-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2013; 3(4): 85-91
doi:10.5923/j.phr.20130304.01
Knowledge, Perception and Acceptance of Couple HIV Counselling and Testing in a Rural Community in Nigeria
Okoli Thompson1, Oladipupo Ipadeola2, O. N Makinde3
1Kings Care Hospital, Abuja, Nigeria
2Malaria Action Program for States, Abuja Nigeria
3Obafemi Awolowo University Teaching Hospital, Ile Ife Nigeria
Correspondence to: Oladipupo Ipadeola, Malaria Action Program for States, Abuja Nigeria.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
HIV Prevalence is still high in Nigeria and Mother to Child transmission of HIV is another burden on HIV positive sero concordance or discordance couples. The Couple HIV Counselling and Testing program (CHCT) was designed to assist in the prevention of mother to child transmission of HIV as a way of fighting against the dreaded HIV epidemics. There are no documented evidence on uptake and acceptance of this service among couples in Nigeria. This study therefore present finding from a household survey aimed at providing insight into people’s perception and acceptance of the CHCT in Nigeria. Adopting the Lot Quality Assurance Sampling Technique (LQAS), data was collected from 76 married men and women living in Kubwa, a rural community within the Nigeria Federal Capital Territory, by personal interview using structured Questionnaire. Filled questionnaires were entered into SPSS and analysis was performed. Findings showed that about 76.3% of the respondents have ever heard of Couple Counselling and Testing while about 60% have ever accessed CHCT. Almost all the respondents were willing to recommend CHCT to newly married or intending couples and about 30% perceived it as a way to promote faithfulness and trust between couples. To assess CHCT, most respondents preferred private hospitals to public health facilities. This study concludes that awareness of CHCT is fair and response is high among married men and women in the selected community.
Keywords: HIV, Couple HIV Counselling and Testing, LQAS, Mother to Child Transmission, Household Survey, Hospital, Perception
Cite this paper: Okoli Thompson, Oladipupo Ipadeola, O. N Makinde, Knowledge, Perception and Acceptance of Couple HIV Counselling and Testing in a Rural Community in Nigeria, Public Health Research, Vol. 3 No. 4, 2013, pp. 85-91. doi: 10.5923/j.phr.20130304.01.
Article Outline
1. Introduction
- Africa is made up of about 10% of the world’s inhabitants and is the region most affected by the HIV/AIDS pandemic. Africa also accounts for 67% of new HIV infections worldwide[1]. At the end of 2008, an estimated 31.3 million adults were living with HIV/AIDS worldwide, about 22.4 million of these were in sub-Saharan Africa, while 57% were women. Furthermore, approximately 90% of the infected children worldwide live in Africa[2]. The Federal Republic of Nigeria is the most populated country in Sub – Saharan Africa, with a population of over 140 million people[3]. The first HIV / AIDS case was reported in Nigeria in 1986 and since that time the number of reported cases has greatly increased. Data from the national sero–sentinel surveys carried out across Nigeria since 1991 show the adult prevalence as 1.8% in 1991, 3.8% in 1993, 4.5% in 1996, 5.8% in 2001, 5.0% in 2003, 4.4% in 2005 and 3.1% in 2007. With a population of 140,431,790, the latest estimates indicate that there are over 2.9 million HIV positive Nigerians[4] HIV Counselling and Testing (HCT) refers to the process by which an individual, couple, or family receives HIV testing and confidential dialogue on HIV prevention, treatment, care, and support.[5]. There are many approaches to HCT, but generally the intervention includes four activities: pretest counseling on the testing process; risk-behavior assessment; each participant’s informed consent; and post-test counseling based on the test result[5]. HIV Counselling and Testing is the gateway to treatment, care, support, and prevention interventions for those who have HIV. It is also a critical opportunity for HIV prevention counseling, particularly for couples where one partner is HIV positive (known as sero-discordance) and for others with a high risk of acquiring HIV. For those who test negative, counselling focuses on prevention messages tailored to the client's or patient's risk behavior(s) and provides referrals to prevention interventions, such as male circumcision clinics and support groups.[6]Couple HIV Counselling and Testing (CHCT) is a counselling and testing protocol whereby couples are given opportunity to be counselled for HIV and allowed to make a decision for testing and receiving the test result together. CHCT is particularly important especially in Ante Natal Clinic setting because it takes care of the challenge of disclosure of positive results to an uninfected partner. With a large portion of HIV infections occurring within stable relationships, CHCT is extremely important. In CHCT, partners attend counseling and testing sessions together and learn their results together. CHCT creates a safe environment for couples to discuss concerns; provides information on HIV prevention, transmission, and treatment; eases tension and reduces blame; and allows for joint decision making. In order to conduct a successful CHCT session, counsellors must be adequately trained and equipped with the appropriate skills to address the variety of issues that may arise. When testing couples together, there are three possible outcomes: concordant positive, where both are HIV positive; concordant negative, where both are HIV negative; and discordant, where one partner is HIV positive and the other is not. Couples with each respective outcome require specific information, referrals, and/or linkages during post-test counselling.Cohabiting couples in Africa now represent the world's largest HIV risk group[7, 8]. In Zambia, DNA sequencing confirmed that 87% of new HIV infections among negative individuals living in a sero-discordant couple were acquired from the spouse[9]. Until recently, most of the studies following-up HIV-negative or sero-discordant couples in countries facing generalised HIV epidemics tended to show that women are specifically at high risk of HIV infection within their regular partnership, presumably due to the infidelity of men and an increased biological susceptibility for women. These biomedical figures are also relayed by individual representations: women fear being infected by HIV by their spouse or regular partner, whereas men fear HIV infection from outside partners[10] In 2006 more than 65% of the 4.3 million new cases of HIV occurred in Sub-Saharan Africa. In this region, most transmission is heterosexual, occurring predominately between cohabiting partners[11]. Among pregnant women tested with their partners in antenatal clinics in Lusaka, the capital of Zambia, 19% of couples had two HIV+ partners ("concordant +") and 17% had one HIV+ and one HIV- partner ("discordant"). In Kigali, the capital of Rwanda, 8% of couples were concordant + and 9% were discordant[12]. These results are similar to those reported in couples' voluntary HIV counselling and testing (CHCT) centres[9, 13, 14], cluster sampling surveys and to those reported for couples in neighbouring Kenya and Tanzania Recent analyses of large-scale studies have shed a new light on the question of HIV infection within the couple. The analyses of the DHS data in Burkina Faso, Cameroon, Ghana, Kenya and Tanzania revealed that, in each of these countries, at least two-thirds of HIV-infected couples were sero-discordant couples. In half of these sero-different couples, the woman was HIV-positive and the man HIV-negative[15]. The United State Agency for International Development (USAID) is at the fore front of the fight against HIV/AIDS in Nigeria. They have been responsible for funding several prevention, treatment, care and support projects. They worked in partnership with The Directorate for International Development (DFID) to fund the “make we talk” program also known as the PSRHH, an acronym for Promoting Sexual and Reproductive Health and HIV/AIDS in Nigeria and the Comprehensive Integrated Approach to HIV/AIDS Prevention and Care in Nigeria (CIHPAC). These two projects were the major projects executed in Nigeria on HIV/AIDS through funding from the US and the British government respectively. USAID has worked with partners to support a wide range of HIV Counselling and Testing activities especially on the PEPFAR project. Some of the activities of USAID include, couples HCT,community-based HCT, and HCT in clinical settings, training and support for HIV counsellors and other staff, social marketing campaigns to promote HCT and enhance community acceptance of HIV/AIDS activities, engagement of other donors and local host-country governments to coordinate HCT efforts, development of HCT guidelines, policies, and protocols adapted to the specific country and cultural context, evaluations of new HIV rapid testing kits and technologies. The success story emanating from all these activities were well documented and reported at National and International conferences on HIV/AIDS and it was recorded that about 57 million HCT sessions were made available to men, women, and children from 2003 to 2008 worldwide. Thus, this study seeks to determine the knowledge and perception of married men and women living in Kubwa Village, a village under the Bwari Area Council of Abuja, on Couple HIV Counselling and Testing programme. Specifically, this project will determine opinion and acceptance of couples on uptake of the couple counselling and testing and also to determine how couple counselling and testing may affect the lives of couples when they find out their sero status to be discordant, concordant positive or negative. Result from this study will be useful in the design and implementation of Couple HIV Counselling and Testing by understanding salient factors that will encourage couples to go for the test together.
2. Methods
- This study was carried out among married men and women in Kubwa Village, under the Bwari Area Council in Abuja. Abuja is in the Capital city of the Federal Republic of Nigeria located in the North Central. It is a fast developing cosmopolitan city with a constant flow of international and local residents with visitors engaged in a variety of enterprises in the public and private sectors of the economy. The city has a population of 1,406,279[3] and an estimated 43,595 number of PLHIVs[4]. Kubwa is divided into four phases with clear boundaries. Sampling of the respondents is based on the Lot Quality Assurance Sampling technique.[16]LQAS is a method that combines two standard statistical techniques: stratified random sampling for data collection, and one-sided hypothesis testing for data analysis. The first step in employing LQAS is to divide the study population into useful lots such as villages or facility catchment areas [17, 18]. The sampling procedure requires a systematic selection of nineteen persons per phase. The selected phase was divided into three sectors such that six persons will be selected in each sector. The seventh person will be selected from the farthest of the three sectors. Based on the above, the total number of persons sampled for the study is 76. Standard questionnaires were used to elicit information from couples in the selected households. Data was collected from house to house questionnaire administration. The data were entered into an SPSS template where all other analysis was performed.
3. Results and Discussion
3.1. Results
3.1.1. Demographic Characteristics of Respondents
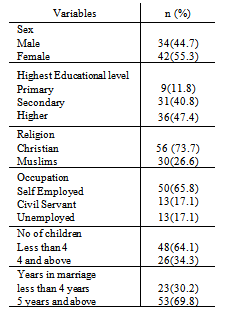
- The data collection took place in Kubwa, Abuja. A total of 76 respondents were interviewed. Data collection was concluded in three days and data entry was done on SPSS. Out of the 76 respondents, 44.7% were male while 55.3% were females. The age of respondents falls between 25 and 56 with a mean of 38.8 and standard deviation of 6.34. About 65% of the respondents were self employed or own small business. A higher percentage of the respondents (88%) have secondary or higher education and about 74% are Christians. Also about 70% have been in marriage for more than 5 years and almost all of the respondent have at least one child. All the respondents claim to have ever visited ANC and also all of them have ever done HIV Counselling and Testing as at the time of the survey. A summary of the basic demographical characteristics of the respondents is displayed in table 1.
|
3.1.2. Knowledge about HIV and CHCT
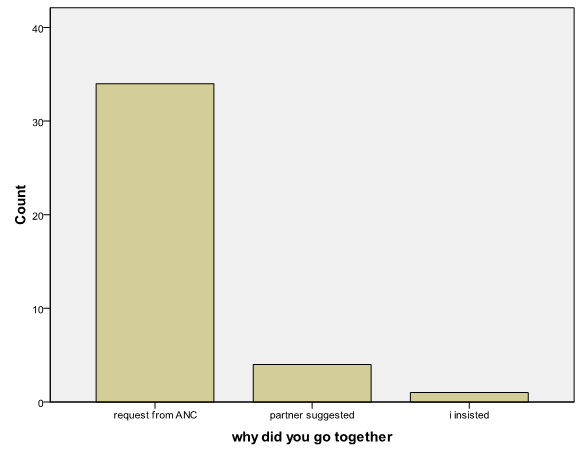 | Figure 1. Showing the distribution of reasons for attending HCT centres with partner (Reasons for Uptake of CHCT) |
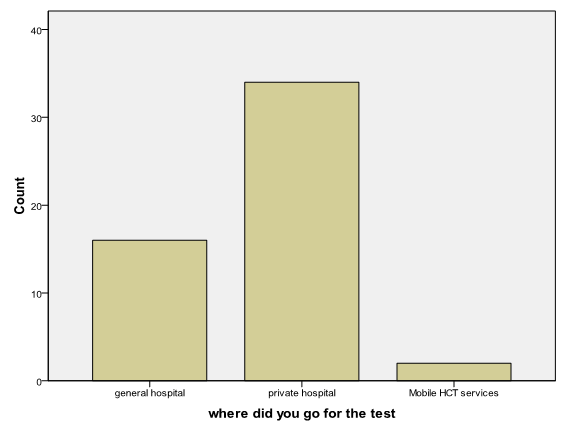 | Figure 2. Showing the distribution of places where respondents accessed CHCT services |
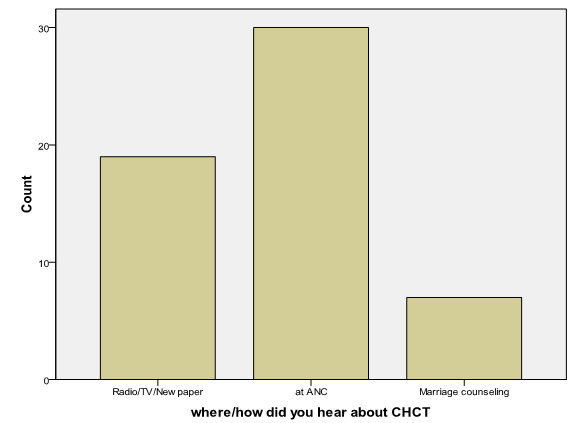 | Figure 3. Showing the distribution of various source of information about CHCT as reported by the respondents |
3.1.3. Perception about Uptake of CHCT Services
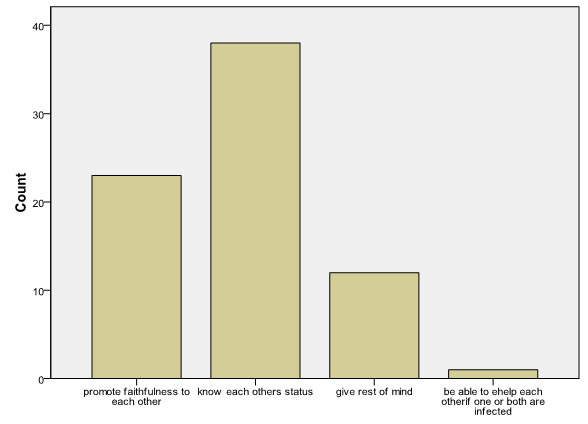 | Figure 4. Showing the distribution of respondent’s reasons to encourage CHCT |
3.1.4. Opinion on how Uptake of CHCT can be Improved
- Several attempts have been made to improve CHCT in Nigeria. One of the major interventions in this regards is encouraging male participation in ANC. Respondents were asked about their views and opinion about ways of encouraging CHCT in Nigeria. About 43% of the respondents believed that CHCT can be improved through increased awareness of the CHCT in Nigeria. Also about 16% of the respondents believed that uptake of CHCT can be improved if CHCT is integrated into other health services. About 31% still believed that partner involvement in ANC will promote CHCT while only 2% reported that making CHCT centres more users friendly will be a way of improving uptake of CHCT services in Nigeria. Most of the respondents mentioned that they are willing to take their partners with them for CHCT services and also willing to advice couples to go together for CHCT. They believe CHCT is better than HCT for married couples.
3.2. Discussion of Findings
- This study aims at accessing the level of awareness and uptake of CHCT in Nigeria and also describes the acceptability and willingness of couples to access CHCT. One of the important findings observed from the study was that CHCT is well known among the members of the community in Nigeria and has received general acceptance as most of the respondents were in support of the program. Also it was observed that a higher percentage of the respondents have ever accessed CHCT in times past and most of the couples interviewed already know their HIV status and that of their partner. This is in contrast to the belief that Nigeria has low uptake of CHCT and also a low acceptance level. Also this study was conducted among couples living in a semi urban area of Nigeria where there is a cluster of public and private health facilities which could be responsible for the high uptake of CHCT. However, it was observed that most person who reported to have ever accessed CHCT were from the women that has ever attended ANC and also most of the respondents had their CHCT session during the ANC visits with their partners. All the ANC attendants who accessed CHCT with their partners reported that the request to bring their partner was made by the ANC care providers. This is an indication that most couples in Nigeria who attends ANC will have been informed about CHCT and will also have accessed the service. Thus the twist to a successful CHCT program remains the promotion of the service through the ANC.Most of the respondents also reported having the CHCT session in private or faith based hospitals. Thus a way to improve uptake of CHCT is to continue to ensure that private and faith based hospitals are involved in the implementation of the program. This will require that staff of these private health facilities is given the required training and capacity building to effectively implement the CHCT program among people who prefer to private hospitals for their ANC and other health services. This study has identified some gaps in the implementation and design of the CHCT in Nigeria. Firstly, the respondents believed that CHCT is not receiving the publicity it deserves. There should be a more comprehensive and extended awareness campaign to sensitize people on the importance if CHCT and also notify them of where to access the services. Most of the respondents who heard about the CHCT were from the ANC and thus many people especially their male counterparts do not have access to information about the program. Sensitization program could come inform of road shows, posters and through the media for wider coverage.
4. Conclusions
- This study has been conducted in accordance with the principle of respect for persons, justice and benevolence with a suitable and scientifically approved methodology. All findings were reported based on the response of the respondents. In order to further stimulate and strengthen HIV prevention efforts and CHCT in Nigeria, increased attention is required to identify and promote adequate prevention messages and programmes aiming at HIV prevention within the couple. Based on the finding from this study additional research on HIV risk management and prevention within the couple relationship will need to be strengthened in Nigeria and data on couple HIV counseling and Testing should be made available as part of the annual report of health interventions. Finally, the objective of this study is to provide information on people’s perception about CHCT in Nigeria and suggest possible ways of improving uptake of CHCT. This has been attempted and reported here and findings from this study will encourage policy makers to improve on the implementation of the CHCT policy as a way of curbing the spread of HV/AIDS in Nigeria.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML