-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Public Health Research
2012; 2(4): 75-83
doi: 10.5923/j.phr.20120204.03
Life Habits and Personal Behaviour of Physicians Working in Government Service and Private Practice in Croatia- a Pilot Study
Ema N. Gruber
Department of psychiatry, Neuropsychiatry Hospital “Dr. I. Barbot”, Popovača, Croatia, psychiatrist
Correspondence to: Ema N. Gruber , Department of psychiatry, Neuropsychiatry Hospital “Dr. I. Barbot”, Popovača, Croatia, psychiatrist.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
The goal of this research was to compare the life habits and personal health behaviour of 182 physicians in government services and in private services and to gain better insight in life habits and personal health behaviour of physicians in general. Methods: Using the 20 statements regarding life habits and personal health behaviour. Results: There are no differences between life habits of physicians regarding the type of service they work except that almost all physicians working in government services stated that they had at least a one close confidential friend while only 2/3 of physicians practice in private services did so. Although 2/3 of doctors from both groups consider themselves “in good health”, more than half of them stated that they were an inappropriate weight for their height and most of them did not exercise regularly. More than 1/3 always drinks more than five alcoholic drinks a week and 1/3 always smoke more than half a pack of cigarettes a day. Conclusion: The type of service that physicians work in makes no difference on their life habits and personal behaviour except that physicians in private services have significantly less confidential friends. The better insight in life habits and personal behaviour of Croatian physicians was gained from the study and “target” spots for interventions are found: attitudes and behaviour considering unhealthy nutritional regimen, excessive alcohol consumption, smoking and lack of physical activity. The benefit of this study is that it emphasizes the need for further research on the subject, since there is a need for improvement of physician’s attitudes, life habits and behaviour. Changing attitudes towards unhealthy nutritional regimen, excessive alcohol consumption, smoking and lack of physical activity could also be, for physicians, a beneficent way to improve the health of their patients serving as a “good model”.
Keywords: Attitudes, Life Habits, Personal Health Behaviour, Physicians Practice in Private Services, Physicians Practice In Government Services
1. Introduction
- The reasons for performing the study were:- To compare the personal health behaviours of physicians in government and private services - To gain better insight in attitudes, life habits and personal behaviour of Croatian physicians in general and comparing to Croatian Adult Health Surveys results.- To emphasize “target” spots for actions or interventions for prevention or improvement of physicians lifestyleHypothesis:- Physicians that work in private services will have worse life habits due to a higher occupational stress and less friends since they are isolated from hospitals than physicians from government services.- In general, the attitudes, life habits and personal behav iour of Croatian physicians will differ comparing to the habits of physicians from other European countries and it will probably be the same as the habits from Croatian Adult Health Surveys results.It is general knowledge that good habits, such as regular practice of physical exercise, enough leisure time, and not smoking are associated with positive health in general and should be encouraged(1), in all people as well as in physicians. Good life habits, behaviour and lifestyle are important for physicians health and well being but, also, they are important since physicians have to serve as a “role model”, and previous research show that patients who struggle with the same unhealthy lifestyle habits as their doctor reported that they are more likely to follow his or her advice than patients who do not have these unhealthy lifestyle habits(3).And one of the major problems is that, although the healthy lifestyle is the mainstay of preventive medicine, many physicians lack confidence in their ability to counsel patients regarding lifestyle(2). It is well known that physicians consider advising and educating patients about diet and physical activity as part of their professional responsibility but their attempts to motivate patients are influenced by perceptions of their own effectiveness, with smoking causing the most frustration(4). This is of concern as smoking among health care professional’s limits their interventions with smokers and their involvement in tobacco control(5). Also, physicians disregard keeping a healthy diet and exercise habits for themselves, perhaps due to feeling protected by their own knowledge and sometimes under-diagnose their own overweight status and even display lower rates of healthy behaviours compared with the general population(6). Furthermore, physicians' excessive number of work hours(more than 65 hours per week) was associated with lack of exercise, not eating breakfast, and sleeping fewer than 6 hours per night(7). In the study that examined the relationship between work stressors and lifestyle-related cancer risk factors, the lifestyle-related cancer risk factors: smoking, obesity, sedentariness and alcohol consumption were documented especially among female physicians and recent findings suggest that diminishing the work stressor burden should be considered when developing intervention strategies aimed at these risk factors(8). The high level of stress among doctors, both physicians practice in private services and physicians practice in government services, has been described in the professional literature and it is likely that this fact has some implications on their work(9-15). Some of the most important sources of stress for general practitioners and hospital physicians of different specializations were identified as intrinsic factors of work, administration, stressors related to financial opportunities, contact with patients, relationships with co-workers, organizational structure and climate, and interference of private and work life(16-20).The Croatian Adult Health Surveys are conducting regularly in Croatia. The results of Croatian Adult Health Survey 2003(21) and Croatian Adult Health Survey(CAHS) 2008(22) are presented. Based on the data from Croatian Adult Health Survey 2003(21) overweight and obesity was the major public health problem in the adult population in Croatia. The likelihood of being obese, either in men or women, was more likely in the middle-aged groups, among respondents from rural areas and those from the Continental region of Croatia, with drinking lifestyle pattern, and non-smokers(21). And according to the Croatian Adult Health Survey(CAHS) 2008, risk factors for Croatian adult population were defined as an unhealthy nutritional regimen, excessive alcohol consumption, smoking and lack of physical activity(22).Also, previous results on Croatian Health care professionals attitudes towards their own health showed that, regardless of education or work; our health professionals do not have healthy life habits. Physicians were obese and physically inactive; most physicians were inclined to self treatment. Many physicians reported alcohol consumption. A vast majority of patients cite their physicians as their primary source of information regarding healthy lifestyle decisions. These findings suggest strategies to improve the physicians' health behavior(23). Life habits and personal behaviour of physicians in Croatia regarding the type of service that physicians work in are the subjects that, up to the author’s knowledge, haven’t been investigated before so this investigation is extending the investigation about healthy life style in Croatian physicians, especially with the hypothesis that type of service that physicians work in could impact their attitudes, life habits and personal behaviour.Basically, the better insight in life habits and personal behaviour of Croatian physicians is needed, especially comparing to the health surveys on Croatian population and their “target” spots for interventions which are unhealthy nutritional regimen, excessive alcohol consumption, smoking and lack of physical activity. The benefit of this study could be the need for further research on the subject, since there is a need for improvement of physician’s attitudes, life habits and behaviour. Changing attitudes towards overweight, alcohol, smoking and exercise and improving their own life habits and health behaviour could also be, for physicians, a beneficent way to improve the health of their patients serving as a “good model”.
2. Methods
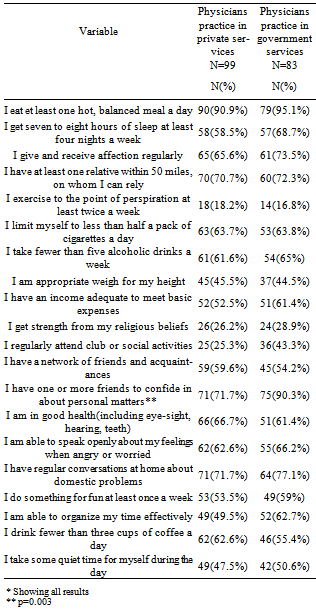
- The surveyed population was divided in two subgroups; physicians practicing in government services and physicians practicing in private services. The inclusion criterion for the subgroup of physicians practicing in private services was: practicing as physicians practicing in private services for at least one year, within the Zagreb city area. The inclusion criteria for the subgroup of physicians practicing in government services were: working as specialists in a general hospital in the city of Zagreb. An exclusion criterion for physicians practicing in private services was: working as physicians practicing in private services for less than one year. An exclusion criterion for physicians practicing in government services was: private/public mix i.e. working at hospital departments and at the same time having private practice, and less than one year of working experience. Those who agreed to participate were asked to evaluate 20 statements regarding their life habits/personal health behaviour by using a five point scale from “always to “never”. Examples of the statements asked to be assessed in the questionnaire are: “I eat at least one hot, balanced meal a day”, “I get seven to eight hours of sleep at least four nights a week”, “I exercise to the point of perspiration at least twice a week”. The whole 20 statements are submitted in the attachment. The differences between the subgroups were tested by the Chi – square test, with the level of significance at P less than 0,05. The SAS system for windows Release 8.2(SAS Institute Inc., Cary, NC, USA) was use to perform the statistical analysis(24).
3. Results
- A total number of 182 physicians(response rate 87%) responded to the questionnaire: 99 physicians practice in private services(response rate 75%) and 83 physicians practice in government services(response rate 92%). Sex and age distribution of participants is shown in table 1.
|
4. Discussion
- Since this is a small pilot study, its limitations include the small number of participants and differences in some characteristics of the two samples that could have affected the results. Only hi-squared test was done to compare the both subgroups and no significant difference was found. Future research could reveal correlations between the statements or the possible connections between the life habits of the participants and their sex and age. The study revealed a lower response rate in the study subgroup; only 75%. A study of the non-respondents was not done. A similar distribution by sex in the two subgroups is a good basis on which to draw conclusions, since there is a significant, tradition – based difference in some questions between the genders, which could have influenced the results significantly(25). It is interesting to note that 2/3 of doctors of both subgroups consider themselves “in good health(including eye-sight, hearing, teeth)”. According to the Croatian Adult Health Survey(CAHS) done in 2008, risk factors for Croatian adult population were defined as an unhealthy nutritional regimen, excessive alcohol consumption, smoking and lack of physical activity(22).It is documented that positive quality of life was associated with good physical health and mental health, regular attendance to scientific meetings, enough leisure time, and professional satisfaction(1). Good or very good physical health was independently associated with positive quality of life and mental health, higher income level, regular physical activities, and never having smoked. Positive mental health remained associated with professional satisfaction, enough leisure time, and positive evaluation of both quality of life and physical health(1).Previous results from a large cross-sectional study of health attitudes, knowledge, behaviour and risks in the post-war Croatian population(the First Croatian Health Project) in 1998(26) show that in the Croatian population, about one third of the male population smokes regularly and 6.6% of the population smokes occasionally. More than 40% of males smoke more than 20 cigarettes a day. Seventy-four percent of subjects started smoking before they were 20 years old. 6.8% of the male population drinks wine more often than four times a week.(26). Compared with self-reports from the general Canadian population, Canadian physicians, seem to have generally healthy behaviour(27). More than 90% of Canadian physicians reported being in good to excellent health, and only 5% reported that poor physical or mental health made it difficult to handle their workload more than half the time in the previous month(although a quarter had reduced work activity because of long-term health conditions). 8% were obese, 3% currently smoked cigarettes, and 1% typically consumed 5 drinks or more on days when they drank alcohol. Physicians averaged 4.7 hours of exercise per week and ate fruits and vegetables 4.8 times a day. Fifty-seven percent agreed that they had a good work-life balance, and 11% disagreed with the statement "If I can, I work when I am ill"(27).The other study, in USA showed that more than 6% screened positive for alcohol abuse and 5% for gambling problems. Thirty-five percent of participants reported "no" or "occasional" exercise. About 27% self-reported "never" or "occasionally" eating breakfast. In addition, 34% reported 6 or fewer hours of sleep daily, while 21% self-reported working more than 60 hours per week. Physicians' excessive number of work hours(more than 65 hours per week) was associated with lack of exercise, not eating breakfast, and sleeping fewer than 6 hours per night(7).In the study in Novi Sad(8), that examined the relationship between work stressors and lifestyle-related cancer risk factors: smoking, obesity, sedentariness and alcohol consumption, among 112 female physicians in Novi Sad, a region of high lifestyle-related cancer risk factors prevalence, a total of 35(31.3%) of the physicians were current smokers and 10(8.9%) were heavy smokers(>20 cigarettes/day); 23(20.5%) had a body mass index(BMI) of 28 or more, and 11(9.8%) were obese(BMI> or =30). Only 27(24.1%) regularly engaged in recreational physical activity. Slightly over 5% consumed alcohol daily. Altogether 15(13.4%) had a low lifestyle-related cancer risk profile(not a current smoker, BMI<28, regular recreational physical activity and no daily alcohol consumption). The risk factors were associated with long work hours, restricted problem-solving strategy, insufficient help with clinical difficulties and supervisory responsibility(obesity and/or sedentariness) and problems hampering patient care(smoking). The findings suggest that diminishing the work stressor burden should be considered when developing intervention strategies aimed at these risk factors(8).In this investigation, around 36% of physicians “always smoke more than half a pack of cigarettes a day”.According to the Croatian Adult Health Survey(CAHS) done in 2008 smoking was found in 14.3% participants(9).Study from Bosnia and Herzegovina indicates that almost half of Family Medicine health professionals in Bosnia and Herzegovina are smokers(28). According to the data from the 2003 and 2006/2007 Tobacco Use Supplement-Current Population in USA(29), licensed practical nurses(20.55%) and respiratory therapists(19.28%) had the highest smoking prevalence. Physicians(2.31%), dentists(3.01%), pharmacists(3.25%), and registered nurses(10.73%) had the lowest prevalence. The lack of significant decline in smoking rates among health professionals was similar to the "flat" rate seen among adults in the United States. This is of concern as smoking among health care professional’s limits their interventions with smokers and their involvement in tobacco control(5). In national survey of U.S. health professionals' smoking prevalence, cessation practices, and beliefs, health professionals have a low smoking prevalence(<6%)(30). In the study on 101 physicians and 524 nurses from the primary health centres(PHCs) and Hospital S. João in the city of Porto in Portugal(31), smoking rates of 23.1% and 13.0% were found among nurses and physicians, respectively. There was a lower proportion of smokers in primary health centres(14.5% vs. 23.9%, p = 0.014)(30). In the study in one of the biggest hospitals in Poland 26% of persons admitted that they smoked, while nearly 12% persons confirmed their addiction. Also, some factors, which determined smoking, such as a large number of duty hours, were identified(31).A previous study of smoking habits of office-based general practitioners and internists in Austria and their smoking cessation efforts showed that just fewer than 11% of doctors were smokers. About 50% of all doctors who responded described themselves as ex-smokers. 38% of the smokers would accept outside help to stop smoking. About 50% of physicians practice in private services and 90% of internists inquire about the smoking habits of their patients during history taking. Of these, 85% of physicians practice in private services and 92% of internists recommend their patients to stop smoking. Doctors who themselves are smokers do so less than their non-smoker colleagues. For this reason, a further reduction in the prevalence of smoking among doctors would be of special importance. Inquiry about smoking habits in the initial history taking should be stressed more to identify any smoker who can be subsequently encouraged to stop smoking(32).To compare the hazards of cigarette smoking in male doctors who formed their habits at different periods, and the extent of the reduction in risk when cigarette smoking is stopped at different ages, the British doctor prospective study was continued from 1951 to 2001. on 34 439 male British doctors. A substantial progressive decrease in the mortality rates among non-smokers over the past half-century(due to prevention and improved treatment of disease) has been wholly outweighed, among cigarette smokers, by a progressive increase in the smoker/ non-smoker death rate ratio due to earlier and more intensive use of cigarettes. Among the male doctors born around 1920, prolonged cigarette smoking from early adult life tripled age specific mortality rates, but cessation at age 50 halved the hazard, and cessation at age 30 avoided almost all of it(33).These findings support the need for new campaigns to reduce smoking among health care professionals and to increase their awareness of the importance of their role in reducing tobacco consumption in society.Also, use of alcoholic beverages in larger than moderate amounts presents a risk for the development of cardiovascular diseases(CVD), cancer, other chronic diseases, mental health, violence, intentional and unintentional injuries and lowers the capability for lucid decision making that proceed into involvement in other risky behaviours(34). In this study, more than 35% of doctors always drink more than five alcoholic drinks a week. According to the Croatian Adult Health Survey(CAHS) done in 2008 alcohol consumption was found in 5.8% participants(9). The highest prevalence of alcohol consumption in men was reported in Eastern Croatia(14.1%)(35). Men living in the Mountainous region had the lowest prevalence of reported alcohol consumption(8.8%). In contrast to men in the Eastern region, women in the same region reported drinking alcoholic beverages with the lowest prevalence(0.3%). The highest proportion of women who reported drinking alcoholic beverages was recorded the Northern Croatian region(1.5%)(35). In the O'Connor and Kelleher investigation alcohol was sometimes or frequently used by around half of doctors(36). Among physicians practice in private services in the process of privatisation those sensitive to stress consume more alcohol(37). Furthermore, previous research shows that alcohol consumption may be used as the main predictor of the stress level in doctors(12).To relate alcohol consumption patterns to mortality in an elderly population of doctors, a 23-year prospective study of 12 000 male British doctors aged 48-78 years was conducted in 1978, involving 7000 deaths(38). In this elderly population, with mean alcohol consumption per drinker of 2 to 3 units per day, the causes of death that are already known to be attributable to alcohol accounted for only 5% of the deaths(1% liver disease, 2% cancer of the mouth, pharynx, larynx, or oesophagus, and 2% external causes of death) and were significantly elevated only among men consuming >2 units/day. Vascular disease and respiratory disease accounted for more than half of all the deaths and were both significantly less common among current than among non-drinkers. Even so, ischemic heart disease, respiratory disease, and all-cause mortality were significantly lower than in the non-drinkers. The British doctor study concluded that although some of the apparently protective effect of alcohol against disease is art factual, some of it is real(38).But, it is very important that when analysing the results of studies on alcohol consumption one should consider the fact that people interpret the measure of “one drink” differently and there are differences in interpretation between countries as well. In Croatia the amount of “one drink” means 0.5 dcl of strong drink or 5 dcl of beer or 1 dcl of vine, while in the USA this amount is 0.3 dcl of strong drink or 3 dcl of beer or 1 dcl of vine. We assume that our investigation was conducted among doctors and who are well acquainted with these measures of dosage, however these differences can be a reason of misinterpretation of the data of recent studies in other countries and the potentially for drawing the wrong conclusions.It is well known that dietary habits as one of lifestyle factors play important role in the onset and progress of some chronic diseases. Chronic diseases, such as cardiovascular diseases and cancer, have become major causes of death worldwide. Healthy and regular diet is a major factor in the promotion and maintenance of good health throughout entire life course(39).Our study showed that a majority of physicians practice in private services and physicians practice in government services stated that they “eat et least one hot, balanced meal a day”. Although 2/3 of doctors of both subgroups stated that they consider themselves “in good health”, more than half of both subgroups consider themselves to have an inappropriate weight for their height, almost as if inappropriate weight does not mean “bad health status”. According to the Croatian Adult Health Survey(CAHS) done in 2008 unhealthy dietary pattern was found in 10% participants(9).Overweight and obesity are major public health problem in the adult population in Croatia and health promotion strategies based on behavioural correlates are needed to prevent excess weight gain in the Croatian population. Over 60% of men and 50% of women in the study had an excess body weight. The prevalence of obesity demonstrated almost the same prevalence in men and women, 20.1% and 20.6% respectively(8).Physicians report that inadequate workplace nutrition has a significant negative impact on their personal wellness and professional performance(40).According to the literature, health professionals have some knowledge of nutrition and weight management but are unclear how to deliver effective weight management advice(41). Physicians’ practices in private services think that obesity is not easy to handle in practice(42). Furthermore, some studies show that physicians practice in private services view weight management as important and feel that they have an important role to play. Although they consider themselves to be well prepared to treat overweight patients, they believe that they have limited efficacy in weight management and find it professionally unrewarding. Physicians practice in private services view the assessment of a patient's dietary and physical activity habits and the provision of dietary and physical activity advice as very important. The approaches least likely to be considered important and/or least likely to be practiced were those that would support the patient in achieving and maintaining lifestyle change(43).Although the majority of doctors from both subgroups eat a balanced meal, more than 1/3 do not get “seven to eight hours of sleep at least four nights a week”. Since data from literature shows that sleep hours matter in reducing the doctor’s stress(44), we can consider that 1/3 of doctors of both subgroups do not use sleep as a protective factor against the stress on work. Most of the doctors in both subgroups stated that they did not “exercise to the point of perspiration at least twice a week”. According to the Croatian Adult Health Survey(CAHS) done in 2008, physical inactivity was found in 44.8% participants(9).Physical activity offers major health benefits and counselling for it should be integrated into the medical consultation(45). Based on the literature, the personal health behaviour of the physician(including physical activity) is associated with his/her approach to counselling patients(45).In the O'Connor and Kelleher investigation, where three hundred Irish Medical Organization members were surveyed on health promotion and health safety issues and 42 % of them claimed to do aerobic exercise three times weekly(36). In the O'Connor and Kelleher investigation, 11.4 % of doctors were current smokers(36).In the Koprivnica-Krizevci comparative study(46) in 1998 and 2002 the smoking habits among health staff in the county was investigated on the sample of 508 persons(44%) in 1998 and 622 persons(50%) in 2002. 49(53%) of those who answered the questionnaire were doctors. The survey showed that of all employees who answered the questionnaire 34% in 1998 were smokers and 31% in 2002. The data of this research showed that the decrease of prevalence of smokers among health care workers is very slow(46). Several healthy lifestyle recommendations based on national and international guidelines suggests eating a healthy diet, and performing at least 150 minutes of aerobic exercise a week, with additional resistance exercises 2-3 times a week, will benefit all caretakers--both personally and professionally(6).Previous studies regarding psychosocial work environment showed that quantitative demands did not contribute to predicting job satisfaction but social support, control, role conflicts, role clarity and qualitative demands were the best predictors of job satisfaction(47).Regarding the result of this study that 71.7% physicians practice in private services and 90.3% physicians practice in government services have one or more friends to confide in about personal matters, it is important to recognize that almost 30% of physicians practice in private services do not have a confidential friend. On the other hand, when asked about “having a network of friends and acquaintances”, about half of the physicians practice in private services and half of the physicians practice in government services answered that they always have a network of friends, but now only about l/4 of the physicians practice in private services regularly attend club or social activities. The observed result may be related to increased professional isolation of the physicians practice in private services due to their newly established working conditions(48) and increased competition among doctors in the process of privatisation. We also may consider that some of physicians practice in private services close friends was fellow doctors(with whom they are now in competition).Data from the literature concerning the perceptions and experiences of the distribution of workload and teamwork between primary care doctors shows that equitable distribution of workload was a common concern among general practitioners in group practices. The resentment about perceived inequalities in workload places a further burden on general practices. The issue of working together warrants further support(49).Furthermore, it is already documented that physicians practice in private services have a need for support so in Australia, peer support groups were founded. Peer support groups are a mutual aid system in which the facilitator helps group members to help each other. Groups provide support, share knowledge and skills, do the ongoing education and skills development, while fostering self care(50). The small groups are empowering, confidence increasing, useful for addressing psychological and interpersonal issues at work and providing helpful recommendations based on physicians practice in private services experiences(51).Unlike their experience at work, about 2/3 of doctors from both subgroups have regular conversations at home about domestic problems and have a reliable relative within 50 miles. Also, more than 2/3 of doctors from both subgroups stated that they give and receive affection regularly and about 2/3 of them are able to speak openly about their feelings when angry or worried. Doctors from the both subgroups mostly give affection to the family and rely on relatives and close friends. Only less than 1/3 of doctors from both subgroups stated that they “get strength from their religious beliefs”. We can only assume that if the question was about recognition of prayer as an important modality in the treatment of patients, this result would be much higher, as in the literature(52), where 91% of Mississippi primary care physicians considered prayer an important treatment modality, but 50.6% rarely or never discussed prayer with their patients. Most who excluded prayer from clinical practice did so to avoid imposing their beliefs upon patients. A majority recognizes prayer, as an important psychosocial variable in assessing and treating patients, but many are hesitant to incorporate this variable into the doctor-patient encounter(53). Physicians should be aware of their own biases in discussions with patients, families, and other health care providers(53).More than half of doctors from both subgroups stated that they can “organize their time effectively”, “take some quite time for themselves during the day” or “do something for fun at least once a week”. Depending on whether one’s point of view is “that the glass of water is half empty or half full”, one can conclude that half of the physicians practice in private services can control their work conditions, organize their time and take some “time off” despite being in the process of privatisation of PHC. According to the literature, physicians practice in private services perceives that their professional position and training adversely influence their attitudes to illness in themselves and their colleagues. Organisational changes within general practice, including revalidation, must take account of barriers experienced by general practitioners in accessing health care. Medical education and culture should strive to promote appropriate self - care among doctors(54).We may also ask, how much physicians practice in private services’ own aims, values, and working conditions underlying their present attitudes and behaviour about lifestyle affects giving the lifestyle advice which they give to their patients(55).It is documented that general practitioner attitudes, normative influences from both patients and the profession, and perceived external control factors(time, cost, availability and practice capacity) all influence management of behavioural risk factors. Provider education, community awareness raising, support and capacity building may improve the uptake of lifestyle modification interventions(4). Solving the legal position of family practitioners working in "lease", introduction of the combined form of payment in family practice, and the possibility of interacting association of physicians could promote the quality of health care(56).
5. Conclusions
- The type of service that physicians work in makes no difference on their life habits and personal behaviour except that physicians in private services have significantly less confidential friends. The better insight in life habits and personal behaviour of Croatian physicians was gained from the study and “target” spots for interventions are found: attitudes and behaviour considering unhealthy nutritional regimen, excessive alcohol consumption, smoking and lack of physical activity. The benefit of this study is that it emphasizes the need for further research on the subject, since there is a need for improvement of physician’s attitudes, life habits and behaviour. Changing attitudes towards unhealthy nutritional regimen, excessive alcohol consumption, smoking and lack of physical activity could also be, for physicians, a beneficent way to improve the health of their patients serving as a “good model”.
References
| [1] | Torres AR, Ruiz T, Müller SS, Lima MC. Quality of life, physical and mental health of physicians: a self-evaluation by graduates from the Botucatu Medical School—UNESP, Rev Bras Epidemiol, vol.14, no.2,pp.264-75,2011. |
| [2] | Wendel S, Bes RE, de Jong JD, Schellevis FG, Friele RD. The fat doctor and the fat patient--can a doctor also be allowed to transgress? Ned Tijdschr Geneeskd, vol. 154,no.51-52,pp.97-99,2010. |
| [3] | Howe M, Leidel A, Krishnan SM, Weber A, Rubenfire M, Jackson EA. Patient-related diet and exercise counseling: do providers' own lifestyle habits matter? Prev Cardiol,vol. 13, no.4,pp.180-5, 2010. |
| [4] | Ampt AJ, Amoroso C, Harris MF, McKenzie SH, Rose VK, Taggart JR. Attitudes, norms and controls influencing lifestyle risk factor management in general practice, BMC Fam Pract, vol.26, no.10:pp.59,2009. |
| [5] | Sarna L, Bialous SA, Sinha K, Yang Q, Wewers ME. Are health care providers still smoking? Data from the 2003 and 2006/2007 Tobacco Use Supplement-Current Population Surveys, Nicotine Tob Res, vol.12, no.11,pp.1167-71,2010. |
| [6] | Dubnov-Raz G, Berry EM, Shemer O, Constantini NW. [Who will take care of the caretaker? Lifestyle recommendations for physicians], Harefuah, vol.150, no.7, pp.583-7,,2011. |
| [7] | Bazargan M, Makar M, Bazargan-Hejazi S, Ani C, Wolf KE. Preventive, lifestyle, and personal health behaviors among physicians, Acad Psychiatry, vol.33, no.4,pp.289-95,2009. |
| [8] | Belkić K, Nedic O. Workplace stressors and lifestyle-related cancer risk factors among female physicians: assessment using the Occupational Stress Index, J Occup Health ,vol. 49, no.1, pp.61-71,2007 |
| [9] | Magas S, Poljicanin T, Sekerija M, Ajduković D, Metelko Z, Car N, Kern J. Lifestyle habits of Croatian diabetic population: observations from the Croatian Adult Health Survey, Coll Antropol, vol 33, no.1,pp.115-9, 2009. |
| [10] | Gruber EN. Liječnici opće/obiteljske medicine i stres- pregled literature.(GPs and stress- literal review), Med Fam Croat, vol. 9, pp.59-69, 2001. |
| [11] | Bonn D, Bonn J. Work related stress: can it be a thing of the past? The Lancet, vol. 355, pp. 124-125, 2007. |
| [12] | Calnan M. Mental health and stress in the workplace: the case of general practice in the UK, Soc Sci Med, vol. 52, pp.499-507, 2001. |
| [13] | Weinberg A, Creed F. Stress and psychiatric disorder in healthcare professionals and hospital staff, The Lancet, vol. 355, pp.533-537, 2000. |
| [14] | Evans J, Lambert T, Goldacre M. GP recruitment and retention: a qualitative analysis of doctor’s comments about training for and working in general practice, Occass Pap R Coll Gen Pract, vol 83, no.iii-vi, pp.1-33, 2002. |
| [15] | Burbeck R, Coomber S, Robinson SM, Todd C. Occupational stress in consultants in accident and emergency medicine: a national survey of levels of stress at work, Emerg Med J, vol 19, pp. 234-8, 2002. |
| [16] | Glavić Ž & Majnarić A. Prvi rezultati privatizacije primarne zdravstvene zaštite na primjeru Požege.(The first results of GPs privatisation in Požega), Liječnički Vjesnik, vol. 121, pp. 70-73, 1999. |
| [17] | Jakšić Ž. Od poziva do profesije. Uvjeti za ispunjenje zadaće obiteljske medicine.(From call to profession. Conditions for being GP),Med Fam Croat, vol 4, pp.49-61, 1996. |
| [18] | Sutherland VJ, Cooper CL. Job stress, satisfaction, and mental health among GPs before and after introduction of new contract, BMJ, vol. 304, pp.1545-8, 1992. |
| [19] | Gorajščan D. Utjecaj privatizacije kao stresogenog čimbenika na liječnike opće/obiteljske medicine.(The impact of privatisation on Gps), In Proceedings of the 8-th Congress of family medicine, pp 215-30, 2000. |
| [20] | Knežević B, Golubić R, Milošević M, Matec L, Mustajbegović J. Hospital healthcare workers and stress at work: study in Zagreb [in Croatian], Sigurnost, vol. 51, pp.85-92, 2009. |
| [21] | Musić Milanović,S, Ivičević Uhernik A, Kristina Fišter, K. Health Behavior Factors Associated with Obesity in the Adult Population in Croatia,Coll. Antropol, vol 33, no.1, pp.67–73, 2009. |
| [22] | Magas S, Poljicanin T, Sekerija M, Ajduković D, Metelko Z, Car N, Kern J. Lifestyle habits of Croatian diabetic population: observations from the Croatian Adult Health Survey, Coll Antropol, vol 33, no.1,pp.115-9, 2009 |
| [23] | Kumbrija S, Milaković SB, Jelinić JD, Matanić D, Marković BB, Simunović R. Health care professionals--attitudes towards their own health. Acta Med Croatica. Feb;61(1):105-10, 2007. |
| [24] | SAS Institute Inc. SAS/STAT Users Guide, Release 6, 03 Edition. Cary NC: SAS Institute INC 1988. |
| [25] | Boerma WG & Van den Brink-Muinen A. Gender-related differences in the organization and provision of services among general practitioners in Europe: a signal to health care planners,Med Care, vol 38, no. 10, pp.993-1002, 2000. |
| [26] | Turek S, Rudan I, Smolej-Narancic N, Szirovicza L, Cubrilo-Turek M, Zerjavic-Hrabak V, Rak-Kaic A, Vrhovski-Hebrang D, Prebeg Z, Ljubicic M, Janicijevic B, Rudan P. A large cross-sectional study of health attitudes, knowledge, behaviour and risks in the Post-war Croatian population. The first Croatian health project,Coll. Antropol, vol. 25, no.1, pp. 77-96, 2001. |
| [27] | Frank E, Segura C. Health practices of Canadian physicians. Can Fam Physician, vol. 55, no.8, pp. 810-811, 2009. |
| [28] | Hodgetts G, Broers T , Godwin M. Smoking behaviour, knowledge and attitudes among Family Medicine physicians and nurses in Bosnia and Herzegovina. BMC Family Practice vol. 5, pp.12-14, 2004. |
| [29] | Tong EK, Strouse R, Hall J, Kovac M, Schroeder SA. National survey of U.S. health professionals' smoking prevalence, cessation practices, and beliefs, Nicotine Tob Res ,vol.12, no.7, pp.724-33, 2010. |
| [30] | Ramos MC, Vinagre S, Cardoso MF. Knowledge, behavior and ethical responsibility of health professionals with regard to smoking, Rev Port Cardiol, vol. 29, no.6, pp.923-46, 2010. |
| [31] | Cofta S, Staszewski R. Hospital staff and smoking habits: do we need modification of smoking behavior in Polish hospitals? J Physiol Pharmacol, vol 59, no. 6, pp. 191-9, 2008. |
| [32] | Kossler W, Lanzenberger M & Zwick H: Smoking habits of office-based general practitioners and internists in Austria and their smoking cessation efforts, Wien Klin Wochenschr, vol. 30, no. 114, pp. 762-5, 2002. |
| [33] | Jacobsen ET, Rasmussen SR, Christensen M, Engberg M & Lauritzen T. Perspectives on lifestyle intervention: the views of general practitioners who have taken part in a health promotion study. Scand J Public Health, vol 33., no. 1, pp. 4-10, 2005. |
| [34] | WORLD HEALTH ORGANIZATION. Strategies to reduce the harmful use of alcohol, report by the secretariat. A61/13 Provisional agenda item 11.10 20 March 2008, accessed: 09.02.2012. Online Available: http://www.who.int/gb/ebwha/ pdf_files/A61/A61_13-en.pdf. |
| [35] | Benčević-Striehl H, Malatestinić D, Vuletić S. Regional Differences in Alcohol Consumption in Croatia Coll. Antropol, vol. 33, no. 1, pp. 39–41, 2009. |
| [36] | O Connor M & Kelleher C: Do doctors benefit from their profession? - A survey of medical practitioners health promotion and health safety practices(editorial). Dept. Of Health Promotion, National University of Ireland, Galway, Ir Med J, vol. 91, pp. 206-9, 1998. |
| [37] | Golik-Gruber V., Gruber E.N., Marušić S., Breitenfeld D & Gorajščan D: Sensitivity to Stress and the Consumption of Alcoholic Drinks Among Doctors in the Process of Privatisation, Alcoholism, vol. 36, no. 2, pp.131-138, 2000. |
| [38] | Doll R, Peto R, Boreham J & Sutherland I. Mortality in relation to alcohol consumption: a prospective study among male British doctors, Int J Epidemiol, vol. 34, no. 1, pp.199-204, 2005. |
| [39] | WORLD HEALTH ORGANIZATION, Diet, nutrition and the prevention of chronic diseases. WHO Tech Rep, Geneva, 2003. |
| [40] | Lemaire JB, Wallace JE, Dinsmore K, Roberts D. Food for thought: an exploratory study of how physicians experience poor workplace nutrition Lemaire et al. Nutrition Journal 2011, Online Available: http://www.nutritionj.com/content/ 10/1/18 |
| [41] | Hankey CR, Eley S, Leslie WS, Hunter CM & Lean ME: Eating habits, beliefs, attitudes and knowledge among health professionals regarding the links between obesity, nutrition and health, Public Health Nutr, vol 7, no. 2, pp.337-43, 2004. |
| [42] | Brotons C, Ciurana R, Pineiro R, Kloppe P, Godycki-Cwirko M, Sammut MR:Dietary advice in clinical practice: the views of general practitioners in Europe, Am J Clin Nutr, vol. 77, no. 4, pp. 1048S-1051S, 2003. |
| [43] | Campbell K, Engel H, Timperio A, Cooper C & Crawford D: Obesity management: Australian general practitioners' attitudes and practices, Obes Res, vol.8, no.6, pp.459-66, 2000. |
| [44] | Firth-Cozens J & Moss F: Hours, sleep, teamwork, and stress. Sleep and teamwork matter as much as hours in reducing doctors stress, BMJ, vol.317, pp.1335-6,1998. |
| [45] | Suija K, Pechter U, Maaroos J, Kalda R, Rätsep A, Oona M, Maaroos HI. Physical activity of Estonian family doctors and their counseling for a healthy lifestyle: a cross-sectional study, BMC Fam Pract, vol 18. no. 11, pp. 45-48, 2010. |
| [46] | Gazdek D & Kovacic L: Smoking habits among health staff in the county of Koprivnica-Krizevci--comparative study 1998 and 2002, Lijec Vjesn, vol. 126, no. 1, pp.6-10., 2004. |
| [47] | Jönsson S. Psychosocial work environment and prediction of job satisfaction among Swedish registered nurses and physicians - a follow-up study, Scand J Caring Sci, vol.19, pp. 45-49, 2011. |
| [48] | Gruber EN. “Dinamika stresa i promjene radnog mjesta liječnika opće/obiteljske medicine u Hrvatskoj”.(“Dynamic of stress and change in working conditions of GPs in Croatia”), M. thesis, Mathemathic faculty, Croatian Institute of Science, Croatia, 2002. |
| [49] | Branson R & Armstrong D: General practitioners' perceptions of sharing workload in group practices: qualitative study. BMJ 2004;14;329(7462):381. |
| [50] | Wilson I, Howell C. Small group peer support for GPs treating mental health problems. Aust Fam Physician, vol. 33, no.5, pp.362-4, 2004. |
| [51] | Wilhelm K, Peel G, Sutton V, Finch A, Sved-Williams A. Small groups for supporting GPs' professional development in mental health disease--an evaluation, Aust Fam Physician , vol.34, no. 9, pp.791-4, 2005. |
| [52] | Wilson K, Lipscomb LD, Ward K, Replogle WH & Hill K: Prayer in medicine: a survey of primary care physicians, J Miss State Med Assoc, vol. 41, no. 12, pp.817-22, 2000. |
| [53] | Neumann JK & Olive KE: Absolute versus relative values: effects on family practitioners and psychiatrists, South Med J, vol 96, no. 5, pp. 452-7, 2003. |
| [54] | Thompson WT, Cupples ME, Sibbett CH, Skan DI & Bradley T: Challenge of culture, conscience, and contract to general practitioners' care of their own health: qualitative study. BMJ, vol. 323,no. 7315, pp.728-31, 2001. |
| [55] | Jacobsen ET, Rasmussen SR, Christensen M, Engberg M & Lauritzen T. Perspectives on lifestyle intervention: the views of general practitioners who have taken part in a health promotion study. Scand J Public Health, vol. 33, no. 1, pp.4-10, 2005. |
| [56] | Marković BB, Katić M, Milaković SB, Petric D. Ten years after "privatization" in primary health care, Acta Med Croatica, vol .61, no.1, pp. 1-6, 2007. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-Text HTML
Full-Text HTML