-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Otolaryngology
p-ISSN: 2326-1307 e-ISSN: 2326-1323
2020; 9(1): 1-3
doi:10.5923/j.otolaryn.20200901.01

Eagle’s Syndrome: A Case Report
Lyra Joy, Ramappa Arabhanvi, B. Viswanatha
Department of ENT, Bangalore Medical College & Research Institute, Bangalore, India
Correspondence to: B. Viswanatha, Department of ENT, Bangalore Medical College & Research Institute, Bangalore, India.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Eagle’s syndrome is the abnormal length of the styloid process due to its calcification. Symptoms include throat pain, foreign body sensation, voice changes, dysphagia and facial paresthesia. The diagnosis of eagle’s syndrome (ES) can be made by palpating the calcified styloid process in the tonsillar fossa. Imaging techniques like computed tomographic imaging confirms the diagnosis. Eagle’s syndrome can be managed medically with, nonsteroidal anti-inflammatory drugs and steroids or by intraoral or extra oral surgical techniques.
Keywords: Eagles syndrome, Styloid process
Cite this paper: Lyra Joy, Ramappa Arabhanvi, B. Viswanatha, Eagle’s Syndrome: A Case Report, Research in Otolaryngology, Vol. 9 No. 1, 2020, pp. 1-3. doi: 10.5923/j.otolaryn.20200901.01.
1. Introduction
- Eagle’s syndrome is a rare condition in which the elongated styloid process or calcified stylohyoid ligament causes recurrent throat pain, foreign body sensation, dysphagia, or facial pain.[1] The other associated symptoms include painful neck movements, pharyngeal discomfort, otalgia, headache, syncope, tinnitus and focal cerebral symptoms.[2] A styloid process greater than 2.5cm should be considered abnormal however an elongated styloid process in association with symptoms can confirm the syndrome.[3] The etiology and pathophysiology of the syndrome are poorly understood. It can be confused with oropharyngeal and maxillofacial disorders and particularly with cranial neuralgia, but with appropriate clinical history and radiography, it can be easily identified and treated. [4]
2. Case Report
- 30-year-old female patient presented to the OPD with a complaint of pain in upper neck region of six months duration. The pain was insidious in origin, dull to moderate in intensity and intermittent in nature. The intensity of pain was exacerbated by movements such as looking up and turning face to left side. In addition, patient also had a sensation of foreign body in throat on swallowing. No history of neck trauma.On intraoral palpation of bilateral tonsillar fossa, tenderness was elicited. Radiographic examination (Mandibular lateral oblique {ramus view} – Orthopantomogram) demonstrated elongated styloid process. CT neck confirmed the diagnosis of elongated styloids measuring 33.6mm on left side and 37.6mm on right side approximately (Fig 1). Subsequent to the radiographic findings re-examination of the patient revealed a hard bony mass which was palpated bilaterally in the tonsillar fossa. The patient was given a primary diagnosis of ES. The patient underwent a chair side infiltration of 2% lignocaine bilaterally in the tonsillar fossa which led to immediate relief from the symptoms.
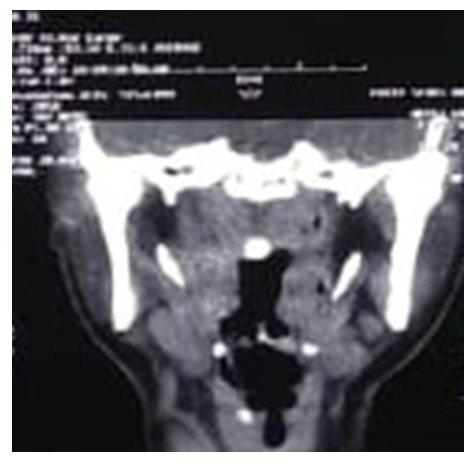 | Figure 1. CT Showing elongated styloid in both sides |
 | Figure 2. Intraoral technique and styloid dissected out from the fossa |
 | Figure 3. Bilaterally excised styloid process |
3. Discussion
- The styloid process is a slender outgrowth at the base of the skull in the temporal bone, immediately posteromedial to the mastoid apex, arising from the inferior surface of the temporal bone at the junction of its petrous and tympanic portions. Lies posterior to the tonsillar and lateral to the pharyngeal wall. It is in close proximity to glossopharyngeal, hypoglossal and facial nerves and to the internal and external carotid artery. [5]The styloid process with its 5 attachments is called the styloid apparatus. Stylohyoid and stylohyoid ligament, both of which derived from reichert’s cartilage of 2nd arch, stylomandibular ligament-part of deep fascia, styloglossus-from occipital myotomes, stylopharyngeus-from third arch. [5]Normal length is 2.5 cm and is considered to be elongated if longer than 3 cm. Eagle Syndrome is a rare and poorly understood condition that presents with a myriad of symptoms that typically include pain in the anterolateral neck. Etiopathogenesis is ascribed to elongation of the styloid process or calcification of the stylohyoid ligament. First described by Watt W. Eagle in 1937. The first description in humans was published by Marchetti in 1656. [6]Etiology proposed were surgical trauma or chronic local irritation can cause osteitis, periosteitis or tendinitis of the styloid apparatus, osseus metaplasia of mesenchymal elements as a consequence of trauma, related to endocrine disorders in women at menopause associated with ossification of ligaments elsewhere and ectopic calcification in disorders of calcium metabolism.Eagle considered tonsillectomy responsible for the formation of scar tissue around styloid apex causing stretching of the vascular and nervous structures as the cause for pain. Other causes were contracture of stylopharyngeus, fracture of ossified stylohyoid ligament with incomplete repair, ossification of muscular tendons causing irritation of structures nearby and abnormal angulation of styloid process. [7]The classic Eagle syndrome, typically seen in patients after tonsillectomy, characterised by ipsilateral dull and persistent pharyngeal pain, centered in the ipsilateral tonsillar fossa that can be referred to the ear and exacerbated by rotation of the head. Bony projection can be palpated in the ipsilateral tonsillar fossa. The pathophysiological mechanisms for the pain of elongated styloid process include:(1) Compression of the neural elements, the glossopharyngeal nerve, lower branch of the trigeminal nerve, and/or the chorda tympani by the elongated styloid process;(2) Fracture of the ossified stylohyoid ligament, followed by proliferation of granulation tissue that causes pressure on surrounding structures and results in pain;(3) Impingement on the carotid vessels by the styloid process, producing irritation of the sympathetic nerves in the arterial sheath;(4) Degenerative and inflammatory changes in the tendinous portion of the stylohyoid insertion, a condition called insertion tendinosis;(5) Irritation of the pharyngeal mucosa by direct compression by the styloid process;(6) Stretching and fibrosis involving the fifth, seventh, ninth, and tenth cranial nerves in the post-tonsillectomy period. [8]Other symptoms include dysphagia, foreign body sensation, and tinnitus or cervicofacial pain. Pain maybe referred to the ear/jaw. Chang et al described a patient with Horner’s syndrome as a consequence of an elongated styloid process. Many reports of transient ischemic attacks and stroke associated with Eagle syndrome and also associated with carotid artery dissection and carotid artery stent fracture. Case report of dysphonia has being associated with an elongated styloid.The “stylocarotid syndrome”- compression of internal or external carotid artery, with their perivascular sympathetic fibers by a laterally or medially deviated styloid process. Pain along the distribution of the artery, worsens with head movements, radiated to parietal and infraorbital regions, correlates with episodes of syncope. [9]The diagnosis of ES must be based on a good medical history and physical examination (Pharyngeal palpation within the tonsillar fossa). The relief of symptoms after injection of 2% lignocaine into the anterior pillar and tonsillar fossa can be used as a diagnostic tool. Imaging techniques include Orthopantomogram, Lateral view radiographs of skull and 3D CT (Cone beam CT) is considered as gold standard as it allows surgeon to evaluate the exact morphology and its relationship with adjacent anatomical structures. [10]The elongated styloid process syndrome can be treated conservatively or surgically. Conservative treatment options have included transpharyngeal injection of steroids and lignocaine, nonsteroidal anti-inflammatory drugs, diazepam, the application of heat.The most satisfactory and effective treatment is surgical shortening of the styloid process through either an intraoral or external approach.Intraoral approach is said to be preferred given the decreased morbidity, adequate exposure, and decreased operative time. Previously, this approach was accompanied routinely with tonsillectomy. Recent interest in tonsillectomy sparing approaches has also been described. If tonsillectomy is undertaken, access to the styloid process is accomplished through the tonsillar fossa, after which dissection continues through the superior constrictor muscle. The styloid process can be adequately identified and resected; however, exposure to the skull base may be limited.The trans-cervical approach utilizes the initial steps of a parotidectomy, including separation of the sternocleidomastoid muscle from the parotid fascia followed by identification of the posterior belly of the digastric muscle. The space between the parotid gland and digastric is further explored to isolate the styloid process prior to resection. While some have believed the cervical approach allows for superior access to the styloid process up to the skull base and improved vascular control, the presence of a cervical incision and the potential risk of facial nerve injury are avoidable shortcomings to this approach. [11,12]Prognosis of ES is determined by the successfulness of surgery. Intraoperative injury, subsequent fibrous entrapment syndrome, or inadequate shortening of the process can result in poor prognosis.
4. Conclusions
- The elongated styloid process syndrome can be diagnosed by a detailed history, physical examination, and radiological investigations.It can be confused or mistaken for many other conditions that must be excluded. Resection of the elongated styloid process is the treatment of choice.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML