-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2012; 2(5): 114-119
doi: 10.5923/j.phr.20120205.01
Breast Cancer and Mammography: Current Knowledge, Attitudes and Practices of Female Health Workers in a Tertiary Health Institution in Northern Nigeria
Oche MO , Ayodele SO , Umar AS
Department of Community Health, Usmanu Danfodiyo University, Sokoto, Nigeria
Correspondence to: Oche MO , Department of Community Health, Usmanu Danfodiyo University, Sokoto, Nigeria.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Breast cancer is one of the most common causes of cancer related deaths among women worldwide, accounting for 31% of cancers among women and 19% of deaths among women are due to cancer. Early detection of breast cancer and early presentation for management has been shown to reduce mortality rates. This descriptive cross-sectional study involving 100 female health workers made up of 30 doctors and 70 nurses was carried out at the Usmanu Danfodiyo University Teaching hospital, Sokoto .The study is aimed at assessing the knowledge of female health workers about breast cancer and their attitude and practice of mammography. A total of 67% of the study subjects had adequate knowledge of breast cancer and its risk factors with 80% of the female doctors having better knowledge compared to the nurses. Majority, (84%) of the respondents were aware of mammography as a way of detecting early cancer of the breast and only 9% of them had undergone the procedure in the last one year. The commonest reason for not undergoing the procedure was that they were not aware of the procedure being carried out in the study centre. The low mammographic screening rate recorded in the study portrays a bad omen for the fight against cancer of the breast and this reinforces the need for educational intervention to increase the awareness and uptake of mammographic screening among the study population.
Keywords: Breast Cancer, Knowledge, Female Health Workers, Mammography, Nigeria
Cite this paper: Oche MO , Ayodele SO , Umar AS , "Breast Cancer and Mammography: Current Knowledge, Attitudes and Practices of Female Health Workers in a Tertiary Health Institution in Northern Nigeria", Public Health Research, Vol. 2 No. 5, 2012, pp. 114-119. doi: 10.5923/j.phr.20120205.01.
Article Outline
1. Introduction
- Breast cancer is one of the most common cause of cancer related deaths among women worldwide(1-3) accounting for 31% of cancers among women and 19% of deaths among women are due to cancer(1). In Nigeria as well as in other parts of the world, Breast cancer remained the most common cancer among women and the second leading cause of death(4-7). While breast cancer is one of the commonest reasons for death among women, it has been observed that detection and diagnosis at the earlier stage of the disease allows women variable treatment options and a greater chance of survival(1)In Nigeria, the burden of the disease is increasing and mostly at advanced stages with minimal hope of any intervention that will significantly reduce disability and mortality(8). One of the major reasons observed for the late presentation was the lack the access by most women to vital information on the factors that decrease breast cancer risks(9,10).Aderounmu et al in their study on the knowledge and at titude of women to cancer of the breast in South WesternNigeria noted that inadequate knowledge of the disease andthe limited awareness of the risk factors for cancer of the breast contributed significantly to the poor prognosis of breast cancer(11).Early detection of breast cancer and early presentation for management has been shown to reduce mortality rates and it is therefore important that regular screening methods be encouraged among populations(12). Empowering female health workers and creating awareness amongst them could go a long way in enhancing the screening program for breast cancer.Breast self examination(BSE), clinical breast examination(CBE) and mammography are the secondary preventive methods used for investigation in early detection of breast cancer(13). According to the American Cancer Society(ACS), women should know how their breasts feel and report promptly to their health care providers any breast changes. Although ACS does not recommend BSE any longer as breast cancer detection though BSE does not increase survival rate(14), It is still widely practiced in most developing countries where CBE and mammography are not readily available and accessible to the vast majority of the women population. This was further underscored by the reported five year survival of breast cancer in Nigeria to be less than 10% compared to 70% in Western Europe and North America(3). Several studies have reported and established a positive association between performance of BSE and early detection of breast cancer (8,15). Health workers play a vital role in empowering women with the necessary information on the various secondary preventive methods on the early detection of breast cancer. For health workers to be effective in imparting health education, they must possess the appropriate knowledge, attitude and beliefs concerning the health behaviour being promoted (18). Nurses and other health care workers who are saddled with the responsibility of giving health talks in clinics can now play a vital role in patient education about breast cancer screening methods (19). They also play a unique role in alerting the community to the early detection of breast cancer as they are usually the closest contacts with female patients(20,21). However, studies in the USA and South western Nigeria have reported knowledge gaps among physicians and nurses in promoting breast cancer screening(16,17).Furthermore, studies have shown that the attitude and orientation of health care providers are important determinants of use of breast cancer screening programs(22,23). Several reports about breast cancer in Nigeria have observed very low knowledge about symptoms of cancer of the breast and various screening methods(8,17,24). The paucity of knowledge and attitude on part of health workers could constitute an impediment to institutional frameworks and policies targeted towards sensitization of the women populace about breast cancer and mammography. Carrying out annual mammography is considered the most valuable tool for detecting breast cancer in the earliest possible stages, before the cancer has metastasized and when interventions are most effective and least invasive and debilitating(25).Similar studies have not been carried out in this part of the country and considering the increasing rate of cancer of the breast in Nigeria, which formed the basis for this study, aimed at assessing the knowledge of female health workers about breast cancer and their attitude and practice of mammography.
2. Methodology
- The design was a descriptive cross-sectional study carried out amongst female health workers at the Usmanu Danfodiyo University Teaching Hospital Sokoto, North Western Nigeria.The hospital is one of the referral centres in north –western part of Nigeria and renders preventive, curative andrehabilitative services including Magnetic resonance imaging (MRI), mammography and radiotherapy among others. The Teaching hospital has a 650 bed capacity with a staff strength of over 1,300 including 166 female health workers.A total of 100 female health workers made up of 30 doctors and 70 nurses were selected proportionate to their population from the departments of obstetrics and gynaecology, surgery and family medicine who are involved in the day to day patient management. A set of comprehensive, structured pretested and self administered questionnaire was administered to the respondents.
3. Instruments and Data Collection
- The questionnaires sought information on biodata, respondents’ knowledge such as signs and symptoms of cancer of the breast, mode of presentation, risk factors, screening and diagnostic procedures and management options available in the study area, attitude towards cancer of the breast and practice of mammography screening. The questionnaires were sorted out for completeness and data cleaning after which data was entered into and analysed using Epi-info version 3.4(2008).The answers to the knowledge questions were scored and graded with each correct answer to a questions attracting one mark and no marks awarded to a wrong answer. Scores <50 and ≥50% were adjudged inadequate and adequate knowledge respectively. There was cross tabulation of variables with level of statistical significance set at 95% confidence interval.
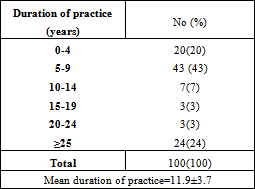
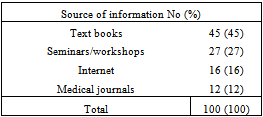
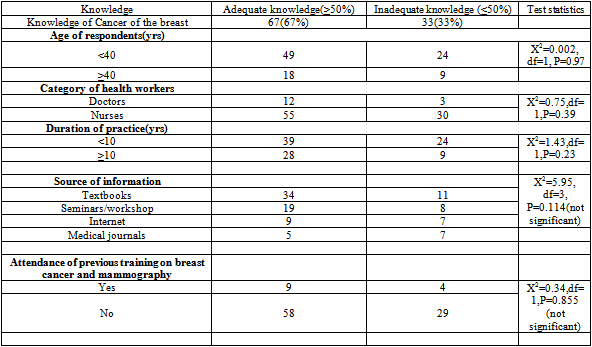
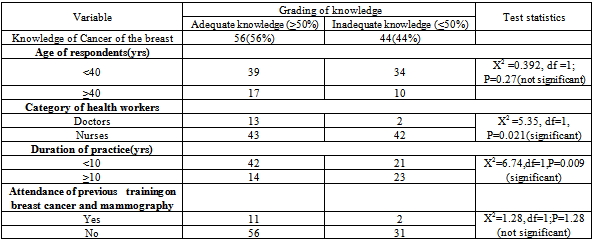
4. Results
| |||||||||||||||||||
|
|
|
|
|
|
5. Discussion
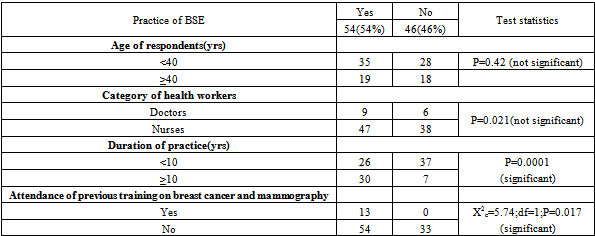
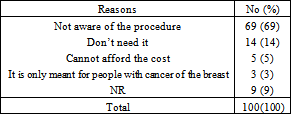
- For health workers to function as effective promoters of breast cancer control through early detection, they must possess the relevant knowledge as well as appropriate attitude and belief concerning the disease and its early detection(18). The respondents in this study demonstrated good knowledge of cancer of the breast and its risk factors as majority(67%) of them had adequate knowledge of the disease. The high knowledge observed in this study is in agreement with the findings from similar studies in Los Angeles, Western Turkey and Ibadan(16,25,26). However the level of knowledge recorded in our study was higher than the findings from other studies where lower figures were observed for the knowledge of breast cancer(27,28). Doctors in our study group had a better knowledge as 80% of them had adequate knowledge of breast cancer which is in consonance with findings from similar studies in Benin city and Lagos, Nigeria(27,29). Although the female doctors in the study had a better knowledge of breast cancer compared to all the other cadre of health workers, this was however found not to be statistically significant(P=0.39). The high knowledge recorded by the female doctors may not be unrelated to the content of their undergraduate curriculum which covered the subject under study. Similarly, the age of respondents(P=0.97) and duration of practice(P= 0.23) did not have any significant impact on the level of knowledge of the respondents about breast cancer and its risk factors. There was a very high level of awareness(84%) about mammography and its use in early detection of breast cancer amongst the respondents in our study. This is in keeping with findings from the study in Benin city, Nigeria where their subjects equally recorded a very high level of awareness(80.7%) about mammography(27). However more than half(56%) of the respondents had adequate knowledge of mammography and its ability to detect cancer of the breast in the early stages. Although the respondents in this study reported high levels of awareness and knowledge concerning mammography, only 32% of them were aware of the procedure being carried out in the study area. This underscores the need to enlighten the female health workers on the availability and use of mammography in detecting cancer of the breast at its earliest stages since these group of health workers are the closest to the female patients who are the eventual recipients of this procedure. The study by Akhigbe and colleagues showed that only 23.7% and 35.9% of their respondents had good and poor knowledge of mammography(27).More than half(57%) of the women in this study showed positive attitude towards mammography and would advise other women to go for it. The high knowledge and awareness about mammography could have contributed to this positive attitude of the respondents. Similar positive attitude to mammography was observed in the study by Bastani et al(18); however the study from Mulago hospital in Kampala showed that all the women in their study generally reported negative attitude towards mammography(28).In this study, only 9(9%) of the respondents had actually undergone mammography. Similar low level of utilization of mammography was previously reported from other centres(17,27,29). In a study carried out at Mulago hospital, Kampala, it was observed that none of their subjects had ever done a mammography and the main reason for this was the high cost of the procedure(28). The low level of utilization of mammography amongst our study subjects may not be unrelated to the lack of awareness about mammography being carried out in the study centre in contrast to the non availability of the mammography in some centres(27). The cost of carrying out a mammography in the study centre is one of the cheapest in the country(less than four thousand naira or <USD25) and yet the female health workers never availed themselves of this opportunity. High utilization of mammography as a result of increased awareness has been reported from other centres(6,30). Some of our study subjects opined that they were not at risk of cancer of the breast, hence they do not need to under mammography, which is in consonance with findings from the study by Odusanya and others(17). Other studies have observed factors like mammography induced pain and fear of irradiation as possible barriers to effective utilization of mammography(31). These barriers can be overcome through a systematic program of continuous dissemination of information about breast cancer and early diagnosis using mammography. The low screening rate with mammogram observed in our study is more alarming considering the fact that all our respondents are female health workers who have good knowledge of breast cancer, its risk factors and complications and are better placed to take the lead in getting screened. With this they can thus advise the women folk on the need for periodical screening using mammography.More than half, 54% of the study subjects do carry out regular breast self examination(BSE). In a culturally sensitive society like ours, BSE is preferred to clinical breast examination(CBE) which many patients may find embarrassing especially when carried out by male doctors. Studies that investigated the possible benefits of BSE have concluded that regular practice of BSE increases the chances of detecting breast cancer at its earliest stages(32). Although the American Cancer Society(ACS) no longer recommends BSE(14), in scarce resourced developing countries like Nigeria where the cost of mammography is beyond the reach of the average woman and there is dearth of clinicians, BSE is still the preferred choice and is recommended for early detection of breast lumps that could be precursors for cancer of the breast.The proportion of our subjects who carried out regular BSE (54%) is comparable to figures obtained in other studies (18, 30), but far lower than the figures observed from Lagos(83%) and Benin city(77.6%) in Nigeria and Singapore (93.7%) (6,27,29).
6. Conclusions
- Data from this study reflect a good knowledge of breast cancer and mammography by the study population with more than half(54%) of them performing regular BSE. However, the low awareness about mammography and the low mammographic screening rate recorded in the study underscores the need for educational intervention to increase the awareness and uptake of mammographic screening among the study population.Conflicting interests: The authors declare that they have no conflicting or competing interests
Authors’ Contributions
- OMO and UAS conceptualized and designed the study in addition to data analysis and manuscript preparationASO carried out the literature search and data generation.All the authors reviewed the manuscript on completion.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-Text HTML
Full-Text HTML