-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2013; 3(5): 130-135
doi:10.5923/j.phr.20130305.04
Determinants of Defaulting from Antiretroviral Therapy Treatment in Nekemte Hospital, Eastern Wollega Zone, Western Ethiopia
Tesfaye Asefa1, Mohammed Taha2, Tariku Dejene2, Lamessa Dube2
1Nekemte Hospital
2Jimma University, college of Public Health and medical sciences Department of Epidemiology
Correspondence to: Lamessa Dube, Jimma University, college of Public Health and medical sciences Department of Epidemiology.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
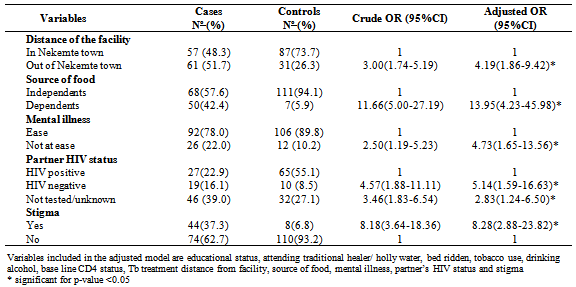
Background: The prognosis of patients with HIV in Sub-Africa has improved with the widespread use of antiretroviral therapy. Despite this success, defaulting from antiretroviral therapy is one of the major challenges in resource-limited settings. There are limited data on determinants of defaulting from antiretroviral therapy in Ethiopia. Therefore the aim of this study is to assess determinants of defaulting from antiretroviral treatment in Nekemte Hospital, West Ethiopia. Method:A case control study was used. The study covered 118 cases and 118 controls. Cases were individuals who had missed two or more clinical appointments (i.e. had not been seen for the last 2 months); controls were individuals who were rated as excellent adherers by the providers. Data were collected from patient records, and by telephone call and home visit to identify the factors associated with for defaulting. The logistic regression model was fitted by using back ward elimination technique to identify independent predictors of antiretroviral treatment defaulting.Result: After controlling for possible confounders, living far from the facility (out of the town) (AOR=4.1; 95%CI 1.86 to 9.42), dependent patients for source of food[AOR=13.9; 95%CI 4.23 to 45.99], patients with mental status not at ease[AOR=4.7; 95%CI 1.65 to 13.35], patients whose partners were HIV negative[AOR=5.1; 95%CI 1.59 to 16.63], patients whose partners HIV status were unknown or not tested[AOR=2.8; 95%CI 1.23 to 6.50] and patients that fear stigma[AOR=8.3; 95%CI 2.88 to 23.83] were statistically significant association.Conclusion: In this study, those who were living out of the town or far from the facility, whose partner’s HIV status was negative or unknown, who were stigmatized and mental ill had a higher chance of defaulting from ART treatment. So, efforts to reduce defualting from ART should focus on addressing these risk factors.
Keywords: Defaulting, Antiretroviral Treatment, Nekemte Hospital
Cite this paper: Tesfaye Asefa, Mohammed Taha, Tariku Dejene, Lamessa Dube, Determinants of Defaulting from Antiretroviral Therapy Treatment in Nekemte Hospital, Eastern Wollega Zone, Western Ethiopia, Public Health Research, Vol. 3 No. 5, 2013, pp. 130-135. doi: 10.5923/j.phr.20130305.04.
Article Outline
1. Introduction
- Sub-Saharan Africa remains the region most heavily affected by HIV, and accounted for 68% of all people living with the virus and for 72% of AIDS deaths in 2009[1]. The HIV/AIDS epidemic in Ethiopia continues to pose a threat to the lives of people. It is estimated that 977,394 people live with the virus resulting in 71,902 HIV related deaths in 2007. The national prevalence of HIV in 2007 is estimated to be 2.1%[2]. Provision of Antiretroviral Therapy (ART) has reduced mortality and also improved the quality of life of people living with HIV and AIDS (PLWHA)[3]. In 2009 alone, 1.2 million people received ART for the first time worldwide[1]. By the end of 2009, there were more than five million people on ART in middle and low income countries. In Sub-Saharan Africa, nearly 37% of people eligible for treatment were able to access ART in 2009[1]. In Ethiopia provision of ART was started in 2003. At the end of June 2008, there were only 110,611 patients (75%) who were alive and on ART out of the 150,136 patients who had been started ART since 2003[4]. Despite this success, poor adherence to ART and defaulting from ART are two major challenges in resource- limited settings[5]. Defaulting reduces the immunological benefit of ART and increases AIDS related morbidity, mortality and hospitalizations[6]. Poor adherence and defaulting from ART treatment increase the risk of drug resistance and treatment failure[5, 7- 8]. A systematic review of 33 patient cohorts from 13 African countries reported that only between 46% and 85% of patients remained in care at 2 years[9]. Studies done in Ethiopia and South Africa had reported, the overall rate of defaulting treatment were 13.6% and 12.8/100 person years respectively[5, 10].Different studies reported that defaulting from ART are influenced by distance from facility[10--16], transportation cost[12, 14, 16], drug abuse[10, 17], being bed redden[10], having HIV negative partner[10], depression[18], stigma[16, 18-20], CD4 count[16], food insecurity[21], adherence support services and food rations at HIV care clinics[22].Previous studies conducted in Ethiopia addressed adherence to ART and associated factors. However, the broader aspects of defaulter and associated factors were not well studied in Ethiopia especially in the zonal hospital. There is only one study that is conducted on this issue and it was conducted in tertiary hospital[10]. Thus this is the first by its kind in zonal hospital in Ethiopia. Besides, the defaulter rate in Nekemte hospital was 21.7% which was the highest (from 2837 ever started 616 patients were defaulters) when compared with the study on Jimma specialized hospital(13.6%)[10]. Therefore the aim of this study was to assess determinants of defaulting from antiretroviral therapy in Nekemte Hospital, West Ethiopia.
2. Methods and Materials
- A case control study was conducted in Nekemte Hospital from March 2011 to April 2011. Nekemte town is located 331 Kilometers West of Addis Ababa, the capital city of Ethiopia. Cases were ART treatment defaulters. ART treatment defaulters in this study are defined as an HIV positive patient who had been on ART treatment and missed two or more monthly clinical appointments[10], and age 15 years and above. Controls were individuals who had been on ART at least for one year and were rated as excellent adherers by the providers[10] and age 15 years and above. For each case, a control that was enrolled in the same month was selected. If more than one control enrolled in the same month, the closest date of enrolment determined selection. Patients attend the ART clinic each month to refill the ART drugs.The sample size was calculated using Epi-info version 6.0.4 software. As estimated from study done in Jimma, proportion of patients living far (distance) from the facility among the cases and controls being 44.1% and 26.0% respectively[10]. At 95% CI and 80% power and case to control 1:1, the total sample size required were 238 (119 cases and 119 controls). The hospital record was used as sampling frame. An electronic pharmacy record was used to generate lists of patients who have failed to pick up medication (defaulters). From lists of defaulter, 119 patients (cases) were randomly selected from the eligible. Using semi-structured questionnaires (a case note extraction), socio-demographic and behavioral information, and clinical factors that could potentially be associated with defaulting (which were recorded at the time treatment started) were retrieved from patient records and cards. The patient card and other forms included questions on socio-demographic information, past medical status, mental health status, and concerns for adherence. The retrieval was conducted by a data clerk in the hospital. Data were also gathered on telephone calls through their addresses recorded at the beginning of ART where possible. In occasions where telephone interview was not feasible five trained peer counselors were used to trace and interview defaulters at home. The interview was conducted at hospital for controls during follow-up visit. The questionnaire was first prepared in English language, then translated to a local language and retranslated to English to check for consistency. Data collectors and supervisors were trained for two day on the methods, objectives and data collection tool before the data collection. Data were entered, processed and analyzed using SPSS software version 16. Data analysis was started by describing each variables involved. Bivariate analysis was done for each explanatory variable separately; to identify those associated to ART treatment defaulting. Variables with p-value less than 0.20 in the bivariate analysis were considered as candidate to be entered in the multivariable logistic regression model. The logistic regression model was fitted by using back ward elimination technique. Log likelihood ratio test was used to assess the goodness of fitness of the final model.The ethical clearance was obtained from Jimma University. Written informed consent was also obtained from each respondent.
3. Result
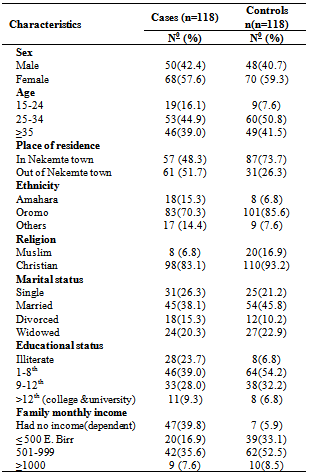
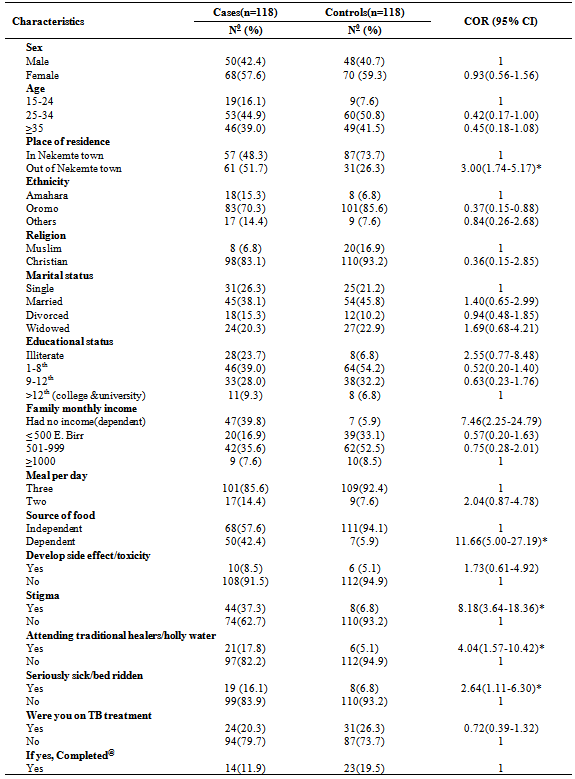
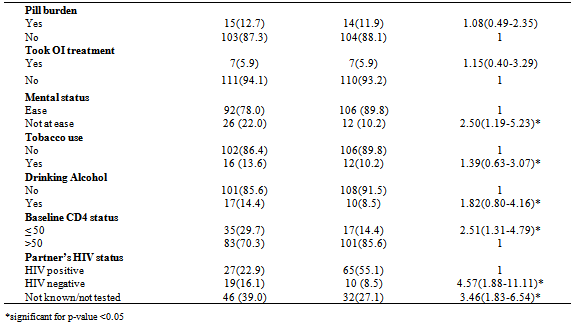
|
|
|
|
4. Discussion
- This study intended to identify the determinants of defaulting from ART treatment. The study used analytic case control design. However, it might have some limitation such as: first, recall bias on some risk factors like drug side effect, toxicity and stigma. Second, distance from health facility was assessed by living in Nekemte town or outside the town, it would have been better in kilometers or hours it take to reach the facility. Distance in Kms or hrs were tried to obtain and majority of participants living outside the town did not respond. So the distance in this study should be interpreted cautiously. Third, using telephone interview for some defaulters may reduce the quality of information as compared to controls. This was used only for very few individual thus may not harm the validity of the study. This study have identified important determinant factors of ART treatment defaulting. In this study living out of the town or far from the facility was significantly associated with ART treatment defaulting. Similar finding was reported by study done in Ethiopia, Kenya, Uganda and South Africa[10-13]. Distance to clinic and transportation are main factors for defaulting from care in a wide variety of settings developing countries[12-16]. This might be because people need to take time off from work to travel great distances to clinics and wait for the service all day. This may discourage patients to come back for ART treatment clinical appointments. Among the socio-economic, patients who had no source of food (economically poor) and living dependently (on relatives, NGO, Government, etc) were 14 times more likely to default compared to patients who live independently. In Jimma zone of Ethiopia, 17.6% of patients who defaulted reported lack of food as a reason for absence from clinic[10]. Patients mental status were significantly associated with ART treatment defaulting. This had been reported by study done in Ethiopia and Nigeria[10, 18]. Depression and emotional adjustment to the HIV infections have been observed as other possible reasons why patients default from ART use[18].Patients with a fear of stigma or Stigmatized patients were 8.3 times more likely to default than not stigmatized (had no fear of stigma). Similarly finding has been reported by study done in Botswana and Nigeria[18, 19]. Stigma is daily issues facing people infected with HIV/AIDS especially in developing countries. Stigma was mentioned as one factor that constrained patients on antiretroviral therapy from sticking to agreed-to treatment plans. The issue of stigma has been a barrier to people living with AIDS disclosing their status and getting access to available support and care services[18]. Patient whose partner was an HIV-negative partner or unknown HIV status was more likely to default from treatment. Similar finding had been reported by study done in Ethiopia[10]. These may be HIV-infected individuals who had an HIV-positive partner who provided support and encouragement compared to those who had HIV-negative or unknown HIV status partner[10].
5. Conclusions
- In Inclusion, PLWH who were living out of the town or far from the facility, whose partner’s HIV status was negative ot unknown, who were stigmatized and mental ill had a higher chance of defaulting from ART treatment. Besides, those who were dependent on other foor food were more likely to defasult from the treatment. So it is recommended to make ART treatment available patients at the village. The staff should advise the patients and make them to bring their partner for HIV test. Linking patients to local social support or facilitating income generating activities for PLWHA to increase their income should be a priority issue. Effort should be made to decrease stigma. Intensifying counseling of patients before initiating and during treatment is importance so that PLWHA can adjust both psychologically and emotionally to the disease. Addressing stigma on an individual level and community level should be considered.
ACKNOWLEDGEMENTS
- We would also like to thank Jimma University for its financial support. We are very grateful to all supervisors, data collectors and study participants who took part in the study.
Competing of Interests
- The authors declare that they have no competing interests.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML