-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
p-ISSN: 2167-7263 e-ISSN: 2167-7247
2012; 2(4): 110-113
doi:10.5923/j.phr.20120204.08
Association Between Malaria Parasite Density in Pregnancy and Fetal Birth Weight in a University Teaching Hospital
Nwangwa E. K, Ekhoye E. I.
Department ofPhysiology, Faculty of Basic MedicalScience, College of HealthScience, Delta State University, P.M.B 001, Abraka, Delta State, Nigeria
Correspondence to: Nwangwa E. K, Department ofPhysiology, Faculty of Basic MedicalScience, College of HealthScience, Delta State University, P.M.B 001, Abraka, Delta State, Nigeria.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
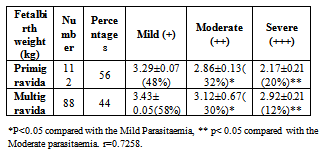
Malaria in pregnancy is an obstetric, social and medical problem requiring multidisciplinary and multidimensional solution. In Africa, perinatal mortality due to malaria is at about 1500/day. In areas where malaria is endemic, 20-40% of all babies born may have complications of malaria.In this Prospective study, two hundred (200) consenting pregnant women who were attending antenatal clinic in a University Teaching hospital who met the inclusion criteria were recruited for the study. Malaria parasitaemia were examined using Giemsa staining of the thick and thin blood films and WBC by coulter automated cell count and QBC centrifugal haematology system. Other parameters (fetal birth weight, gestational age, parity, maternal age) were also documented. The result showed a strongly positive correlation(r =0.7258) and statistically significant (p<0.05) decrease in birth weight for mild (3.29±0.07kg), moderate (2.86±1.33kg) and severe (2.17±0.213kg)parasitamia in primigravida and mild (3.43±0.05kg), moderate (3.12±0.05kg) and severe (2.92±0.21kg) in multigravida.Also found is that the average birth weight in primigravida (2.85±0.158kg) is lower than that of multigravida (3.07±0.039kg). It is therefore, recommended that malaria screening should form part of routine antenatal investigations in malaria endemic regions to prevent the problems associated with low birth weight.
Keywords: Malaria Parasite Density, Birth Weight, Pregnancy
Cite this paper: Nwangwa E. K, Ekhoye E. I., Association Between Malaria Parasite Density in Pregnancy and Fetal Birth Weight in a University Teaching Hospital, Public Health Research, Vol. 2 No. 4, 2012, pp. 110-113. doi: 10.5923/j.phr.20120204.08.
Article Outline
1. Introduction
- Malaria causes about 400 – 900 million cases of fever and approximately one to three million deaths annually[1]. The vast majority of cases occur in children under the age of 5 years, pregnant women are also vulnerable[2]. Hundreds of millions are infected each year and it is responsible for one million deaths per year worldwide, 90% in Africa[3].It is estimated that each year over 30 million women become pregnant in malaria infected areas of Africa with most living in area of stable malaria transmission[4]. Despite the effort to reduce transmission and increase treatment, there has been little change in these areas at risk of this disease[5]. Indeed, if the prevalence of malaria stays on its present upwards course, the death rate could double in the next twenty years[1]. Malaria and pregnancy are mutually aggravating conditions. The physiological changes due to malaria have a synergistic effect on the course of each other, thus making the life difficult for the mother, the child and the treating physician. Most epidemiologic studies conducted in the malaria endemic countries have found the primigravidae are more susceptible in human malaria than multigravidae[6].In areas of intense transmission, Plasmodium falciparum infection during pregnancy is usually asymptomatic and therefore remains undetected and untreated, despite the presence of parasites in the placenta. The main adverse manifestations of malaria in pregnancy are maternal anaemia and pre-term delivery[7,8.9]. Malaria parasitaemia has been associated with risk factor for low birth weight babies caused by intra-uterine growth retardation (IUGR) and pre-term deliveries (PTD)[10]. A healthy birth weight is extremely important for newborn as low birth weight babies are more susceptible to health problems, slower development, delayed milestones and low immunity[11]. It is also established as an important risk factor for neonatal morbidity[12]. Therefore, pregnant women must acquire a form of pregnancy-associated immunity during their first pregnancies that helps protect them during subsequent pregnancies[7]. The aim of this study is to find the association between malaria parasite density and birth weight in relation to Primigravida and multigravida.
2. Materials and Methods
2.1.Study Area
- This study was carried out in University of Benin Teaching hospital,Benin City. Edo State Nigeria. It is located at the south- south geographical oil rich region with rain forest Vegetation. Malaria transmission is stable and all-round the year.
2.2.Study Population, Data Collection, Data Analysis
- The studypopulation was drawn from both primigravid and multigravid women and their newborn babies, and were recruited from March 2009 to October, 2010 as part of prospective study investigating the effect of malaria parasitaemia on fetal birth weight. Women with pregnancy induced hypertension, diabetes mellitus, parity greater than four, renal disease, smokers and other chronic ailments e.g. sickle cell, and asthma were excluded from this study. Maternal age, weight and birth weight of the babies’ data were collected for this study.
2.3. Study Population
- During this course of study, pregnant females with ages ranging from 20 to 44 years attending antenatal clinic at the Obstetrics and Gynecology department of University of Benin Teaching Hospital were considered.All pregnant women who presented on different occasions with signs and symptoms of malaria (fever, headache, easy fatigability and weakness) in different trimesters and during labour were tested for malaria. Those who were positive and met inclusion criteria were recruited for the study. The total number of subjects used for the study was 200 pregnant females.
2.4. Sample Collection and Analysis
- Maternal blood samples were collected during labor by pricking the finger with a sterile lancet and collecting 1 or 2 drops of blood directly on two clean glass slides and immediately thick and thin blood film were made using Giemsa staining technique. The air dried smears were field stained, flushed in clean water and slanted on a draining rack to air dry. The dried stained smear was microscopically examined at x100 objective (oil immersion). The diagnosis of malaria was based on the identification of asexual plasmodium on the thick blood film while the thin blood film was used to identify species of plasmodium. About 3 ml in tube were transported on ice within 1 hours to a laboratory and within 2 hours of initial sample collection, WBC were counted by a Coulter automated cell count(Beckman-Coulter) and a QBC centrifugal haematology system(Becton-Dickinson Diagnostic system). The density of the parasite attack was determined by counting the number of asexual parasites against 100 leucocytes on the thick blood film and converted to parasite/µl assuming the total white blood cell count to be 8000 leucocytes/µl.Parasite Density = Number of parasites present X 8000 Average WBC count per µl of blood1 – 10 parasites/ 100 hpf was regarded as(+) or mild infection11-100 parasites/ 100hpfwas regarded as (++) or moderate infection1-10 parasites/1hpf of blood as (+++) or severe infection.
2.5. Ethical Consideration
- Institutional approval was obtained from University of Benin Teaching Hospital to conduct the research in the antenatal clinic of Obstetrics and Gynaecology department.
2.6.Statistical Analysis
- Statistical analysis of measures of central tendency and dispersion of variables (gestational age, maternal age, parity and fetal birth weight) was performed. Evaluation of the relationship between parasite density and fetal birth weight was analysed by Pearson;s correlation coefficient and statistical significance by students t-test. All analysis was performed using SPSS version 17.0. The level of significance was considered at P<0.05.
3. Results
- More number of women in this study group were in the young and prime reproductive period age category. i.e. < 25 years of age (36%) followed by 25 - 30 years (33%) and >30 years (31%).
|
4. Discussions
- Pregnancy and the physiological changes associated with it has been shown to be a predisposing factor to malaria, its associated maternal anaemiaand the resultant reduction in birth weight. Atypical manifestation of malaria is common in pregnancy, particularly in the second half of pregnancy.Malaria during pregnancy has been reported to be an important determinant of fetaloutcome[13, 8]. Findings from this study indicates that malaria parasitaemiasignificantly (P< 0.05) decreases fetal birth weight; this reduction in fetal birth weight is highly dependent on the degree of parasitaemia. With increasing number ofpregnancies, the incidence of low birth weight is reduced[14], with primigravida having an average birth weight of 2.85± 0.158kgand multigravida 3.07±0.039 kg.The increased risk of malaria among primigravidae has been well described[7], and is again seen in this study population. According to Brabin,[13] the reduction in birth weight is usually more marked in primigravidae but can extend to second and third gravidae in areas of low malaria transmission [15]. Also in this study most of the subject (56%) had term delivery (37-40 weeks) showing that malaria does not have any significant effect on the gestational age at delivery this was similar to other findings where the two main Plasmodium species, P. falciparum and P. vivax, were associated with lowbirth weight, but they do not reduce gestational age [15,16,17,18].
5. Conclusions
- It is obvious from this study that malaria parasitaemia in pregnancy has a negative effect on fetal birth weight. Therefore, there is an urgent need for an intensified effort against malaria in pregnancy by the adoption, practice and the sustainability of the measures targeted at preventing malaria transmission in order to guide against the risk of maternal anaemia in pregnant women and also to reduce fetal morbidity, still birth, and infant mortality that results from low birth weight attributable to malaria during pregnancy. The use of intermittent prophylactic therapy (IPT) in pregnancyis therefore highly encouraged especially in malaria endemic area.
6. Recommendations
- It is recommended therefore, that malaria control practices should form part of safe motherhood and should be sponsored from the national health scheme fund and made available and accessible at all levels of health care system.
ACKNOWLEDGEMENTS
- The researchers wish to thank the staff of Obstetrics and Gynaecology department of University of Benin Teaching Hospital for their support and assistance
References
| [1] | Breman J (2001); The ears of the hippopotamus; Manifestation, determinants and estimates of malaria burden; AMJ Trop Med publisher, New-Jersey |
| [2] | Greenwood B M, Greenwood AM, Bradley AK, Byass P, Jammeh K, Marsh K et al. 1987 Mortality and morbidity from malaria among children in a rural area of the Gambia, West Africa. Transactions of the Royal Soceity of Tropical Medicine Hygeine; 81: 478-486 |
| [3] | WHO (2010). Roll Back Malaria WHO partnership. "Economic costs of malaria" |
| [4] | World Health Organization/UNICEF. 2003. Africa malaria report 2003. WHO/CDS/MAL/2003.1093. World Health Organization, Geneva, Switzerland. |
| [5] | Hay S, Guerra C, Tatem A, Noor A, Snow R (2004). "The global distribution and population at risk of malaria: past, present, and future". Lancet Infect Dis 4 (6): 327–36.PMID 15172341. |
| [6] | Bray R.S, Anderson M.J., (1979) Falciparum Malaria and Pregnancy. Transactions of the Royal Soceity of Tropical Medicine and Hygiene; 73:427-431 |
| [7] | Brabin BJ (1983) An analysis of malaria in pregnancy in Africa. Bulletin of the World Health Organization 61, 1005–1016 |
| [8] | Menendez C (1995) Malaria during pregnancy: a priority area of malaria research and control. Parasitology Today 11, 178– 183. |
| [9] | Steketee RW, Nahlen BL, Parise ME & Menendez C (2001) The burden of malaria in pregnancy in malaria-endemic areas. American Journal of Tropical Medicine and Hygiene 64, 28–35. |
| [10] | McGregor I.A.,Wilson M.E., Billewicz W.Z. (1983). ‘Malaria infection of the placental in the Gambia West Africa. Its incidence and relationship to still birth, birth weight and placental weight’.transections of the Royal Soceity of Tropical Medicine and Hygeine; 77:232-244. |
| [11] | Walter PR, Garin Y, Blot P.1982 Placental pathologic changes in malaria. A histological and Ultrastructural study. American Journal of Pathology; 109: 330-342. |
| [12] | Borja JB, Adair LS 2003 Assessing the net effect of young maternal age on birth weight, American Journal of Human Biology 15 (6) 733-740 |
| [13] | Brabin BJ. (1991): The risks and severity of malaria in pregnant women. In: Applied field in malaria reports, no. 1. Geneva, Switzerland: World HealthOrganization,.(TDR/FIELDMAL/ 1). |
| [14] | Brabin, B. and Piper, C. (1997). Anaemia and malaria attributable low birth weight in two population in Papua New Guinea. Ann. Human Biol. 24: 547-555 |
| [15] | NostenF,Kuile FO, Maelankirri L, (1991). Malaria during pregnancy in an area of unstable endemicity. Trans R Soc Trop Med Hyg;85:424–9. |
| [16] | Nosten F, McGready R, Simpson JA, (1999). The effects of Plasmodium vivax malaria in pregnancy. Lancet;354: 546–9. |
| [17] | Dolan G, Kuile FO, Jacoutot V, (1993). Bed nets for the prevention of malaria and anaemia in pregnancy. Trans R Soc Trop Med Hyg;87:620–6. |
| [18] | Nosten F, terKuile F, Maelankiri L, (1994). Mefloquine prophylaxis prevents malaria during pregnancy: a double-blind, placebo-controlled study. J Infect Dis 169:595–603. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML