-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2013; 3(3): 79-84
doi:10.5923/j.phr.20130303.07
Differentials in Prevalence of Goitre among School Children (6-12 Years of Age) in Rural North-West, India
Gurdeep Singh1, Gurmeet Kaur2, Vijay Mengi3, Sunil Kumar Raina4
1Department of Community Medicine), AIMSR, Bathinda (Punjab), India, Department of Communtiy
2Medicine, Govt. Medical College, Jammu- India, Post-Graduate Department of Communtiy Medicine
3Govt. Medical College, Jammu, India, Dr.RP Government Medical College, Tanda, kangra
4Dr.RP Government Medical College, Tanda (kangra), Himachal Pradesh
Correspondence to: Sunil Kumar Raina, Dr.RP Government Medical College, Tanda (kangra), Himachal Pradesh.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
A cross – sectional study of prevalence of goitre and its association with certain Socio-cultural factors like age, sex, intake of iodized/non iodized salt, educational status of mother & income was conducted in children studying in different Govt. Schools of Miran Sahib Area of R.S. Pura Block, Jammu (India). 1610 children in the age group of 6-12 years were clinically assessed for the presence of goiter. The prevalence of goiter among children in 6-12 years was 12.1% (195/1610). No child with goitre grade 2 was found in the study. Prevalence of goitre was found to be high (20.96%) in children consuming non- iodized salt and was statistically significant. Prevalence of goitre was also found to be high (17.2%) in children from low income groups and also in children of illiterate mothers (16.6%), thus emphasizing the importance of these factors with the prevalence of Goitre.
Keywords: Prevalence, Goiter, Grade, Iodized Salt, Socio – cultural Factors, Chi-square(X2)
Cite this paper: Gurdeep Singh, Gurmeet Kaur, Vijay Mengi, Sunil Kumar Raina, Differentials in Prevalence of Goitre among School Children (6-12 Years of Age) in Rural North-West, India, Public Health Research, Vol. 3 No. 3, 2013, pp. 79-84. doi: 10.5923/j.phr.20130303.07.
1. Introduction
- Iodine is an important micronutrient required for human nutrition. Iodine deficiency disorders (IDD) refer to a complex clinical and sub clinical disorder caused by the lack of adequate dietary iodine and is the most common cause of preventable brain damage, mental retardation, stunted growth and development in children. Goitre is the most common clinical manifestation of Iodine deficiency in children and adults.Globally about 740 million people are affected by goitre and more than two billion (or over 38% of the population living in 130 countries) are estimated to be at risk of IDD. Many countries including China and India have come to regard their entire population as at risk of IDD.[1]In India, IDD constitute a major public health problem. Not a single state or union territory in the country is free from the problem of IDD; out of 587 districts in the country, 282 have been surveyed for IDD and 241 are found to be goitre endemic.[2] In India 167 million people are at risk for IDD, 54.4 million people have goitre, and 8.8 million people suffer from IDD related mental/motor handicaps.[3]World wise Iodine deficiency is a major threat to the health and development of population particularly in School age children and pregnant women when requirements of iodine are not met, thyroid hormone synthesis is impaired resulting in series off functional and developmental abnormalities collectively referred as IDD. Iodine deficiency disorders are among the easiest and cheapest of all disorders to prevent. The addition of a small amount of Iodine to the salt that people consume every day is all that needed. Generally school-age children are considered an appropriate target group because they fulfil the desired criteria of susceptibility to iodine deficiency, accessibility as a study group and representativeness of society as a whole.[4]The present study was designed:1. To determine the prevalence of goiter among children 6-12 yrs study in Govt. School of a Rural Area, Jammu.2. To determine the association with certain socio – cultural factors like age, sex, consumption of iodized/ non iodized salt, education status of mother & income of the family.
2. Material & Methods
- The study was conducted on 1610 school children studying on different Govt. Schools of Miran Sahib area of R.S. Pura Block in Jammu.Background: Strategically located J&K constitutes the northern most extremity of India. Situated between 32.17 degree and 36.58 degree north latitude and 37.26 degree and 80.30 degree east longitude, the total area of the State is 22,22,236 sq. kms including 78114 sq kms under the administration of Pakistan and 42,685 sq kms under that of China. The State is bounded by Pakistan, Afghanistan and China from the West to the East. The State is well connected with rest of the country by air, rail and road. (Figure 1) The State has 4 geographical zones of: (1) Sub-mountain and semi-mountain plain known as kandi or dry belt including Jammu district; (2) The Shivalak ranges; (3) The high mountain zone constituting the Kashmir Valley, Pir Panchal range and its off-shoots including Doda, Poonch and Rajouri districts and part of Kathua and Udhampur districts; and (4) The middle runs of the Indus River comprising Leh and Kargil. The State is the northern most state of India comprising threedistinct Climatic regions viz. Arctic cold desert areas of Ladakh, temperate Kashmir valley and sub-tropical region of Jammu. There is a sharp rise of altitude from 1000 feet to 28,250 feet above the sea level within State’s four degree of latitude. The population (2001 census) of the State is 10,143,700. The State with its summer and a winter capital at Srinagar and Jammu, respectively, is divided into 20 districts. One fifth of the population in J&K resides in urban areas; 23.83 % population has been recorded as urban in the state against the National Average of 25.72%. Jammu city has recorded very rapid growth and presently ranks as the 48th biggest city in the country.The study was conducted in the villages of Miran Sahib zone RS Pura health block of Jammu district, the winter capital of J&K. RS Pura health block field practice area for the Department of Community Medicine.
 | Figure 1. Map showing location of Jammu and Kashmir |
3. Results
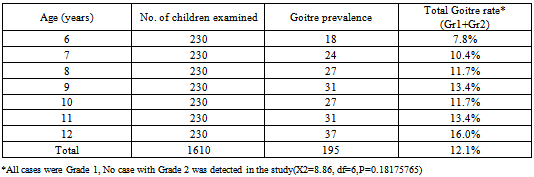
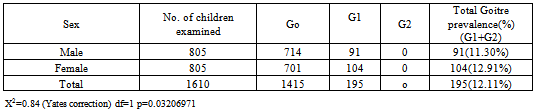
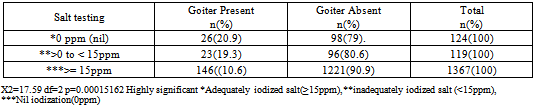
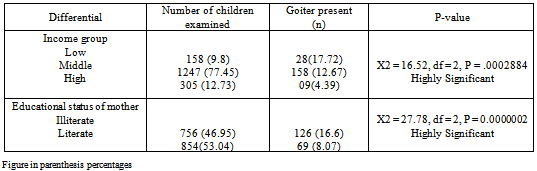
- 1610 children in the age group 6-12 years were screened for goitre in all. Goitre prevalence was found to be 12.1% in the school children. All cases had goiter grade1. No case with goiter grade 2 was found. The prevalence of goiter rate was increasing from 7.8% at age of 6 years to 16 % at age of 12 years except in the age at 10 years(11.7%) and this was found to be statically insignificant. (Table-1) Sex wise it was observed that 12.9 % of screened females had goiter as compared to 11.3% of males but this gender difference was not found to be statistically significant (X2=0.99,P=0.32) as shown in Table 2. Table 3 shows that out of total 1610 children, 1367 (84.9%) children were belonging to households consuming iodized salt (≥15ppm). Prevalence of giotre was high in children consuming salt with insufficient iodine (<15ppm) in comparison to children consuming salt with sufficient iodine(≥ 15ppm).This difference in prevalence was found to be statically highly significant ((X2=17.59,P=0.00015162) As shown in Table 4, Difference of goitre in relation to various socio-demographic revealed that there was significant association with the levels of income and literary status of mothers. The Prevalence of Goitre was found to be significantly high (17.7%) in children from low income group as compare to children (4.3%) belonging to high income group. The Prevalence of Goitre was high in children belonging to illiterate mothers about (16.6 %) as compare to low (4.3%) prevalence in children belonging literate mothers. High prevalence(13.1%) was found in children taking Goitrogenic vegetables (Cabbage, cauliflower, carrot) as compared to children taking non-goitrogenic vegetables having lower prevalence of 10.6% . However the difference was found to be non-significant.
|
|
|
|
4. Discussion
- The prevalence of goiter among children in 6-12 years was 12.1% (195/1610) in this conducted in Miran Sahib area of RS Pura health block. Micronutrient like iodine though required in micro-quantities are of enormous health significance taking part in a variety of biological functions.School children serve well for micronutrient surveillance. They are accessible and more over school based surveillance can provide a stimulus for teachers to develop health education activities including efforts to help children improve their own micronutrients intake and that of their families. Goitre is the most common clinical manifestation of iodine deficiency in children and estimation of its prevalence is commonly resorted to while carrying our iodine deficiency surveys.To evaluate the severity of Iodine deficiency disorder (IDD) in a region, the most widely accepted marker is prevalence of endemic Goitre in school children. WHO / UNICEF/ICCIDD on the basis of IDD prevalence, recommended the criteria to understand the severity of IDD as a public health in a region (WHO/UNICEF/ICCIDD, 1994).[6] According to this criteria, a prevalence of rate of 5% - 19.9% is considered as mild; 20 - 29.9% as moderate and prevalence rate of above 30% considered as severe.In studied School children, the prevalence of goitre was found to be 12.11% and according to the WHO – UNICEF – ICCIDD guide lines the rural area of Jammu falls in the mild iodine deficiency category of severity of IDD by goiter prevalence in school children.A similar prevalence of 12.1% was also found by kapil U in Kangra in H.P.[7] Biswas ABalso reported a similar prevalence of 11.3% in their study.[8] W.H.O bulletin 2005 has estimated the Global total Goitre prevalence to be 15.8%.[9] However, a higher prevalence of 21.1% was reported by C.S Pandav (1995) in a survey done in nine states outside the traditional Goitre belt.[10] A low prevalence of 4.78% was reported in 6-12 year children by an ICMR study done in 15 districts of India.[11]U Kapil (1998) reported a Goitre rate of 6.1% in school children 6-10 years in their study.[12] However a micronutrient profile of Indian population by ICMR reported the overall Goitre (Grade I and 2 combined) to be about 10% which is consistent with the prevalence rate seen in this study.[13] In the state of J & K, 14 districts were surveyed for IDD and all were found to be endemic: the district nutrition project done by ICMR 2001 found the prevalence of Goiter in Srinagar to be 4.46% and of Baramulla 0.9%.[14]The prevalence of goitre was found to be high in girls (12.91%) as compared to boys(11.30%). R K Gakkhar 2001 reported a higher prevalence of 3.2% in girls than boys.[14]The prevalence of goitre was also found to be high in children taking non-iodized salt as compared to children taking iodized salt which was found to be (20.96%) followed by 19.32% in children consuming inadequately iodized salt and 10.60% in children consuming adequately iodized salt. The National Health Family Survey (N.H.F.S) II (98-99) in J&K showed that 29.8% of the rural households were using non-iodized salt, 26.9% were using inadequately iodized salt and 24.8% use inadequately iodized. The same survey has shown that only half of all households (53%) used iodized salt and this is quite low in light of Govt. regulations salt iodization. WHO/UNICEF/ICCIDD recommends that 90% of households salts should get iodized salt at the recommended level of 15 ppm (ICCIDD /UNICEF WHO, 2001) and the present study showed that out of 1610 children, 1367(84.90%) children were consuming adequately iodized salt (≥15ppm), 109(6.77%) inadequately iodized salt (<15ppm), while about 124(7.70%) consuming salt with nil iodization(0ppm), suggesting the need to strengthen the system of monitoring quality of salt to ensure availability of 15 ppm of iodine at household level. Regarding the income groups, the prevalence of goitre was high 17.22% in low income groups as compared to 4.39% in high income groups, this could be attributed to consumption of adequately iodized salt by people belonging to high income groups and according to NFHS survey II, 80% of household with high standards of living use adequately iodized salt as compared to 33% of households with a low standard of living. The low prevalence of goitre (8.07%) in children of literate mothers could because literate mothers were more aware of the benefit of iodized salt and were able to look after the health of their children in a better way. Prevalence of goiter was high (13.16%) in children taking Goitrogenic vegetables (Cabbage, cauliflower, carrot) as compared to children (10.68%) not taking–goitrogenic vegetables and this difference of prevalence was found to be not statically significant. Goitrogens interefere with Iodine utilization by throid gland and are found in brassica group of vegetables. [15]
5. Conclusions
- Iodine deficiency is a public health problem of mild severity in the school children aged 6-12 yrs, studying in different Govt. schools of the rural area of Jammu. Iodine deficiency can be prevented by using salt that has been fortified with iodine, and the recommended levels of iodization are to be ensured at household levels.Continuous concerted efforts should also be made to strengthen information education and communication (IEC) activities needed to be undertaken in order to create awareness about the detrimental effects and prevention of IDD, and encourage iodated salt consumptionSchool children follow what the teachers do and say and teachers are considered as good role models to transmit the value of life and ways of life in schools as also outside schools. School children can be used as ambassadors of health message to their homes and neighborhood and as change agents.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML