1990[6]. Despite this long experience with cholera, an understanding of the epidemiology of the disease aiding its persistence in outbreak situations is still lacking. This review therefore provides the knowledge gaps of the infection with the hope that it will help to develop targeted approaches to controlling the infection.
2. Methods
2.1. Study Area
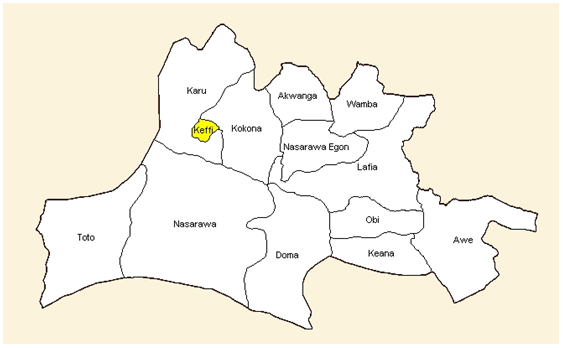 The outbreak L.G.A of Nassarawa State, 58 km from the state capital in Northern senatorial district. There is a General Hospital one primary health Centre (PHC), two faith base organization hospital, and 20 private health centers. The main economic activities in the municipality are farming, petty trading, and fishing. The L.G.A experience two main seasons as typical in other places. The Rafin Kurmi Tagwaye River with its tributaries services as a major source of drinking for most sub-urban area of kurmi tagwaye. The vegetation of the area is forest with traces of savannah in the North Eastern part of the country. The outbreak was mainly centered on kurmin tagwaye in Akwanga L.G.A, which is populated with 2,600 people with individuals engaged in economic activities in both the formal and informal sectors. STUDY DESIGNWe interviewed the state disease notification officer (SDNO) and the local government disease notification officer, the public health nurse the Hospital Management teams, the Environmental Health Officer and the Chief Executive to obtain information on the outbreak and preliminary data on those affected. We reviewed the surveillance data and the initial line-list generated by the DNSO.Based on the information we gathered, we defined a cholera patient case as a person having acute diarrhea (watery) with or without vomiting. We also defined cholera case-patient as a person with vibrio cholera isolated from stool sample or epidemiologically or kurmin tagwaye between 12th to 14th September 2013. We then reviewed medical records from all health facilities in General Hospital Akwanga and primary health care center, Akwanga. In order to meet up with the case definition. Further review was conducted at three other health facilities. Data extracted were age, sex, occupation, place of resident, date of onset, date of presentation at health facility, Signs and symptoms and outcome. Active case search and community interview to trace other case and contact.CASE-CONTROL STUDYWe conducted un-matched case control study in the municipality using the entire Kurmin tagwaye as study population. Based on sample size formula for comparing proportion as embedded in the “stalcalc” utility feature of epi-info statistical software, we used a confidence level of 95% Power of 80%, expected exposure frequency in cases of 50%, case to control ratio of 1:2 and an odds ratio of 4 (for a risk factors on which intervention would have a significant impact to a minimum sample size of 18 cases and 36 control were obtained.Case definition was applied and control was defined as persons living in the same community with case patient but who did not have acute watery stool during the same period. Case finding was done through the L.G.A LNSO data based of cholera cases derived from patients’ information and case search provided by patients evaluated at the two hospitals, clinics and communities. These records captured demographic information including; name, gender, date of birth, place of birth, clinical status, therapeutic status, result of therapy, V cholera serotype and health system status. Two controls were selected for each case by location of resident within the community. The control was found each case by a member of investigation team standing in front of the case’s house and spinning a bottle to determine a starting direction. Next, a number between two and five was drawn at random to indicate the number of houses in the chosen direction to proceed before attempting to interview the first control. This method was chosen because of the absence of a sampling frame. (Street address, post code etc.).The study was explained to the house-hold by the field workers and if they agreed to participate, workers selected two of the available house-hold member without diarrhea and vomiting by simple number drawn and interviewed the individuals as control for the study. In case of refusal, the field workers repeated the bottle spinning procedure to select another house-hold. Individuals were excluded from being control if they reported suffering from watery diarrhea since 12th Sept, 2013.Copies of a standardized questionnaire, written in English were administered to cases and control in their native hausa tongue by bilingual and multi-lingual trained interviewers state management team. The questionnaire collected basic demographics information and containing questions pertaining food and water exposures and hygiene practices from 12th to interview date, in cases where a child was the study subject, question were directed to his guardian within the household (typically a family member) who had knowledge of the child’s activities.LABORATORY INVESTIGATIONS We collected stool and water samples from the case-patient and sent to the National Public Health Laboratory at Lagos for primary microbiological assessments. The investigation were done by the laboratory staff of the hospital with support of the research filed track resident of NFELTP stool was either directly plated of thiosulfate-citrate bile salt agar (TCBS) or transported on carry blair transport media and plated on TC BS agar. Colonies and vibrio positive isolates were serogroup and serotyped using agglutination test with commercial anti-sera.ENVIRONMENTAL SURVEYAn environmental survey of house-hold of cases and control was undertaken. We expected their source of water supply principally observing activities around the kurmin tagwanye river, the drainage system, sewage line, general sanitation along water bodies and collected water specimen and sent them for water quality testinh at the state lab.ETHICAL ISSUES: Informed consent and permission was sought from the participants before the interviews, we protected the confidentiality of the participants through use of codes. However, ethical committee review did not apply as this was a public health response to an outbreak. Preliminary report of the outbreak was been discussed by the local disease notification officer and elders of the community affected.
The outbreak L.G.A of Nassarawa State, 58 km from the state capital in Northern senatorial district. There is a General Hospital one primary health Centre (PHC), two faith base organization hospital, and 20 private health centers. The main economic activities in the municipality are farming, petty trading, and fishing. The L.G.A experience two main seasons as typical in other places. The Rafin Kurmi Tagwaye River with its tributaries services as a major source of drinking for most sub-urban area of kurmi tagwaye. The vegetation of the area is forest with traces of savannah in the North Eastern part of the country. The outbreak was mainly centered on kurmin tagwaye in Akwanga L.G.A, which is populated with 2,600 people with individuals engaged in economic activities in both the formal and informal sectors. STUDY DESIGNWe interviewed the state disease notification officer (SDNO) and the local government disease notification officer, the public health nurse the Hospital Management teams, the Environmental Health Officer and the Chief Executive to obtain information on the outbreak and preliminary data on those affected. We reviewed the surveillance data and the initial line-list generated by the DNSO.Based on the information we gathered, we defined a cholera patient case as a person having acute diarrhea (watery) with or without vomiting. We also defined cholera case-patient as a person with vibrio cholera isolated from stool sample or epidemiologically or kurmin tagwaye between 12th to 14th September 2013. We then reviewed medical records from all health facilities in General Hospital Akwanga and primary health care center, Akwanga. In order to meet up with the case definition. Further review was conducted at three other health facilities. Data extracted were age, sex, occupation, place of resident, date of onset, date of presentation at health facility, Signs and symptoms and outcome. Active case search and community interview to trace other case and contact.CASE-CONTROL STUDYWe conducted un-matched case control study in the municipality using the entire Kurmin tagwaye as study population. Based on sample size formula for comparing proportion as embedded in the “stalcalc” utility feature of epi-info statistical software, we used a confidence level of 95% Power of 80%, expected exposure frequency in cases of 50%, case to control ratio of 1:2 and an odds ratio of 4 (for a risk factors on which intervention would have a significant impact to a minimum sample size of 18 cases and 36 control were obtained.Case definition was applied and control was defined as persons living in the same community with case patient but who did not have acute watery stool during the same period. Case finding was done through the L.G.A LNSO data based of cholera cases derived from patients’ information and case search provided by patients evaluated at the two hospitals, clinics and communities. These records captured demographic information including; name, gender, date of birth, place of birth, clinical status, therapeutic status, result of therapy, V cholera serotype and health system status. Two controls were selected for each case by location of resident within the community. The control was found each case by a member of investigation team standing in front of the case’s house and spinning a bottle to determine a starting direction. Next, a number between two and five was drawn at random to indicate the number of houses in the chosen direction to proceed before attempting to interview the first control. This method was chosen because of the absence of a sampling frame. (Street address, post code etc.).The study was explained to the house-hold by the field workers and if they agreed to participate, workers selected two of the available house-hold member without diarrhea and vomiting by simple number drawn and interviewed the individuals as control for the study. In case of refusal, the field workers repeated the bottle spinning procedure to select another house-hold. Individuals were excluded from being control if they reported suffering from watery diarrhea since 12th Sept, 2013.Copies of a standardized questionnaire, written in English were administered to cases and control in their native hausa tongue by bilingual and multi-lingual trained interviewers state management team. The questionnaire collected basic demographics information and containing questions pertaining food and water exposures and hygiene practices from 12th to interview date, in cases where a child was the study subject, question were directed to his guardian within the household (typically a family member) who had knowledge of the child’s activities.LABORATORY INVESTIGATIONS We collected stool and water samples from the case-patient and sent to the National Public Health Laboratory at Lagos for primary microbiological assessments. The investigation were done by the laboratory staff of the hospital with support of the research filed track resident of NFELTP stool was either directly plated of thiosulfate-citrate bile salt agar (TCBS) or transported on carry blair transport media and plated on TC BS agar. Colonies and vibrio positive isolates were serogroup and serotyped using agglutination test with commercial anti-sera.ENVIRONMENTAL SURVEYAn environmental survey of house-hold of cases and control was undertaken. We expected their source of water supply principally observing activities around the kurmin tagwanye river, the drainage system, sewage line, general sanitation along water bodies and collected water specimen and sent them for water quality testinh at the state lab.ETHICAL ISSUES: Informed consent and permission was sought from the participants before the interviews, we protected the confidentiality of the participants through use of codes. However, ethical committee review did not apply as this was a public health response to an outbreak. Preliminary report of the outbreak was been discussed by the local disease notification officer and elders of the community affected.2.2. Data Analysis
- Data were entered into Epi-Info software version 3.3 for data cleaning and analysis. We performed descriptive analysis of outbreak data by person, place and time. Univariate analysis were expressed as frequency distribution, percentages, mean I standard deviation and rates (attack rate, case-facility rate etc. as appropriate. Inferential analysis of the case control study data, we dichotomized qualitative exposure-variables and compare them among case patients versus control into bivariate analysis to identify potential risk factors using chi-square test at 95% confidence level or alpha level of 5%. an exposure was consider a risk factor if the odds of association with cholera-case status at 95% confidence interval was statistically significant base on a P-value of 0.05.
3. Results
- DESCRIPTION OF CHOLERA BY PLACEMost of the affected cases were founded in the kurmin tagwaye sub-urban area of Akwanga L.G.A Nasarawa State. The others were scattered in other area eleven cases (61.1%) were found at kurmin tagwaye while seven cases (38.2 ) were found at angwan Tiv.
3.1. Analytical Studies
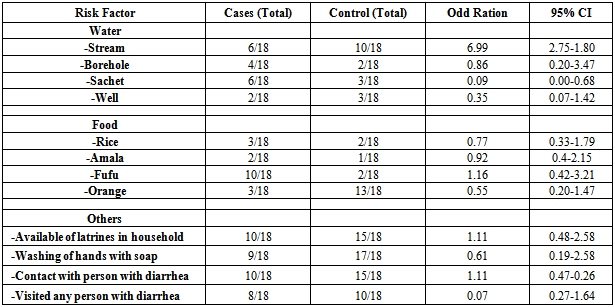
- We recruited 36 participants for the case-control study, of which 18 were cases and 18 were controls giving a case to control ratio of 1:1. The mean ages for cases were 24 ±3 years and controls 30±2 years. The age range among the cases was 6-84 years and that of the control 10-70years. Majority of the cases were females of cases. Those who developed cholera were times as likely to have dunk from the river and streams as compared to those who did not develop the disease (OR=6.99 95% CI:2.75-18).
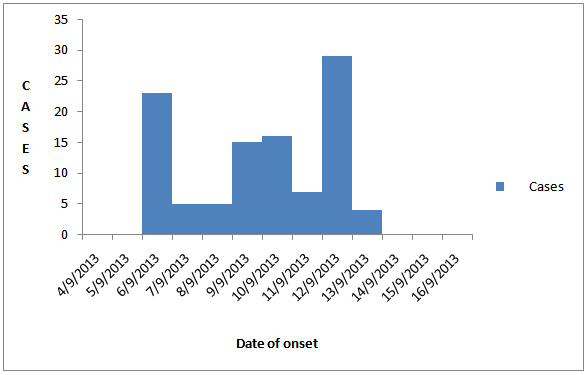 | Figure 1. Epi-Curve of Cholera Outbreak in Akwanga L.G.A of Nasarawa State |
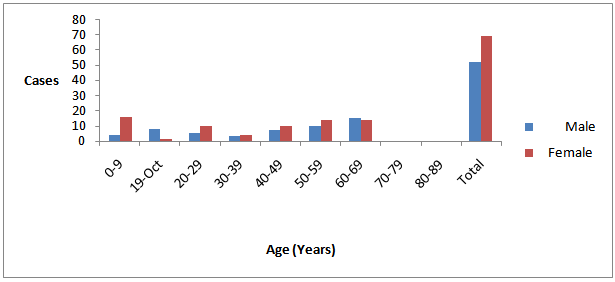 | Figure 2. Distribution of Cholera cases by Gender and Age in Akwanga L.G.A of Nasarawa State |
|
4. Discussion
- Cholera is a disease of history that remains a major public health problem in many parts of Africa, with Nigeria inclusive. It’s common among poor people and vulnerable communities that lack good portable water despite public health awareness, health promotion, detailed understanding of the bacteriology, and epidemiology and public health aspect for more than a century.o The study revealed that, the cholera epidemic affects all age groups in the L.G.A, mostly young adult females probably due to their involvement with water for domestic activities which exposed them to the index case through direct contact or sharing contaminated water source.o This observation could be due to the facts that some of the females were food vendors at the river sites, traditionally; females are more involved in fetching water for domestic use from the local stream which could expose them further to the infection. House-hold contact could be an underlying factor for community wide transmission of this outbreak.o Epidemiological and environmental evidence indicates that this outbreak was water-borne. Water borne cholera is common worldwide (5). The Millennium Development Goal (MDG) proposes to decrease by half population without access to safe water and sanitation by 2015. (11) While MDG consider piped water as improved water source of transmission of waterborne pallogens may occur when the pipes and not periodically maintained or are absent.o We observed pollution of the Kurmin Kagwaye River with defecation by car washers also most people use shallow latrine due to high water tables. Environmental unsanitary conditions, densely populated and large slum population are known to facilitate cholera outbreak. The reproduction of cholera in a community is defined by social and environmental factors. The importance of the aquatic reservoir depends on the sanitary condition of the community. Cholera appears in a community, it’s essential to ensure three things namely: hygienic disposal of human feaces, an adequate water supply of safe drinking water and good food hygiene. The most useful measure in preventing the spread of cholera is the provision of safe drinking water and sanitary disposal of human waste (1). Whereas at rsik areas of cholera outbreak include urban slums and camp of internally displaced people or refugees. Out investigation revealed that certain occupational group like small-scale car was business, mai-ruwa (water) sellers where minimum requirement of clean water and sanitation are not met may also facilitate the transmission of the diseases. The limitation of these studies is a rapid flow of the kurmin Tagwaye Rivers and the timing of water sample collection as well as probably technical deficiencies might have led to the non-isolation of vibrio cholera or other known microbial causes of watery diarrhea from water samples sent to the laboratory.Social economic status and differences in age groups as confounder in the un-matched cast control study could influence the association found. Despite these limitations, the study provided useful information that will informed stakeholders actions in controlling the outbreak and to avert similar future outbreak by ensuring the provision of portable water and proper sanitary environmental condition among population in this and other communities in Akwanga L.G.A of Nasarawa State.
5. Conclusions
- An outbreak of Ogawa serotype of cholera was isolated at Akwanga L.G.A of Nasarawa State with 2 case fatality was established. It was an intermittent common. Source outbreak and affected mostly persons ages 20-29years. We established that drinking water from kurmin tagwaye stream was the major outbreak. Boiling and chlorination of water was initiated base on our recommendation and this controlled the outbreak.
ACKNOWLEDGEMENTS
- I wish to thank all the medical team from Nasarawa state ministry of health and Nigeria Field Epidemiology Laboratory training program for sponsoring the study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML